Originally published at EM Cases – Visit to listen to accompanying podcast. Reposted with permission.
Follow Dr. Anton Helman on twitter @EMCases
Just one case of missed pediatric physical abuse I consider a travesty. The sad state of affairs is that thousands of cases of pediatric physical abuse are missed on initial presentation to EDs across North America. And a small but significant minority of these children die. In fact, 20-30% of children who died from abuse and neglect had previously been evaluated by medical providers for abusive injuries that were not recognized as abuse. Every child that presents to the ED with a suspicious injury gives the treating physician an opportunity to intervene. We have to get better at identifying these kids when there’s still something we can do to protect them, before it’s too late. In this EM Cases main episode podcast on Pediatric Physical Abuse Recognition and Management Dr. Carmen Coombs and Dr. Alyson Holland discuss the 6 B’s of child abuse, the TEN-4 FACE decision rule, the Pittsburgh Infant Brain Injury Score, disclosure tips, screening tests, reporting responsibilities and more…
Podcast production by Anton Helman. Editing and sound design by Richard Hoang & Anton Helman
Written Summary and blog post by Shaun Mehta & Alex Hart, edited by Anton Helman February, 2018
Cite this podcast as: Helman, A, Coombs, C, Holland, A. Pediatric Physical Abuse Recognition and Management. Emergency Medicine Cases. March, 2018. https://emergencymedicinecases.com/pediatric-physical-abuse/. Accessed Tue, 22 Apr 2025 03:19:46 +0000.
Why pediatric physical abuse matters
For those children who survive their physical trauma, there are both short term and long term effects. Short term effects include risk of escalating abuse with increased risk of morbidity and mortality. Long term effects include developmental delays, mental health issues, chronic disease and substance abuse according to the ACEs Study.
Emergency providers’ responsibility in suspected pediatric physical abuse
The unfortunate truth is, if we don’t think about abuse, we’ll definitely miss it. So, the most important first step is always simply to think about it. Then our responsibility turns to reporting it, considering the differential diagnosis, investigating what is medically necessary and ensuring appropriate follow up or admission if necessary.
Sentinel injuries are minor injuries with major significance
Much as with sentinel bleeds of subarachnoid hemorrhages, even seemingly trivial injuries of abuse can be viewed as “sentinel events” for much worse outcomes in the future. According to Sheets et al in 2013, as many as 25% of abused infants had prior sentinel injuries.
One reason we miss physical abuse in these kids is that most sentinel injuries are minor injuries such as bruises, intraoral injuries, or simple fractures and we overlook the real significance of these injuries, which is that they provide an opportunity for us to intervene before more serious injury occurs. As EM providers, recognizing and responding appropriately to sentinel injuries protects kids. Failure to do so can result in repeated abuse and subsequent morbidity and mortality.
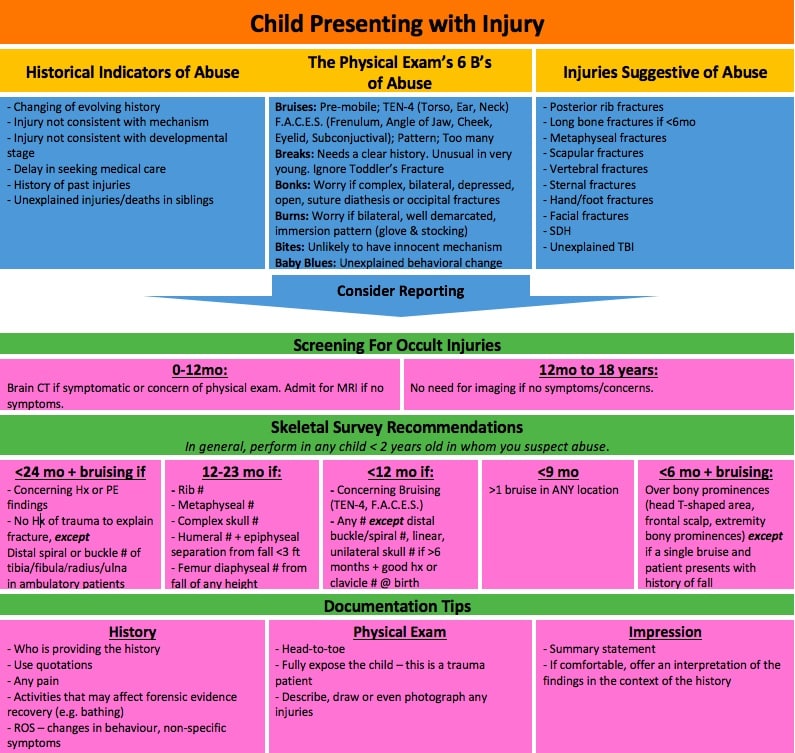
Historical Indicators of Pediatric Physical Abuse
- No/vague explanation for a significant injury
- Important detail of the explanation changes dramatically
- Explanation given is inconsistent with the child’s physical and/or developmental capabilities
- Different witnesses provide different explanations
- Injury occurred as a result of inadequate supervision
- Delay in seeking medical care without reasonable explanation
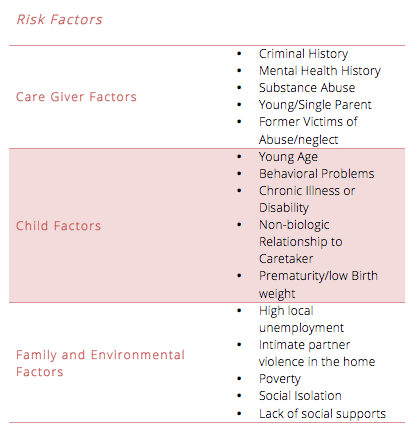
Remember though that no child is immune from abuse and an absence of the above risk factors does not preclude one from investigating suspicious injuries further. Indeed, it is in this population that abuse is often missed.
