Originally published at EM Cases. Reposted with permission. Listen to accompany podcast HERE
Follow Dr. Anton Helman on twitter at @EMCases
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post by Winny Li & Lorraine Lau, edited by Anton Helman November, 2019
Cite this podcast as: Helman, A. Reid, A. Koblic, P. Ep 132 Emergency Approach to Seizures and Seizure Management. Emergency Medicine Cases. November, 2019. https://emergencymedicinecases.com/approach-seizures-management. Accessed Tue, 22 Apr 2025 03:20:10 +0000
General approach to the patient with a presumed resolved seizure
- ABCDEFG (ABC’s and Don’t Ever Forget the Glucose)
- Establish IV access (for medication delivery if recurrent seizure in the ED)
- Distinguish between seizure vs seizure mimics
- Distinguish between first seizure vs recurrent seizure
- Categorize the seizure
- Identify the underlying cause of seizure
- Assess for complications of seizure
- Assess anti-seizure drug levels
- Disposition and discharge instructions
Step 3: Distinguish between a seizure and seizure mimics
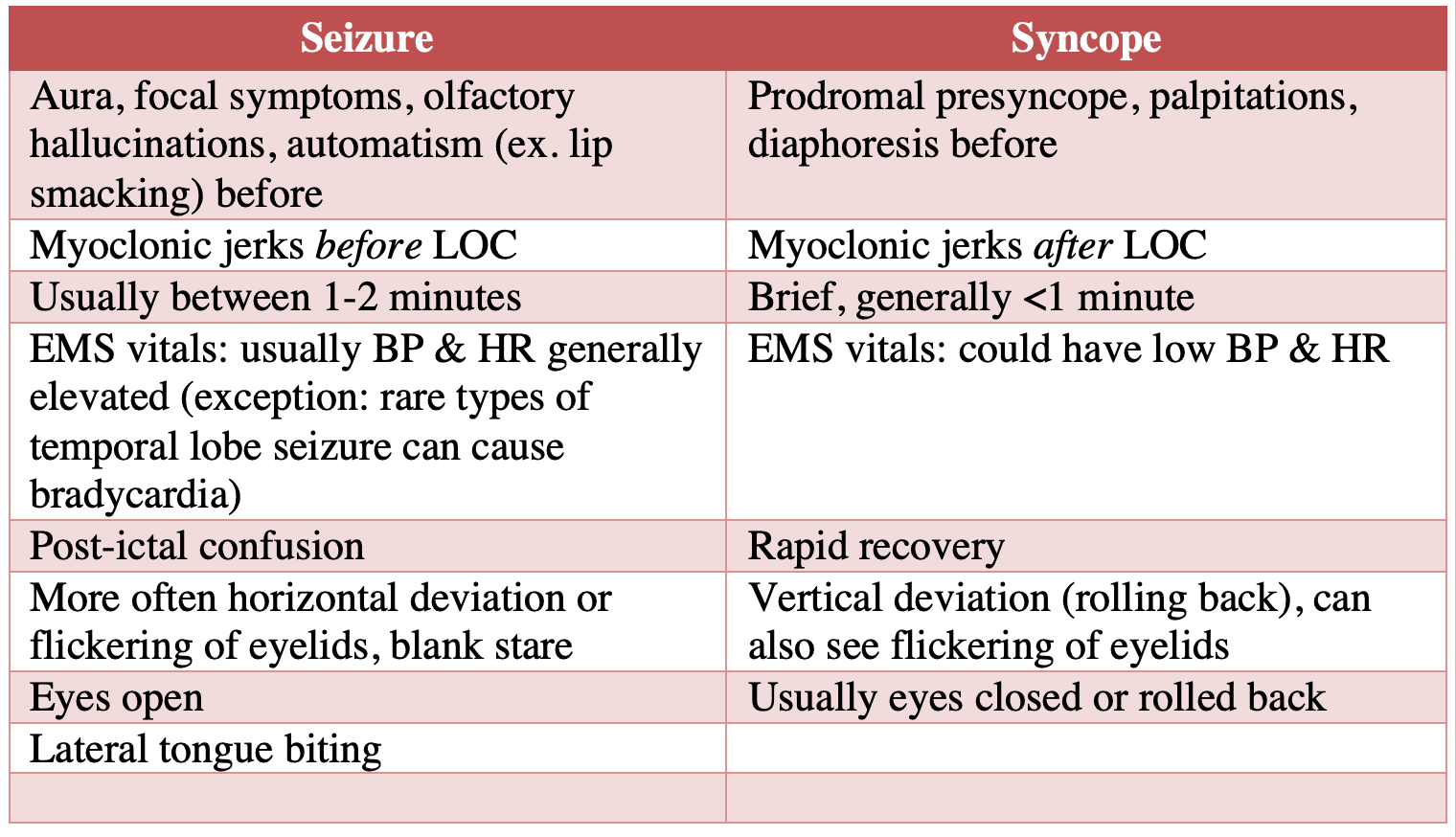
We attribute cardiac syncope to seizure in about 10-20% of patients who we label as having a seizure.
