Author: Geoff Comp DO, FAWM (@gbcomp, EM Resident Physician, Doctors Hospital / OhioHealth) // Edited by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
Case 1:
You are working in the middle of a busy shift in the dead of winter, when a 52 y/o male is brought in by EMS. They report he was stranded in his hunting tree stand in a blizzard. They were able to passively rewarm him in the ambulance, but he has very erythematous fingers with distal duskiness. What is your next step?
Cold related injury can be broadly divided into freezing and non-freezing conditions based on their clinical presentation and the degree of injury. Frostbite is the major injury involving tissue freezing. Non-freezing injuries include frostnip, chilblains/pernio, immersion or “trench” foot, and cold urticaria. Treatment is usually supportive, with recognition and prevention as major goals of therapy. The development of these conditions depends on many factors including duration of exposure, ambient temperature, alcohol consumption, degree of protective clothing, and physical activity level. Chronic medical conditions that result in peripheral vascular disease and neuropathy including atherosclerosis and diabetes mellitus also play a role in the development of cold injury.1
Frostbite
Frostbite is a freezing injury that occurs when tissues are exposed to temperatures below their freezing point, resulting in direct ice crystal formation and cellular lysis with microvascular occlusion.2,3 Most of the damage from frostbite occurs as a result of a freeze thaw cycle with endothelial damage and cellular death resulting in osmotic gradient changes, initiation of the arachidonic acid cascade, vasoconstriction, and hematologic abnormalities including thrombosis.4 The severity of irreversible damage is most closely related to ambient temperature and length of time the tissue remains frozen.1 The handhands, feet, ears, nose, and cheeks are the most common locations.5
History, Physical Exam, and Testing:
The diagnosis of frostbite is based on history and physical exam. Important historical information to obtain includes:
– Time of injury
– Environmental factors including temperature, wind, or precipitation
– Type of clothing worn
– Level of physical activity
– Pre-hospital treatment or management
– Associated use of recreational drugs, alcohol, or tobacco
– Associated trauma or medical illness.6
Favorable prognostic indicators on physical exam are sensation to pinprick, normal skin color, and large blisters with clear fluid. Non-blanching cyanosis, dark fluid-filled blisters, and hard, non-deforming skin are concerning for a poor prognosis.5 While the initial diagnosis of the condition is clinical, various radiologic techniques can be used to help determine extent of injury. Digital subtraction angiography and multiphase bone scintigraphy have both been proposed to determine the precise anatomic localization of the level and depth of tissue necrosis aiding in potential surgical staging and monitoring of treatment.7
Frostbite is classically categorized into four levels of injury:4,8
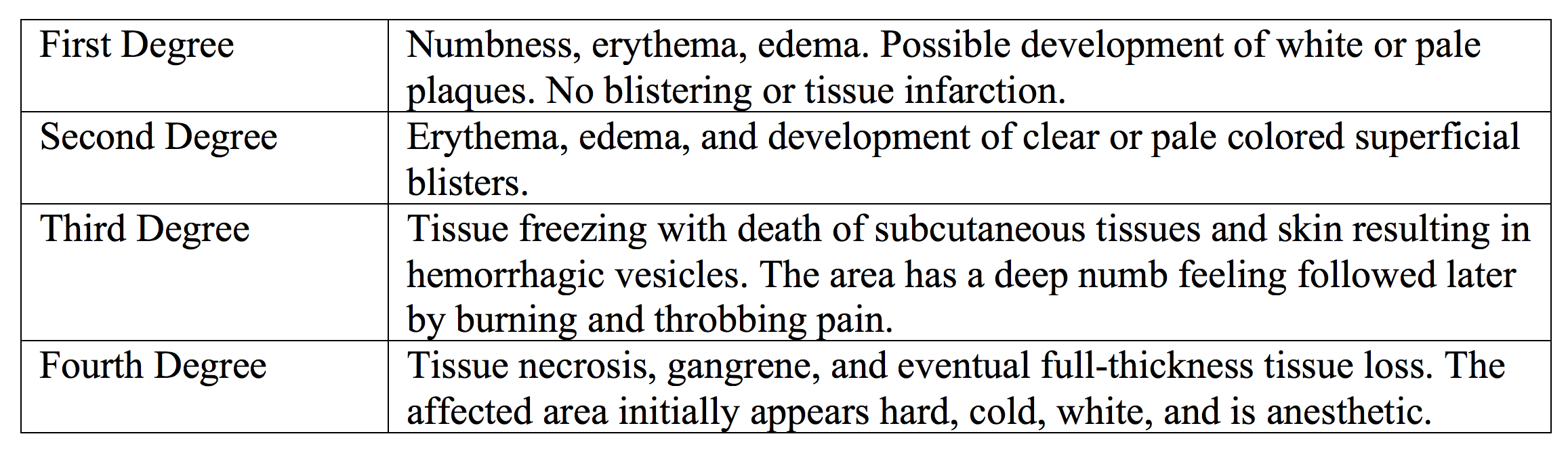

However, the appearance of the injury changes frequently during the course of treatment, ranging from the reversible changes after rewarming to permanent cellular destruction. It is difficult to correctly identify final extent of tissue destruction at first evaluation, and some authorities simply classify frostbite as either superficial or deep.1,3
Treatment:
The initial treatment in the Emergency Department for all degrees of frostbite is the same. Addressing ABC’s, trauma evaluation, removing wet and constrictive clothing, treatment of concomitant hypothermia, and identification of other injuries should be confirmed in all cold injury cases if warranted.3 The decision to initiate active rewarming in a prehospital environment depends on the possibility of continued cold injury to the area, as thaw and refreeze cycles can cause additional cellular injury. It is better to keep the affected part frozen until a thawed state can be maintained.8