Physical Exam Findings Suggestive of Abuse: The 6 B’s
As children learn to run, walk and explore new environments, they are bound to hurt themselves. Teasing apart which injuries are due to normal childhood rambunctiousness and those that are a result of abuse requires vigilance and a thorough assessment. Remember to fully undress your patients in order to complete a head to toe exam (Teeuw et al 2012) that won’t miss subtler injuries.
Signs of disciplinary abuse are usually found on areas of the body that are concealed by clothing such as the back and buttocks.
Look for
- Injuries at different stages of healing
- Multiple Injuries
- Patterned Injuries
- Any injury in a young infant.
Other clues include
- Poor child hygiene
- A child who appears, anxious, withdrawn or fearful of a person in the room
6 B’s – Bruises, Breaks, Bonks, Burns, Bites, Baby blues
Bruises
The most common abusive injury is a bruise. Kids bruise often, but certain scenarios should raise alarm bells.
A) Bruising in the pre-mobile infant.
“If you don’t cruise, you don’t bruise.”
Pierce et al found that only 1.3% of infants less than 5 months old had bruising.
Feldman et al found that over 50% of pre-mobile infants with bruising were victim of abuse.
Make certain you base your assessment on the child’s developmental stage and not absolute age.
Bruising in infants is very rare. Not all of these babies are abused but they almost always (ie, unless there was significant trauma in a public setting with multiple witnesses) warrant further evaluation for child abuse.
B) Bruising in an unusual/protected area
TEN-4 FACES Bruising Rule (Pierce 2010)
Any bruise found in any of the following locations should trigger the possibility of pediatric physical abuse:
Torso
Ears
Neck
Any bruise in a child younger than 4 months old
FACES
Frenulum
Angle of Jaw
Cheek
Eyelid
Subconjunctival Hemorrhage
Pearl: Think of a subconjunctival hemorrhage in an infant as a bruise on the eyeball and frenulum injury as a bruise to the frenulum. These injuries are highly suggestive of abuse in the infant.
C) Patterned Bruises
- Linear bruises to buttock (whipping, spanking, paddling)
- Linear bruising to the pinna
- Retinal bleeding
- Hand prints or oval marks
- Belt Marks – U-shaped end or associated buckle inflicted puncture wounds
- Loop marks (rope, wire, electric cord)
- Ligature marks, circumferential rope burns to neck, wrists, ankles and gag marks to comers of the mouth
D) Too Many Bruises
It is helpful when consider whether or not a patient has too many bruises to compare with bruise prone areas such as the shins.
Don’t try to age/date bruises as physicians are unreliable at determining the age of bruises.
Breaks
While there are no fractures that are pathagnomonic for abuse, any fracture in any age group can be abusivedepending on how the fracture was sustained. Most abusive fractures occur in children < 18 months of age so again, our highest level of suspicion should be in young children. An important exception is that of the Toddler’s fracture which requires little force and can occur from simple falls.
1. Any fracture in a nonambulatory infant or child
2. Femur fracture in an infant < 12-18 months of age
Baldwin 2011: The odds of a femur fracture being abuse rather than accidental trauma was 19 times greater for children < 18 mo of age.
3. Humerus fractures in an infant < 18 months of age
Pandya 2010: Children < 18 mo with a humerus fracture had a 32 greater odds of being the victim of abuse.
Location: Proximal and mid shaft humeral fractures are more likely due to abuse whereas distal humerus/supracondylar fractures are less likely to be due to abuse.
4. Multiple fractures and/or an unexpected healing fracture
5. Skull fractures, especially if complex or bilateral
Deye 2013: A small (~5%) but not insignificant number of infants < 12 months old with apparently isolated skull fracture undergoing abuse evaluation were found to have additional unexpected fractures on skeletal surveys.
