Authors: Kyle Smiley (EM Resident, BAMC, San Antonio, TX), Jason Woods (PEM Attending, CHCO, Denver, CO)// Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to Critical Kids, an emDOCs series focused on pediatric emergency medicine. Pediatric emergencies are challenging. We’ll provide summaries of the evidence to support your decisions at the bedside. Our first post looks at the PECARN C-Spine Rule.
Background
- Cervical spine injuries are rare in pediatric patients1
- More patients are being diagnosed with incomplete lesions
- More patients are tetra- vs paraplegic
- Diagnosis is challenging due to varying presentations, difficult history and physical exam2
- Previous scoring tools have had poor sensitivity and specificity for predicting CSIs3,4
- Data are mixed on lifetime cancer risk in children receiving ionizing radiation5-7
- One study found 78% increase in thyroid cancer in children who received a CT of the cervical spine and another found 24% higher risk of cancer in children age <10 who had a CT.
- Studies have not demonstrated clear benefit of MRI over CT8,9
- Contradictory to adults, there is limited increase in diagnostic yield to clear C-spine in pediatrics
- Still commonly utilized as extrapolation from adult literature
- In an effort to decrease sedation risks, limited sequence MRIs have been validated, but most centers do not have access to this modality at this time
- PECARN recently published a large, prospective trial that provides guidelines for pediatric cervical spine imaging10
- Contradictory to adults, there is limited increase in diagnostic yield to clear C-spine in pediatrics
Study Design
- The PECARN prediction rule for cervical spine imaging of children presenting to the emergency department with blunt trauma: a multicentre prospective observational study included over 22,000 pediatric patients from 18 different EDs across the United States
- 11,857 in derivation cohort; 10,573 in validation cohort
- Inclusion criteria were all children treated at participating centers who had known or suspected blunt trauma and met at least one of the following criteria:
- Evaluated by the trauma team
- Had cervical spine imaging
- Transported from scene by EMS
- Excluded all children with isolated penetrating injury
- Defined high-risk as any findings associated with >10% chance of CSI
- Defined non-negligible risk factors as clinically important but <10% chance
- Primary outcome was CSI identified within 28d of initial presentation that required hospital admission and/or surgery
- Cervical spine injuries include fractures, ligamentous injuries, intraspinal hemorrhage, vertebral artery injury or spinal cord injury
- Other measures included rule performance characteristics including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV)
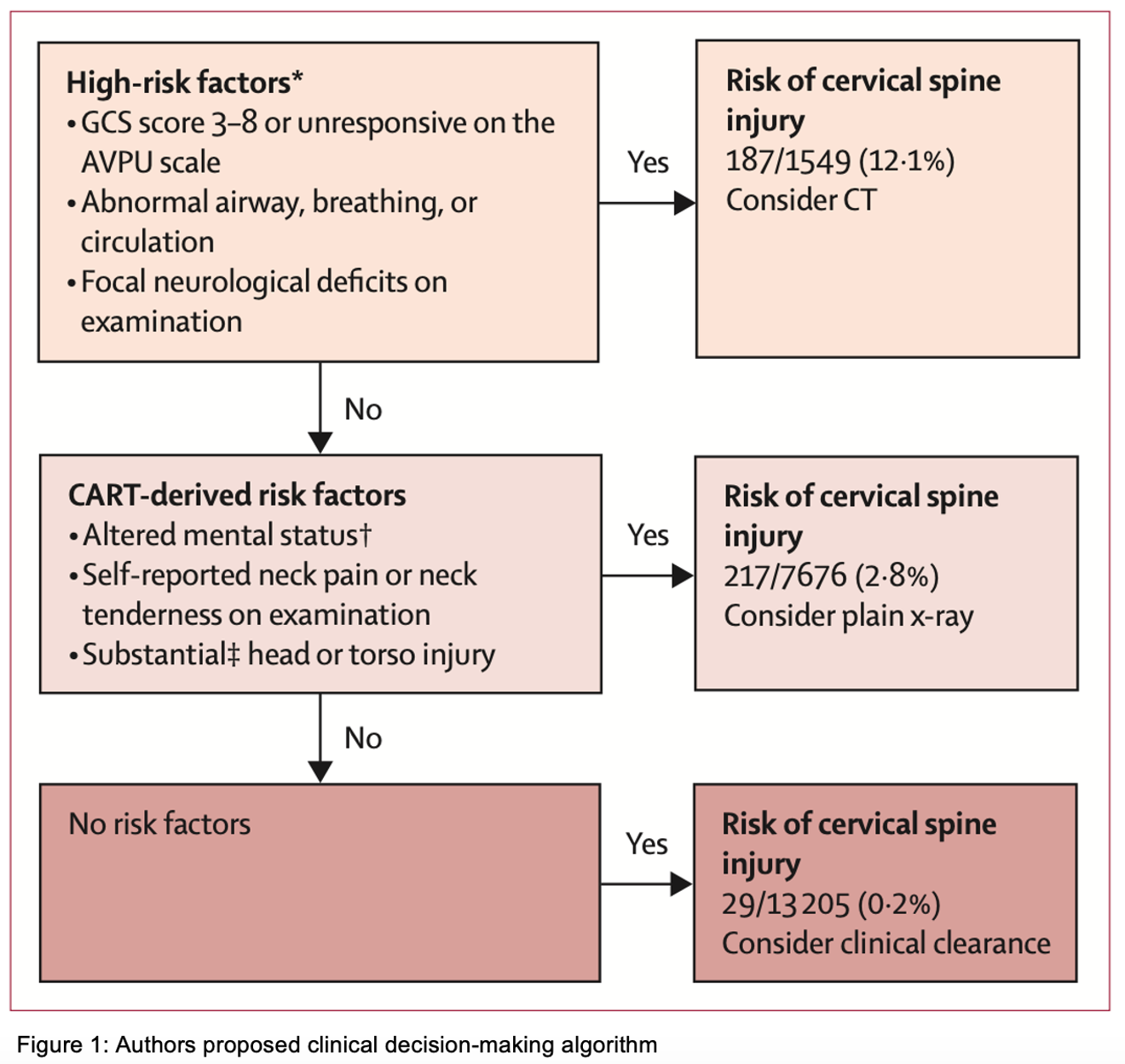
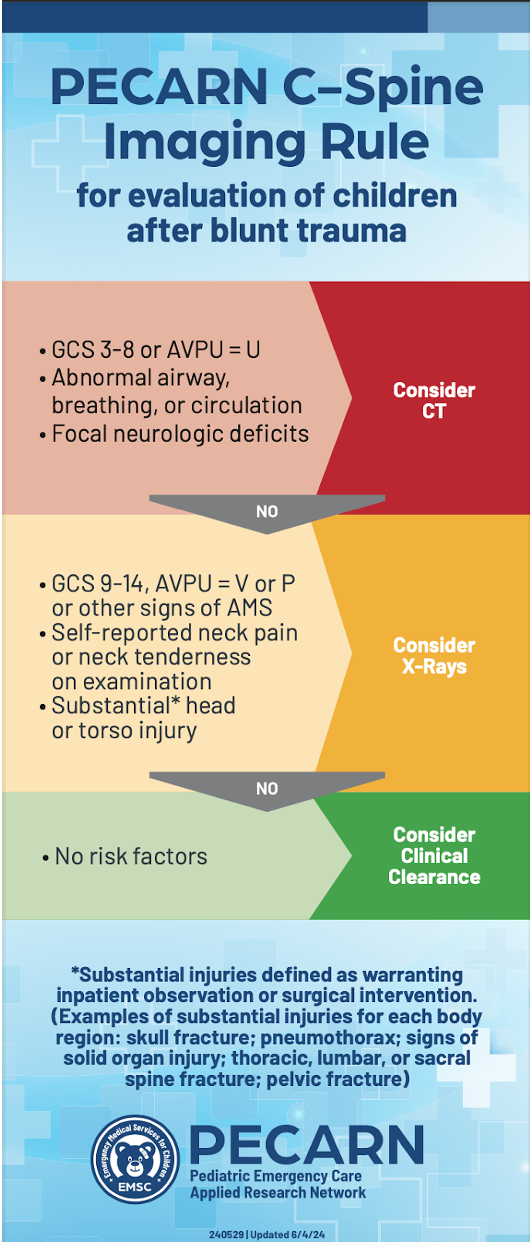
- Developed a clinical decision algorithm