Elements that are highly suggestive of true seizure activity include (from highest LR to lowest):
- Lateral tongue-biting
- Lateral head rotation
- Unusual posturing
- Urinary incontinence
- Blue skin colour observed by bystanders
- Limb jerking
- Prodromal trembling, hallucinations, pre-occupation or deja-vu
- Amnesia for behaviors surrounding event
- Postictal phase
Factors that decrease the likelihood of true seizures
- Presyncope before LOC
- LOC with prolonged standing, sitting
- Prodromal diaphoresis, vertigo, nausea, chest pain, feeling of warmth, palpitations or dyspnea
Pearl: Lateral tongue biting has a specificity of 100% for the diagnosis of generalized tonic-clonic seizures in patients who present with a transient loss of consciousness.
Distinguishing seizure from syncope
All patients who present with a presumed seizure should have an ECG done to assess for causes of cardiac syncope.
Distinguishing seizure from psychogenic non-epileptiform seizures (PNES)
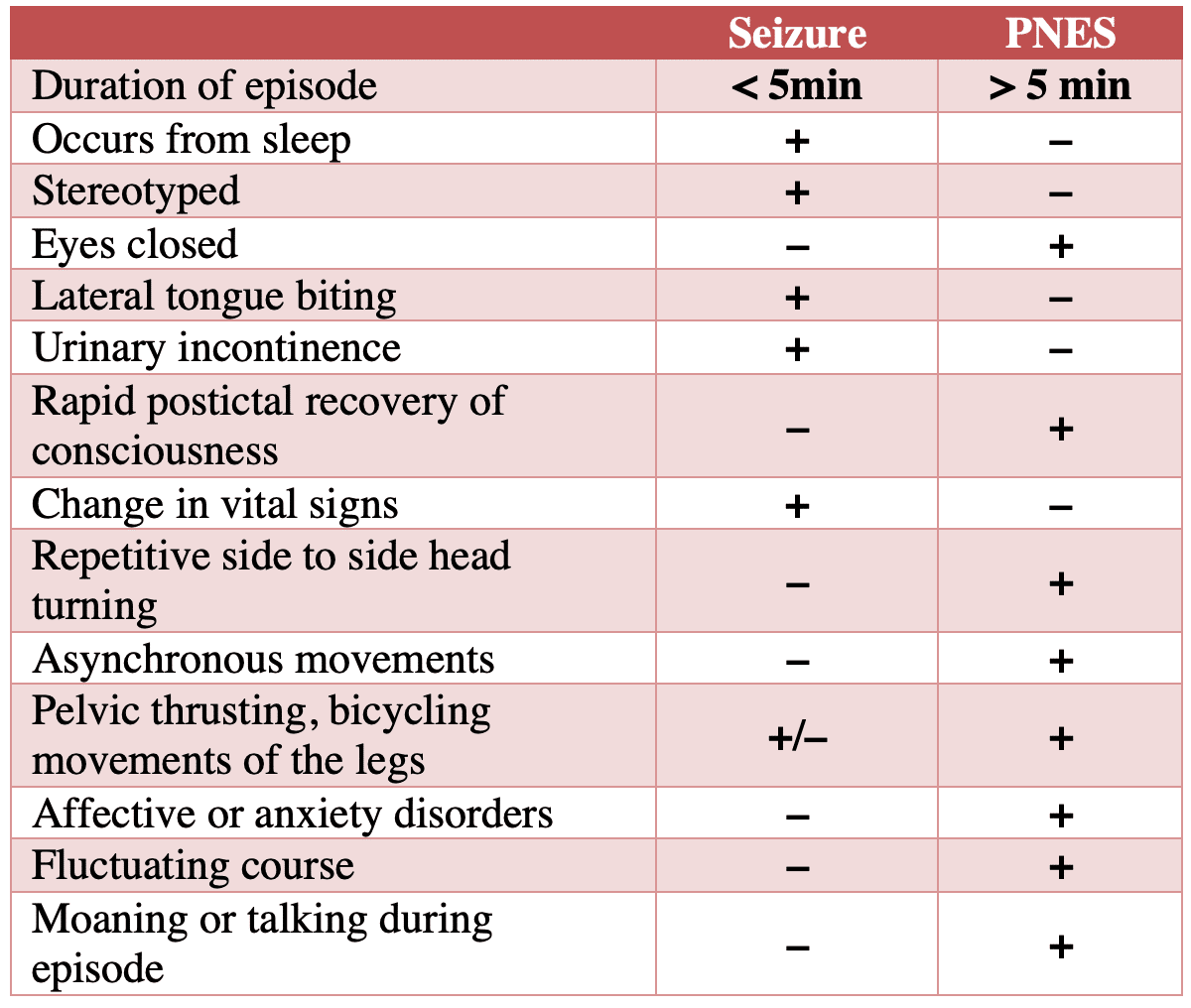
PNES, formerly “pseudoseizures”, are not due to abnormal electrical activity in the brain. When in doubt, assume true seizure as it can be extremely difficult to distinguish PNES from epileptic seizures in the ED. Video EEG is the gold standard for diagnosis, however this is not typically possible in the ED setting. Epilepsy and PNES frequently coexist in the same patient. It has been estimated that up to 60% of patients with PNES have an addition epileptic seizure disorder.
PNES is often misunderstood and patients are perceived as malingering or “faking it”. They have a morbid psychiatric illness. Approach patients with PNES with compassionate counselling and referral for Cognitive Behavioural Therapy, the only therapy proven to be beneficial for PNES. Medications do not effectively prevent or treat the events.
Pitfall: Assuming that a seizure is PNES in a patient with a history of PNES. It has been estimated that up to 60% of patients with PNES have an addition epileptic seizure disorder. When in doubt, assume true seizure as can be extremely difficult to distinguish PNES from epileptic seizures in the ED.
Distinguishing migraine from seizure
While both migraines and seizure tend to have positive neurologic symptoms (increased movement or new sensation) that march, (progress over time and spread through the body) this marching of positive neurologic symptoms occurs over a few seconds in seizures, whereas they occur over several minutes in migraines.
Distinguishing TIA from seizure and Todd’s Paralysis
