Originally published at CoreEM.net, dedicated to bringing Emergency Providers all things core content Emergency Medicine available to anyone, anywhere, anytime. Reposted with permission.
Written by Trudi Cloyd, MD and edited by Dr. Tim Greene and Dr. Swaminathan. Follow Dr. Swaminathan and CORE EM on twitter at @EMSwami and @Core_EM
Definition
- Fracture of the articular portion of the proximal tibia

Tibial Plateau Fracture – Schatzker Type VI (radrounds.com)
Mechanism
- Axial load combined with varus (inward angulating) or valgus (outward angulating) force on weight bearing knee.
- Lateral plateau fractures more common than medial (involved in 85-90% cases) (Schwartz, 2008). The medial plateau is stronger as it bears the majority of the load transferred across the knee.
- Medial plateau fractures generally result from a high-energy mechanism
- Pedestrian struck against fixed knee, classically described as “bumper fracture” or “fender fracture” of lateral plateau
Epidemiology
- Low-energy mechanisms (e.g. simple fall, stepping awkwardly off bus) more common in elderly female patients with underlying osteopenic bone typically result in depressed fractures (Cole, 2009)
- High-energy mechanism (falls, sports-related injuries or motor vehicle accidents (MVAs)) are more common in younger patients
- Frequently missed fracture due to subtle radiographic findings
Presentation + Initial Evaluation
- Refusal to bear weight on the affected extremity
- Presence of a knee effusion
- Evaluate for compartment syndrome particularly in those with a high-energy mechanism injury (high-speed MVC, fall from height etc)
- Evaluate for neurovascular injury (popliteal artery, peroneal nerve) which may be seen if there was concomitant knee dislocation spontaneously reduced

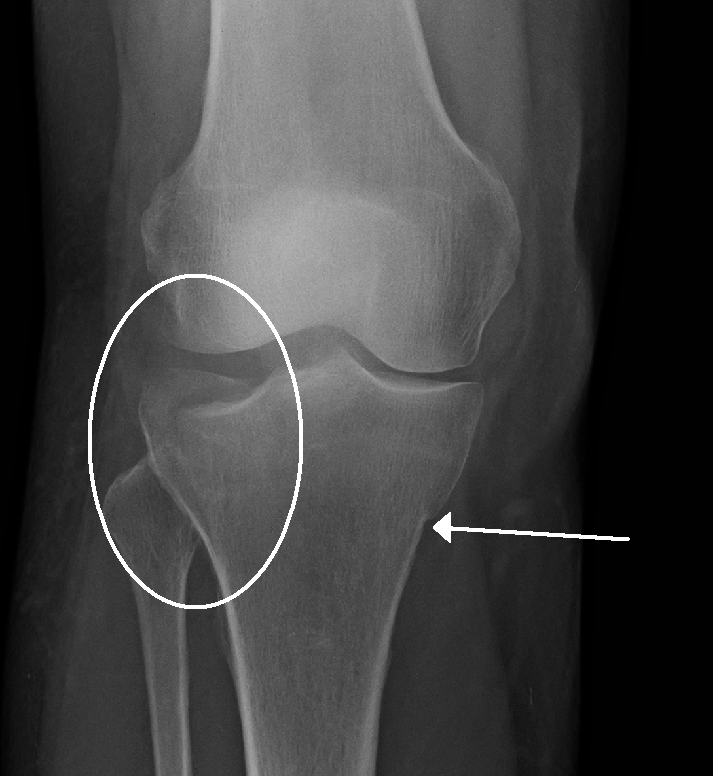
Medial Tibial Plateau Fracture (Case courtesy of RMH Core Conditions, Radiopaedia.org. From the case rID: 33626)
Imaging
- X-ray
- Views: AP, lateral and oblique views
- Fractures can be subtle as slope of tibial plateau makes accurate assessment of depression difficult on AP view
- Increased trabecular density may represent compression fracture (see image B)
- Joint widening is not reliable sign in standard AP because it requires a weight bearing view which should not be attempted if this injury is suspected
- Knee effusions and lipohemarthrosis (fat-fluid level), although non-specific, may indicate underlying bony injury. The latter is seen best on cross-table lateral view when the beam is tangential to the fat-blood interface.
- CT Scan
- May be necessary for fracture diagnosis in the ED, especially if clinical suspicion persists despite negative x-rays.
- Frequently required for further characterization of fracture pattern and evaluation of involvement of articular surface, as well as preoperative planning.
- MRI
- Typically not necessary in ED management
- May be scheduled as part of follow up evaluation for meniscal and ligamentous injury or for identification of occult fractures
Tibial Plateau Fracture (Schatzker VI)
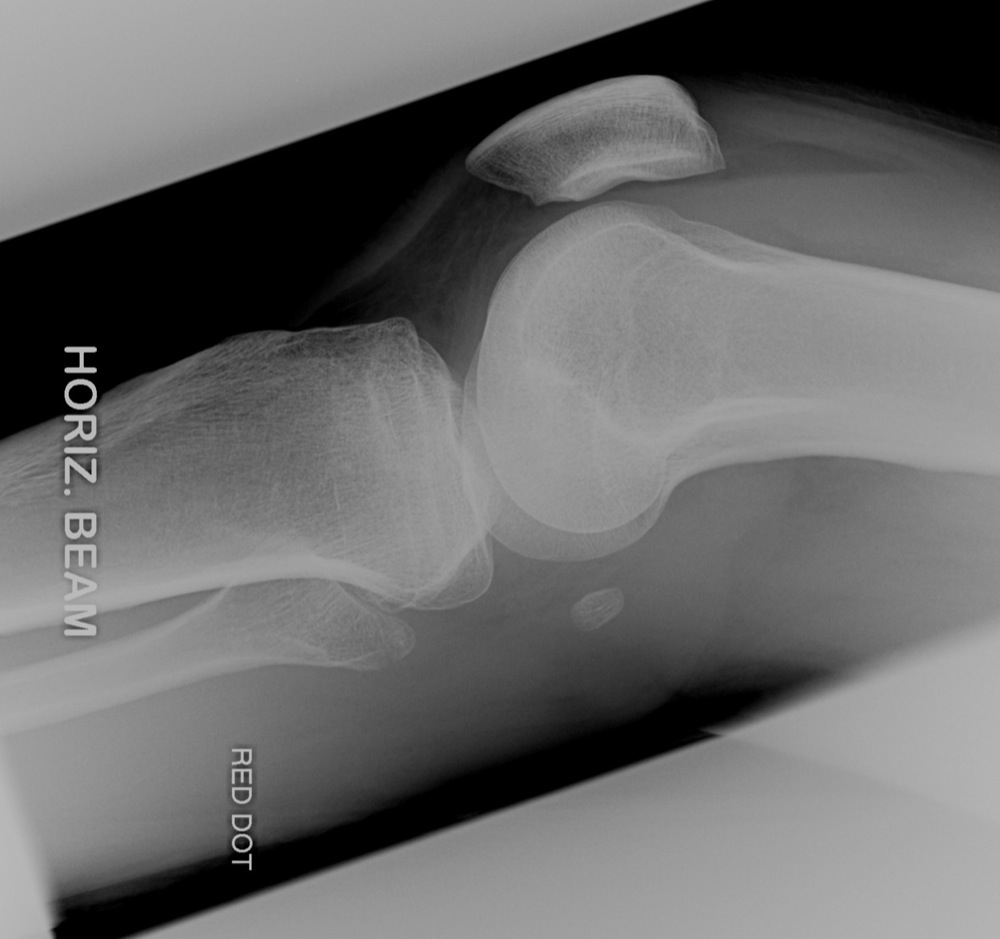
Tibial Plateau Fracture with Lipohemarthrosis (imageinterpretation.co.uk)
Schatzker Classification
- Type I: lateral plateau, split fracture
- Results from axial load with valgus stress
- Cancellous bone of lateral plateau prevents depression in young healthy patients
- Type II: lateral plateau, split-depression fracture (most common)
- Same mechanism of injury as Type I but with underlying osteopenic bone unable to resist depression
- Type III: lateral plateau, isolated depression fracture (rare)
- Compression fracture of lateral plateau, usually laterally or centrally located
- Rare and see only in older individuals or those with severe osteopenia
- Type IV: medial plateau fracture
- Results from axial or varus stress, split or split-depression fracture
- Medial plateau stronger than lateral, represents higher energy injury than Types I, II, III
- Type V: bicondylar fracture
- Medial and lateral plateau fractures with or without compression
- Results from pure axial force on extended knee, high-energy injury
- Type VI: plateau fracture with separation of metaphysis from diaphysis
- Results from combination of high-energy forces
- Complex bicondylar fracture with separation of condylar components from diaphysis
- Depression and impaction of fragments