Study Results
- CSI incidence was 1.9% in the studied population
- Having ≥1 of the following high-risk features conferred a risk ratio of 8.9 (95% CI 7.1-11.2)
- GCS 3-8 or U on AVPU
- Airway, breathing, circulation abnormalities
- Focal neurologic deficits
- Having 0 of the above risk factors but any of the following indicated a non-negligible risk of CSI
- Self-reported neck pain
- Midline neck tenderness on exam
- GCS 9-14 or V/P on AVPU
- Significant head or torso trauma
- Defined as injuries requiring surgical intervention or inpatient observation
- Combining the high-risk and non-negligible risk factors yields a 94.3% (95% CI 90.7-97.9) sensitivity and 60.4% (95% CI 59.4-61.3) specificity with a negative predictive value (NPV) of 99.9% (95% CI 99.8-100.0) (Figure 1)
- Authors estimate that using their imaging rules, they would decrease CT imaging of the neck from 17.2% to 6.9% in patients with traumatic injury
- Also noted no increase in number of cervical spine x-rays
- Subgroup analyses performed similarly to overall cohorts
- Transferred patient cohort had NPV of 99.8% and sensitivity of 91.5%
- Child abuse victim cohort had NPV of 99.8% and sensitivity of 92.8%
- Authors estimate that using their imaging rules, they would decrease CT imaging of the neck from 17.2% to 6.9% in patients with traumatic injury
- Missed 29 patients with CSI
- 20/29 were misclassified as having none of the risk factors
- Remaining 9 patients did not require operative intervention
- 20/29 were misclassified as having none of the risk factors
- Interestingly, hanging/strangulation mechanism of injury, suspected intoxication, distracting injury, and history of CSI did not confer enough risk to be included in the proposed clinical decision pathway
Strengths
- Large, multi-center trial
- Externally validated at different facilities than the derivation cohort
- No children were excluded for demographic factors (eg-age, race, primary language)
- Researchers assessing for outcomes were blinded to proposed clinical predictors
- Controlled for confounders such as mechanism of injury, predisposing conditions, transport method
Weaknesses/Limitations
- Only occurred in Level 1 Pediatric Trauma Centers
- May not be generalizable to community EDs, particularly when providers have different comfort levels with pediatric trauma
- Prevalence of CSI was almost double previously reported studies11,12
- Higher CSI prevalence in enrolled patients than all eligible patients and in derivation cohort compared to validation cohort
- Similar predictive performance between groups
- Did not address need for MRI imaging in patients with high pretest probability but negative initial CT
Summary
- For patients age 0-17 years with suspected or confirmed exposure to blunt trauma presenting to pediatric trauma centers, the PECARN CSI clinical decision making pathway outperforms previous screening/prediction tools.