Active rewarming is best performed in a circulating water bath around 37°C to 39°C. Frostbitten faces can be thawed using warm water compresses, and ears may be thawed with small bowls of warm water.6 Thermal injuries can occur when rewarming is performed with an uncontrollable heat source outside a monitored temperature range. Immersion rewarming can be discontinued when the affected area developed a red or purple appearance and becomes pliable to the touch.1 Gently dry, elevate, and apply bulky dressing to the affected area. The rewarming process is incredibly painful, and symptomatic treatment including aggressive pain control should be initiated early. Tetanus status should be determined and updated as needed. Empiric prophylactic antibiotics are not needed. Scheduled NSAIDs are recommended for both pain and inflammatory control.2 Blister treatment is controversial. Common practice is to selectively drain clear blisters with needle aspiration to reduce tissue exposure to thromboxane and prostaglandin rich fluid, while leaving hemorrhagic blisters intact to prevent desiccation.6,8 Early involvement with your burn surgeon about blister treatment is important to guide clinical course.
Surgical management including debridement and amputation is reserved for late frostbite management after the rewarming phase in days to weeks. However, escharotomy/fasciotomy or initial debridement is warranted if there are signs of compartment syndrome or significant concomitant infection not responsive to antibiotic therapy.5 There is gradual demarcation of the injured area and delineation of non-viable tissue over time. Early surgical intervention is avoided as the permanent tissue loss is often much less than originally suspected.3
New Ideas in Treatment:
Additional adjuvant treatments are currently under study. The use of IV or intra-arterial TPA has been suggested to attempt to limit damage caused by microvascular thrombosis in frostbite.2 TPA may partially or completely restore blood flow to non-perfused digits reducing the amount of amputation.9,10 However, studies are limited. Current recommendations are to consider TPA for severe frostbite injury within 24 hours of the initiation of rewarming and weigh bleeding risks against potential benefit.4,8 Hyperbaric treatment is also being explored as a treatment to improve symptoms. This is based on extrapolation of mechanism of action, case reports, and animal models, and more information is needed.11 Others recommend vasodilators, or sympathetic blockade including sympathectomy, to improve vasodilation and local blood flow. However, no prospective, randomized trials are available, and the results of the isolated reports show mixed results.3
Disposition and Further Management:
After the initial ED management of frostbite, it is best to be conservative when determining disposition including recognition of social and concomitant medical issues. Patients unable to care for themselves adequately should never be discharged into subfreezing temperatures. Consultation with the surgical team is also warranted for significant injury or concerning features. If injury is minor, shared decision making may be utilized. Patients must be provided with sufficient guidelines for self-care including outlining cold injury prevention strategies. They must also receive clear instructions for close short-term and long-term follow-up.6
Case 1 Conclusion:
You have been able to slowly rewarm your patient’s fingers and will admit him to the burn unit for further evaluation and staging.