While TIAs typically involve a truly abrupt onset of negative neurologic symptoms (loss of sensation or motor function), the symptoms of seizure come on more gradually and generally involve positive neurologic symptoms that march. The exception is Todd’s paralysis. Todd’s paresis/paralysis, defined as transient postictal neurologic deficits, occurs after the seizure, and symptoms can persist from seconds to days before spontaneous resolution. However, both Todd’s paralysis and seizures post-stroke are uncommon presentations. If you aren’t 100% sure why your patient has a persistent new focal neurologic finding after a seizure, or if the story of seizure is unclear, or if the patient is at high risk for a stroke, it is advisable to get on the phone with your stroke team or neurologist to help you sort out whether the patient is a candidate for thrombolysis or endovascular therapy.
Can lab values help to distinguish true seizure vs. seizure mimics?
Biomarkers such as lactate, CK and ammonia can be helpful as additional data points, but each have their own pros and cons and have ideal time period that they need to be drawn.
Lactate
Serum lactate appears to peak instantaneously after a seizure and rapidly clears, making it ineffective as a test after 1.5 hours. There may be some discriminating power, but the best cut-off is unclear and studies are all retrospective with specificities in the 80’s and sensitivities between 65-85%. In certain patient populations with other underlying medical comorbidities such as liver disease or sepsis, they may present with an elevated lactate and have delayed lactate clearance. Nonetheless, a very high lactate within 1.5hrs of seizure that clears completely after 1.5hrs is highly suggestive of a true seizure.
CK, ammonia, and prolactin
Our experts advise against routinely using other serum biomarkers such as CK, ammonia, and prolactin to rule in or out epileptic seizures. These markers have varying results across studies, with intra and inter-individual variations, and serum levels may be affected by other medical or physiological conditions.
Step 4: Distinguish between a first time seizure and recurrent seizure (hint: it’s not just a matter of asking the patient)
It is important to distinguish between a first time seizure and recurrent seizure because medical management will change depending on which it is. Ask specifically about subtle motor jerking, positive sensory phenomena, staring spells or hallucinations in the weeks and months prior to presenting to the ED that may suggest an underlying subtle chronic seizure disorder. In one observational study, 28% of patients who presented with a presumed first time generalized tonic-clonic seizure had a history of minor epileptic symptoms such as myoclonus or simple partial seizures.