Most acute fractures are symptomatic but there are some fractures (metaphyseal fractures and rib fractures) which are often occult and only identified on imaging and are highly concerning for child abuse. These fractures may be found “incidentally” when getting imaging for a different reason (ie, a rib fracture seen on a chest xray obtained in an infant with suspected pneumonia) but need to be addressed the same as any abusive injury.
6. Classical metaphyseal fractures (bucket handle fractures) from being shaken violently back and forth
7. Rib fractures, especially posterior rib fractures (highest probability for abuse)
Every injury can be caused by abuse. Nothing is pathognomonic for abuse.
Bonks
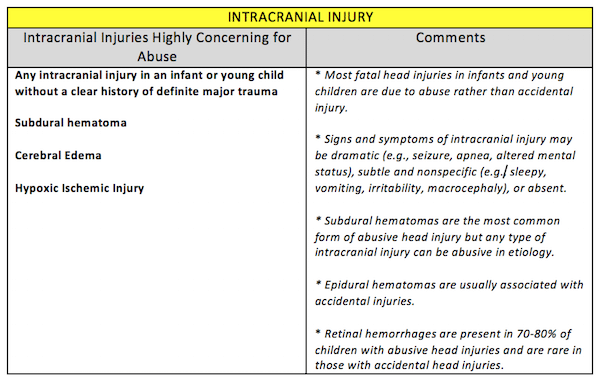
Signs of abusive head trauma can be subtle and non-specific. The Pittsburgh Infant Brain Injury Score (PIBIS) by Berger et al (see below) can help decide which patients warrant head imaging.
Skull fractures are most often accidental, but a small proportion are associated with abuse according to Deye et al in 2013. Increase your suspicion for abuse if skull fractures are complex, bilateral, depressed, open, presenting with suture diathesis or occipital fractures.
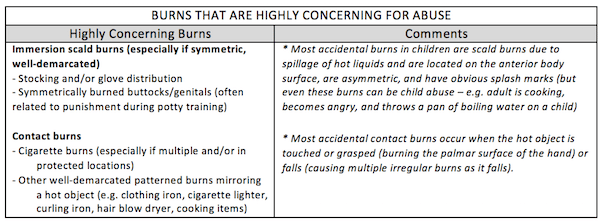
Burns
Bites
Human bites have typical, stereotyped pattern.
Baby Blues (Irritability)
Some severe injuries (see head trauma) can present with very non-specific symptoms. This is why it is so important to fully examine all concerning patients.
Screening for Medical Conditions Mimicking Abuse
The two most common conditions that mimic bruising are Mongolian spots and hemangiomas.
Compared to a bruise, Mongolian spots (congenital dermal melanocytosis) are bluish-green and located on the buttocks/lower back, present at birth, are non-tended, and fade over months to years. Hemangiomas are also non-tender, subcutaneous, and proliferate over time. If in doubt, use POCUS!
Many conditions may predispose a child to bruising and bleeding including HSP, ITP, leukemia and hemophilia, and consider osteogenesis imperfecta and rickets in children who present with fractures as a result of a minimal force mechanism.
Screening for occult injuries: The workup in suspected pediatric physical abuse
The basic medical evaluation for suspected physical abuse in a young child includes a skeletal survey, head imaging, and trauma labs.
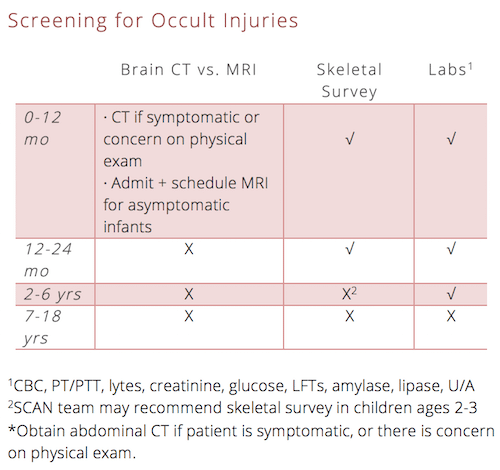
Which children suspected of abuse require a skeletal survey?
Detailed guidelines for skeletal survey in young children can be found here.
As a general guide: Any child < 2 yo in whom you suspect abuse should undergo a skeletal survey.
Pediatric abusive head trauma
Head trauma in young children may present with non-specific symptoms. Signs and symptoms of abusive head trauma in an infant or young child can be subtle or non-specific (sleepy, vomiting, fussy, lethargic) or even completely absent and these are the cases we often to fail to recognize.
Pittsburgh Infant Brain Injury Score (PIBIS) for Abusive Head Trauma
The 5-point PIBIS
- Abnormality on dermatologic examination (2 points),
- Age ≥3.0 months (1 point),
- Head circumference >85th percentile (1 point), and
- Serum hemoglobin <11.2g/dL (1 point).