The Bottom Line: Frostbite Evaluation and Treatment
- ABC’s, then treat hypothermia or serious trauma.
- Rewarm in water heated and maintained between 37-39°C for approximately 30 minutes until the area becomes soft and pliable to the touch.
- Pain medication including scheduled NSAIDs
- Tetanus prophylaxis.
- Selectively drain by needle aspiration clear blisters and leave hemorrhagic blisters intact.
- Dry, bulky dressings and elevate the affected body part if possible.
- Early consultation with surgical team to discuss TPA for deep frostbite if less than 24 hours after thawing, as well as additional strategies for definitive management.
Case 2:
Your next chart is a homeless man complaining of foot pain. He has also been out in the cold but reports he didn’t recognize any problems until he took off his wet shoes for the first time in 2 weeks.
Immersion Foot/Trench Foot
Trench foot is a direct soft tissue injury due to prolonged wet conditions in above freezing temperatures. This exposure causes skin breakdown and prolonged alternating vasoconstriction and vasodilation resulting in direct injury to local nerves and vessels. During the initial phase the foot appears pale, mottled, and numb with no pain. The rewarmed or “hyperemic” stage is associated with burning pain, erythematous skin, and painful swelling. There is also occasional marked hyperalgesia to light touch.12 Chronic symptoms may include hyperhidrosis, as well as a dull ache, and decreased sensation due to nerve damage. The treatment of immersion foot is dry rewarming and general supportive care.13 There is no role for prophylactic antibiotics, but instruct the patient on specific signs and symptoms to monitor for infection. Prevention is key; make sure to instruct the patient to keep their feet warm and dry with good socks and dry shoes.6
Chilblains/Pernio
Pernio, or Chilblains, is a nonfreezing cold related injury characterized initially by localized tingling and numbness followed by the development of erythematous, purplish, edematous lesions, with vesicles in severe cases.6 This cutaneous inflammatory process is caused by prolonged cold-induced vasoconstriction with subsequent hypoxemia  and vessel wall ischemia.12 These lesions occur most commonly on the hands, feet, and ears, with symptoms including intense tenderness, pruritus, burning, and numbness.14 They are self-limited and usually resolve within a few days to 3 weeks. However, patients may develop chronic residual hyperpigmentation. First-line treatment is conservative management with drying, passive slow rewarming, smoking cessation, and topical steroids for severe cases. Other proposed treatments include calcium channel blockers, immunosuppressive agents, aspirin, and nitroglycerine ointments, but more information is needed to clarify benefit, and there are not universally accepted medication options for treatment.12
and vessel wall ischemia.12 These lesions occur most commonly on the hands, feet, and ears, with symptoms including intense tenderness, pruritus, burning, and numbness.14 They are self-limited and usually resolve within a few days to 3 weeks. However, patients may develop chronic residual hyperpigmentation. First-line treatment is conservative management with drying, passive slow rewarming, smoking cessation, and topical steroids for severe cases. Other proposed treatments include calcium channel blockers, immunosuppressive agents, aspirin, and nitroglycerine ointments, but more information is needed to clarify benefit, and there are not universally accepted medication options for treatment.12
Frostnip
Frostnip is essentially “pre-frostbite.” This is a superficial non-freezing injury associated with vasoconstriction with the development of frost on exposed skin. Intracellular ice crystals do not form in the tissue, and there is no tissue loss or necrosis.8 The injury is reversible, and rewarming will result in return of sensation to the affected area.3
Cold Urticaria
Cold urticaria is a hypersensitivity reaction characterized by the development of a rash and hive-like lesions after cold exposure. Symptoms can vary from rapidly resolving mild localized urticarial rash or wheals to angioedema and anaphylaxis.15 Symptoms are usually limited to cold-exposed skin areas, however, swimming in cold water is the most common trigger of severe reactions. The treatment of this condition includes antihistamines as well as traditional anaphylaxis management if needed.12
Case 2 Conclusion:
You are able to warm and dry your patient’s feet. He is provided with clean warm socks and shoes and is able to go directly to a shelter for the evening.