Step 5: Categorize the seizure
There are numerous types of seizures that exist that do not need to be identified in the ED as workup and short term management are not dictated by seizure type. However it is important to broadly classified seizures in the ED as:
- Provoked (specific cause) or unprovoked (epilepsy)
- LOC or no LOC
- Motor symptoms or not (convulsive or nonconvulsive)
- Focal or generalized or progress from focal to generalized
- Status epilepticus (> 5min or consecutive seizures without a return to baseline in between) or not
Step 6: Identify the underlying cause of the seizure
While there are hundreds of causes of seizures, with alcohol withdrawal and epilepsy with drug noncompliance being two of the most common, it is important to rapidly identify the immediate life-threats that require specific time-sensitive antidotes.
Immediate life-threats that require immediate treatment with specific antidotes:
- Vital sign extremes: hypoxemia (O2), hypertensive encephalopathy (labetolol etc) and severe hyperthermia (cooling)
- Metabolic: hypoglycemia (glucose), hyponatremia (hypertonic saline), hypomagnesemia (Mg), hypocalcemia (Ca)
- Toxicologic: anticholinergics (HCO3), isoniazid (pyridoxine), lipophilic drug overdose (lipid emulsion) etc.
- Eclampsia: typically > 20 weeks of pregnancy and up to 8 weeks postpartum (Mg)
After any immediate life-threats have been identified and treated it may be useful to divide causes into intracranial vs systemic, and consideration for imaging and lumbar puncture should be entertained.
Indications for ED CT head in patients who present with a seizure
Consider a non-contrast CT head in patients with a:
- First time seizure
- Prolonged postictal period or persistent altered mental status
- History of malignancy, immunocompromised, bleeding disorder/anticoagulation, shunt, neurocutaneous disorder, chronic alcohol abuse
- Fever
- Non-trivial head injury
- New focal onset seizure
- Persistent focal neurological deficit
Do all patients with first time seizure require a CT head?
Both the American Academy of Neurology and ACEP recommend emergent CT head in adults with first time seizure, noting that CT findings in these patients changes acute management in 9-17% of cases. One study of 259 patients with a first alcohol-related seizure showed a clinically significant CT head lesion in 6.2% of patients even when the history and physical examination were nonfocal. This suggests that patient with a history of alcohol use disorder who present with a seizure should not be presumed to be suffering an alcohol withdrawal seizure as the underlying cause, and that we should have a low threshold for imaging patients with alcohol use disorder with a first-time seizure.
Step 7: Assess for complications of the seizure
Potential sequelae of seizures include trauma (TBI, long bone fractures, dislocations – posterior shoulder dislocation is a classic injury that often has subtle findings) hypoglycemia, acidosis, rhabdomyolysis, AKI, hyperkalemia, aspiration, neurogenic pulmonary edema, neurogenic cardiac injury (cardiac Takotsubo cardiomyopathy, tachyarrhythmia and sudden unexpected death in epilepsy – SUDEP).
Consider serial troponins and ECGs in patients with prolonged seizures or risk factors for CAD as these patients are at risk for developing cardiac ischemia secondary to a seizure.
Pearl: An elevated troponin in seizure is NOT a benign post seizure change, it should prompt a cardiac work up!
Step 8: Assess anti-seizure drug levels
Anti-seizure drug levels are recommended for any patient with known epilepsy/seizure disorder who has a change in their seizure pattern. Factors that affect drug levels and dictate target drug levels include:
- Their usual target drug level
- Drug compliance
- Any new medications that may interact with the anti-seizure medication (eg antibiotics, Wellbutrin)
- Change in frequency, duration or features of the seizure
- Intercurrent illness that may lower the the seizure threshold
Anti-seizure drug levels can be difficult to interpret, especially when multiple drugs are on board, so our experts recommend consulting a neurologist to aid in adjusting drug dosages for all but the noncompliant patient who requires a drug load (see below). Anti-seizure drug concentration assays available to most EDs include: phenytoin, valproate, phenobarbital and carbamazepine. Drug levels that are not immediately available in the ED but may be useful for our neurology colleagues in follow-up include: lamotrigine, levetiracetam (Keppra) and clobazam.
Anti-seizure medication drug loading: What’s the evidence? Is Oral or IV better?