- Use with caution in community EDs
- Applying this clinical pathway may significantly reduce radiation exposure and healthcare costs.
- More studies are needed to evaluate the rule in centers without pediatric trauma specialists.
References
- García-Rudolph A, Wright MA, Rivas N, Opisso E, Vidal J. Epidemiology of pediatric spinal trauma with neurological deficits in Catalonia: a 36-year experience. Eur Spine J. 2024 Jun 9. PMID: 38852115.
- Jeong D, Beno S, Drake JM, Freire G. Clinical characteristics of upper cervical spine injuries in children: a retrospective case series. J Neurosurg Pediatr. 2024 Feb 9;33(5):452-460. PMID: 38335518.
- Azad TD, Jiang K, Weber-Levine C, Lee RP, Jain A, Sponseller P, Groves M, Theodore N, Nasr IW, Jackson EM. Evaluation of cervical spine clearance scores in children younger than 3 years with blunt trauma. J Neurosurg Pediatr. 2024 May 31:1-7. PMID: 38820612.
- Tavender E, Eapen N, Wang J, Rausa VC, Babl FE, Phillips N. Triage tools for detecting cervical spine injury in paediatric trauma patients. Cochrane Database Syst Rev. 2024 Mar 22;3(3):CD011686. PMID: 38517085.
- Brody AS, Frush DP, Huda W, Brent RL; American Academy of Pediatrics Section on Radiology. Radiation risk to children from computed tomography. Pediatrics. 2007 Sep;120(3):677-82. PMID: 17766543.
- Chodick G, Ronckers CM, Shalev V, Ron E. Excess lifetime cancer mortality risk attributable to radiation exposure from computed tomography examinations in children. Isr Med Assoc J. 2007 Aug;9(8):584-7. PMID: 17877063.
- Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 2013; 346:
- Azizi N, Huynh JL, Raslan O, Bobinski M, Hacein-Bey L, Ozturk A. Pediatric cervical spine clearance after blunt trauma and negative CT: What is the role of MRI? J Neuroradiol. 2024 May 25;51(5):101206. PMID: 38801971.
- Melhado C, Durand R, Russell KW, Polukoff NE, Rampton J, Iyer RR, Acker SN, Koehler R, Prendergast C, Stence N, O’Neill B, Padilla BE, Jamshidi R, Vaughn JA, Ronecker JS, Selesner L, Lofberg K, Regner M, Thiessen J, Sayama C, Spurrier RG, Ross EE, Liu CJ, Chu J, McNevin K, Beni C, Robinson BRH, Linnau K, Buckley RT, Chao SD, Sabapaty A, Tong E, Prolo LM, Ignacio R, Floan Sachs G, Kruk P, Gonda D, Ryan M, Pandya S, Koral K, Braga BP, Auguste K, Jensen AR; Western Pediatric Surgery Research Consortium Cervical Spine Injury Study Group. The Sensitivity of Limited-Sequence MRI in Identifying Pediatric Cervical Spine Injury: A Western Pediatric Surgery Research Consortium Multicenter Retrospective Cohort Study. J Trauma Acute Care Surg. 2024 Mar 25. PMID: 38523120.
- Leonard JC, Harding M, Cook LJ, Leonard JR, Adelgais KM, Ahmad FA, Browne LR, Burger RK, Chaudhari PP, Corwin DJ, Glomb NW, Lee LK, Owusu-Ansah S, Riney LC, Rogers AJ, Rubalcava DM, Sapien RE, Szadkowski MA, Tzimenatos L, Ward CE, Yen K, Kuppermann N. PECARN prediction rule for cervical spine imaging of children presenting to the emergency department with blunt trauma: a multicentre prospective observational study. Lancet Child Adolesc Health. 2024 Jul;8(7):482-490. Epub 2024 Jun 4. PMID: 38843852.
- Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR. A prospective multicenter study of cervical spine injury in children. Pediatrics 2001; 108: E20.
- US Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS). 2023. https:// www.cdc.gov/injury/wisqars/index.html (accessed Dec 11, 2023).