The Bottom Line: Other cold related injuries
- Make sure to keep in mind other cold injuries when dealing with a hypothermic patient.
- Gentle rewarming is always a great option.
- Early consultation with surgical or burn colleagues will assist in care guidance and local protocol management.
- Keep in mind other types of non-freezing injury and make sure to council your patients on self-care.
For additional information on accidental hypothermia recognition and management, see these other articles on EMDocs:
http://www.emdocs.net/em3am-hypothermia/
http://www.emdocs.net/hypothermia-and-drowning-pearls/
This post is sponsored by www.ERdocFinder.com, a supporter of FOAM and medical education, who with their sponsorship are making FOAM material more accessible to emergency physicians around the world.
Further Reading/References:
- Petrone, Patrizio, et al. “Management of Accidental Hypothermia and Cold Injury.” Current Problems in Surgery, vol. 51, no. 10, 2014, pp. 417–431.
- Handford, Charles, et al. “Frostbite.” Emergency Medicine Clinics of North America, vol. 35, no. 2, 2017, pp. 281–299.
- Jurkovich, Gregory J. “Environmental Cold-Induced Injury.” Surgical Clinics of North America, vol. 87, no. 1, 2007, pp. 247–267.
- Freer, Luanne, et al. “Frostbite.” Auerbach’s Wilderness Medicine, by Paul S. Auerbach et al., 7th ed., Elsevier, 2017, pp. 197–222.
- Murphy, James V., et al. “Frostbite: Pathogenesis and Treatment.” The Journal of Trauma: Injury, Infection, and Critical Care, vol. 48, no. 1, Jan. 2000, pp. 171–178.
- Michael, T. Paddock. “Cold Injuries.” Tintinalli’s Emergency Medicine: a Comprehensive Study Guide, by Judith E. Tintinalli et al., 8th ed., McGraw-Hill Education, 2016.
- Millet, John D., et al. “Frostbite: Spectrum of Imaging Findings and Guidelines for Management.” RadioGraphics, vol. 36, no. 7, 2016, pp. 2154–2169.
- Mcintosh, Scott E., et al. “Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Frostbite.” Wilderness & Environmental Medicine, vol. 22, no. 2, 2011, pp. 156–166.
- Bruen, Kevin J., et al. “Reduction of the Incidence of Amputation in Frostbite Injury With Thrombolytic Therapy.” Archives of Surgery, vol. 142, no. 6, 2007, pp. 546–553.
- Gonzaga, Teresa, et al. “Use of Intra-Arterial Thrombolytic Therapy for Acute Treatment of Frostbite in 62 Patients with Review of Thrombolytic Therapy in Frostbite.” Journal of Burn Care & Research, vol. 37, no. 4, 2016, pp. 323–334.
- Kemper, Tom C.P.M., et al. “Frostbite of Both First Digits of the Foot Treated with Delayed Hyperbaric Oxygen: A Case Report and Review of Literature.” Undersea and Hyperbaric Medicine, vol. 41, no. 1, 2014, pp. 65–70.
- Handford, Charles, et al. “Nonfreezing Cold-Induced Injuries.” Auerbach’s Wilderness Medicine, by Paul S. Auerbach et al., 7th ed., Elsevier, 2017, pp. 222–234.
- Olson, Zachary, and Nicholas Kman. “Immersion Foot: A Case Report.” The Journal of Emergency Medicine, vol. 49, no. 2, 2015, pp. 45–48.
- Cappel, Jonathan A., and David A. Wetter. “Clinical Characteristics, Etiologic Associations, Laboratory Findings, Treatment, and Proposal of Diagnostic Criteria of Pernio (Chilblains) in a Series of 104 Patients at Mayo Clinic, 2000 to 2011.” Mayo Clinic Proceedings, vol. 89, no. 2, 2014, pp. 207–215.
- Hochstadter, E. F., and M. Ben-Shoshan. “Cold-Induced Urticaria: Challenges in Diagnosis and Management.” BMJ Case Reports, vol. 2013, 2013.










1 thought on “Brrr! ED Presentation, Evaluation, and Management of Cold Related Injuries”
Pingback: REBEL Core Cast 48.0 Frostbite - REBEL EM - Emergency Medicine Blog