The ACEP Clinical Policy 2014 suggests that for anti-seizure medications given in the ED setting for patients with a known seizure disorder in which resuming their antiepileptic medication is deemed appropriate, there is a lack of evidence to support one route of administration (oral versus parenteral) over the other in terms of preventing early recurrent seizure. Our experts prefer oral loading because the acute side effects of IV loading may prolong length of stay in the ED. Although loading with antiepileptic medication is commonly done, there is a lack of evidence to support or refute this practice.
Should patients with a first time seizure be loaded on an anti-seizure medication in the ED?
Our experts agree with the recommendations from the American Academy of Neurology, that first-time unprovoked seizure patients who are back to baseline and suitable for discharge do not require loading on anti-seizure medications.
Certain patients at higher risk of recurrent seizures can be considered for medication loading in the ED. For a patient with a first unprovoked seizure clinical factors associated with an increased risk for seizure recurrence include a prior stroke or TBI, a significant neuro-imaging abnormality, or a nocturnal seizure. While the decision to start anti-seizure medications should be individualized, clinicians should advise patients with an unprovoked first seizure that over the longer term (>3 years), immediate treatment is unlikely to improve the prognosis for sustained seizure remission.
Our experts recommend Levetiracetam oral load of 1,500mg in the ED followed by 500-1000mg po bid as the drug of choice for ED loading of the first time seizure patient who is deemed appropriate for a drug load because of its effectiveness for both focal and generalized seizures as well as its safety profile. Consider an alternative for patients with known psychiatric illness as levetiracetam may worsen psychiatric symptoms.
|
Oral Loading Dose | IV Loading Dose | |
|---|---|---|---|
| Carbamazepine (Tegretol) | 8mg/kg suspension in single oral load | NA | |
| Gabapentin (Neurontin) | 900mg/day oral (300mg tid) for 3 days | NA | |
| Lamotrigine (Lamictal) | 6.5mg/kg single oral load if on lamotrigine for >6 mo without a history of rash or intolerance in the past and only off lamotrigine for <5 days | NA | |
| Levetiracetam (Keppra) | 1,500mg oral load, followed by 500-1000mg bid | 1,000-1,500 mg IV | |
| Phenytoin (Dilantin) | 20mg/kg divided in maximum doses of 400mg every 2 hours | 18mg/kg (max rate of 50mg/min) | |
| Fosphenytoin (Cerebyx) | NA | 18 PE/kg IV (max rate of 150 PE/min) | |
| Valproate (Depacon) | NA | Up to 30mg/kg IV (max rate of 10mg/kg/min) |
Step 9: Disposition and discharge instructions of the patient with seizure
Which patients with a first-time generalized seizure can be safely discharged home?
Those with a single first-time generalized seizure and otherwise normal history and physical who return to neurological baseline can be discharged home with close follow-up with outpatient neurology. If discharged, the patient should have somebody monitor them for recurrent seizure for 24hrs given the significant risk of recurrent seizure (up to 9%).
Indications for, and timing of, EEG
EEG are useful in confirming epileptic brain activity, defining seizure type and quantifying risk of recurrence. Status epilepticus patients and post status epilepticus patients need an EEG ASAP. Patients with a first unprovoked seizure and patients with a change in their baseline pattern of seizures should get an EEG ideally within a few days, as the diagnostic yield of an EEG decreases with time.
Discharge instructions and mandatory reporting for the patient who presents to the ED with a seizure
Good discharge instructions can be lifesaving – patients need to know not to swim, bathe alone or a baby in a bathtub, climb heights, operate heaving machinery or drive. In Ontario, it is mandatory to report anyone 16 years of age or older who has had a seizure to the Ministry of Transportation regardless of whether or not they have a driver’s license. Check your local regulations and policies for laws regarding mandatory reporting.
Take home points for emergency approach to resolved seizures
- ABCDEFG – Don’t Ever Forget the Glucose.
- Immediate life threats with specific antidotes: the vital extremes – hypoxemia, hypertensive encephalopathy and hyperthermia, metabolic causes – hypoglycemia, hyponatremia, hypomagnesemia, hypocalcemia, toxicologic causes like TCA, and eclampsia which can occur up to 8 weeks postpartum.
- For lab work think about both the causes and the complications of seizures like rhabdomyolysis and acidosis. Consider serial troponins in at-risk patients and serial lactates if you’re not sure if it is a true epileptic seizure. Consider drug levels, both the ones that you can get back immediately and those that might be helpful for the follow up neurologist.
- Have a low threshold for CT head for first time seizure patients and for alcoholics who present with withdrawal seizures.