Schatzker Classification System
Emergency Department Management
- Evaluate for other associated injuries especially in high-energy fracture patterns (Type IV, V, VI). These include other axial load fracture sites such as femoral neck, calcaneus, spine, and pilon fractures
- Medial Plateau Fractures (Type IV)
- High rate of vascular injury from concomitant knee dislocations
- Consider checking ankle-brachial index (ABI) in these patients (Egol, 2015)
- Low-energy fractures
- Do not usually require a period of observation for compartment syndrome
- Well-padded knee immobilizer/Bulky Jones dressing
- Strict non-weight bearing with orthopedic follow up
- High-energy fractures
- Often have multi-system trauma
- Increased likelihood for compartment syndrome
- Consider observation in all patients looking for development of compartment syndrome
- Open fractures and those with associated compartment syndrome or vascular compromise must be evaluated by orthopedics emergently for surgery
Prognosis
- Most elderly patients are managed non-surgically if fractures are only minimally displaced
- Operative management will ultimately depend on age of patient and practice patterns but most Type II and almost all medial/bicondylar injuries will be operative
Take Home Points
- Tibial plateau fractures can have subtle radiographic findings. Maintain a high clinical suspicion for obtaining additional imaging or CT for patients unable to bear weight in the ED following injury.
- Evaluate patients with high-energy mechanisms of injury for compartment syndrome and consider observation for serial examinations
- Discharge patients in knee immobilizer and strict non-weight bearing. This prevents further injury to articular cartilage and many patients will have concomitant ligamentous and meniscal injuries.
References
Baxter A. Emergency Imaging: A Practical Guide. Stuttgart, Germany: Thieme; 2016: 458-459.
Berkson EM, Virkus WW. High-energy tibial plateau fractures. J Am Acad Orthop Surg 2006; 14:20-31. PMID: 16394164
Cole P et al. Tibial plateau fractures. In: Browner B, Levine A, Jupiter J, Trafton P, Krettek C, eds. Skeletal Trauma: Basic Science Management and Reconstruction. Philadelphia: Saunders Elsevier, 2009: 2201-2287.
Egol KA et al. Handbook of Fractures, 5th ed. Philadelphia: Wolters Kluwer, 2015: 445-453.
Schatzker J et al. The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res 1979; 138:94-104. PMID: 445923
Schwartz DT. Emergency Radiology: Case Studies. New York: McGraw-Hill, 2008: 307-316.
Zeltzer DW, Leopold SS. Classifications in Brief: Schatzker classification of tibial plateau fractures. Clin Orthop Relat Res 2013; 471:371-4. PMID: 22744206