- Key elements to distinguish true seizure from seizure mimics include lateral tongue biting (100% specificity), EMS vital signs of elevated HR and BP, lateral gaze deviation and post-ictal altered mental status.
- To distinguish TIA from seizure, TIAs usually have a truly abrupt onset of negative phenomena – a loss of sensation or power vs a seizure or migraine – they march – the motor or sensory symptoms progress over time and migrate through the body, with that marching happening faster in a seizure compared to a migraine.
- Todd’s Paralysis is rare, occurs after the seizure and can last seconds to days. If the story is unclear or the patient is at high risk for stroke, it’s advisable to get on the phone with your stroke team or neurologist to help you sort out whether the patient is a candidate for thrombolysis or endovascular therapy.
- When in doubt whether or not a seizure was a true epileptic seizure or a psychogenic seizure, err on the side of true seizure – even neurologists with the aid of EEG video monitoring can be fooled.
- Drug level interpretation is complicated unless levels are undetectable; consult a neurologist for guidance, especially for patients taking multiple anti-seizure medications
- In the ED, oral Keppra is probably the safest choice for loading patients in the ED.
- First time unprovoked seizure patients who are back to baseline and suitable for discharge do not require loading on anti-seizure medications.
- EEG is indicated for all status epilepticus and post status epilepticus patients ASAP, and within a few days for patients with undiagnosed unprovoked seizures
- Good discharge instructions can be lifesaving, and know your local rules around mandatory reporting.
References
- King MA, Newton MR, Jackson GD, Fitt GJ, Mitchell LA, Silvapulle MJ, et al. Epileptology of the first-seizure presentation: a clinical, electroencephalographic, and magnetic resonance imaging study of 300 consecutive patients. Lancet. 1998 Sep;352(9133):1007–11.
- Sheldon R et Historical criteria that distinguish syncope from seizures. J Am Coll Cardiol. 2002 Jul 3;40(1):142-8.
- Benbadis SR et al. Value of tongue biting in the diagnosis of seizures. Arch Intern Med. 1995 Nov 27;155(21):2346-9.
- Krumholz A, Wiebe S, Gronseth G, et al. Practice Parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2007; 69(21):1996-2007.
- Seizures ACEP Policy committee. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department With Seizures. Ann Emerg Med. 2014;63(4):437–447.e15. doi:10.1016/j.annemergmed.2014.01.018.
- Limdi NA, Shimpi AV, Faught E, et al. Efficacy of rapid IV administration of valproic acid for status epilepticus. Neurology. 2005;64:353-355.
- Chen L, Feng P, Wang J, et al. Intravenous sodium valproate in mainland China for the treatment of diazepam refractory convulsive status epilepticus. J Clin Neurosci. 2009;16:524-526.
- Gilad R, Izkovitz N, Dabby R, et al. Treatment of status epilepticus and acute repetitive seizures with i.v. valproate acid vs phenytoin. Acta Neurol Scand. 2008;118:296-300.
- Marson A, Jacoby A, Johnson A, et al; Medical Research Council MESS Study Group. Immediate versus deferred antiepileptic drug treatment for early epilepsy and single seizures: a randomised controlled trial. Lancet. 2005;365:2007-2013.
- Chadwick DW. The treatment of the first seizure: the benefits. Epilepsia. 2008;49(suppl 1):26-28.
- Gottlieb M, Clayton GC. Should Antiepileptic Drugs Be Initiated in the Emergency Department After a First-Time Seizure?. Ann Emerg Med. 2017;69(6):752-754.
- Leone MA, Giussani G, Nolan SJ, et al. Immediate antiepileptic drug treatment, versus placebo, deferred, or no treatment for first unprovoked seizure. Cochrane Database Syst Rev. 2016;(5):CD007144.
- An Evidence Based Approach to the First Seizure. Calgary. Supplement – Management of First Time Seizure. Epilepsia, 49(Suppl. 1):50-57, 2008.
- Doğan EA, Ünal A, Ünal A, Erdoğan Ç. Clinical utility of serum lactate levels for differential diagnosis of generalized tonic-clonic seizures from psychogenic nonepileptic seizures and syncope. Epilepsy Behav. 2017;75:13-17.
Drs. Helman, Koblic and Reid have no conflicts of interest to declare









1 thought on “EM Cases: Emergency Approach to Resolved Seizures”
Pingback: Nerdfallmedizin.de - NERDfall Nr. 15 – Teil 2: Dissoziative Krampfanfälle – gar nicht so selten und häufig fehlinterpretiert