At a score of 2, the sensitivity and specificity for abnormal neuroimaging was 93.3% (95% confidence interval 89.0%–96.3%) and 53% (95% confidence interval 49.3%–57.1%), respectively.
Full PDF of validation study of Pittsburgh Score
3 Ds – Documentation, Disclosure & Disposition in pediatric physical abuse
Documentation in pediatric physical abuse
Proper documentation can be challenging but is extremely important in these scenarios. The chart is a medicolegal document that may be called upon if an investigation takes place.
History
- Who is providing the history
- What, when, who
- Use quotations to document exact statements from child and caregiver
- Any pain that the child is experiencing
- Activities that may affect forensic evidence recovery (eg. bathing)
- Review of systems – changes in behaviour, non-specific symptoms
- The usual (past medical history, social history, meds, allergies)
Physical Exam
- Head-to-toe
- Fully expose the child – this is a trauma patient
- Describe, draw or even photograph any injuries
Impression
- Summary statement
- If comfortable, offer an interpretation of the findings in the context of the history
Disclosure tips in pediatric physical abuse
Be direct and professional. “As a physician, I worry when I see X, Y and Z and it makes me concerned that someone may have hurt your child.”
Refrain from being accusatory. “It’s not my role to say who hurt your child but it is my obligation to report my concern.”
Encourage the family to focus on the child. “Right now, we need to make sure that your child gets the medical care that he/she needs.”
Call for help. Discuss the case with social work, child protective services, a child abuse consultant (eg. SCAN team), and the primary care physician.
Disposition in pediatric physical abuse
To admit or not to admit? If you are concerned about the child’s safety, then admit to hospital for observation and further work up. Discharge from ED only if the medical evaluation is complete and safe disposition can be arranged by child protective services from the ED.
What is our responsibility in reporting of suspected pediatric physical abuse?
The specific rules around reporting abuse vary across the jurisdictions, but the fundamental principle is the same: health care providers need only reasonable suspicion that a child is being harmed to report, not “proof”. We are penalized for failing to report suspicion, not for reporting unsubstantiated suspicion. Reporting to the provincial or state child welfare office is legally mandated. Reporting to pediatric specialists and healthcare centers specializing in child abuse pediatrics is often useful but does not fulfill that legal mandate.
Take home points for Detection and Management of Pediatric Physical Abuse
Sentinel injuries are minor injuries with major significance. These may appear minor, but are often missed and provide an opportunity for us to intervene before serious injury.
No child is immune from abuse. While risk factors for abuse may be helpful in triggering a suspicion for abuse, many children who suffer from abuse have no identifiable risk factors.
The most common abusive injury is a bruise. If you don’t cruise, you don’t bruise. Keep an eye out for the 6 B’s of child abuse.
Head trauma in young children may present with non-specific symptoms. Be suspicious in the right clinical context.
Concerning features for abuse are subtle. These include delay in seeking care, vague or changing history of trauma, mismatch of history and injury or developmental stage of child, and multiple or patterned injuries.
Certain injury patterns should always raise concern for abuse. These include posterior rib fractures, subdural hematomas, immersion burns, patterned bruises and others. None are pathognomonic. Use the TEN-4 FACE decision tool.
The basic medical evaluation for suspected physical abuse in a young child includes a skeletal survey, head imaging, and trauma labs. There are recommendations when and when not to investigate.
Report abuse when you are suspicious – it is your legal responsibility. Regional guidelines vary, but report based on suspicion, not on proof.
Best review article on Evaluation of Suspected Pediatric Child Abuse Full PDF
Excellent article on Assessment of Bruising in Assessing Child Abuse Full PDF
Diagnostic imaging for suspected child abuse Full PDF
![]() For more on child abuse on EM Cases:
For more on child abuse on EM Cases:
BCE 67 Child Abuse – Sentinel Injuries
For more EM Cases content on Pediatric Emergencies check out our free interactive eBook,
EM Cases Digest Vol. 2 Pediatric Emergencies here.
Drs. Helman, Coombs and Holland have no conflicts of interest to declare
References on pediatric physical abuse
- Christian CW. The evaluation of suspected child physical abuse. Pediatrics. 2015;135(5):e1337-54.
- Tiyyagura G, et al. Barriers and Facilitators to Detecting Child Abuse and Neglect in General Emergency Departments. Ann Emerg Med. 2015;66(5):447-54.
- Pierce MC, Magana JN, Kaczor K, et al. The Prevalence of Bruising Among Infants in Pediatric Emergency Departments. Ann Emerg Med. 2016;67(1):1-8.
- Pierce MC, Kaczor K, Aldridge S, O’flynn J, Lorenz DJ. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics. 2010;125(1):67-74.
- Kemp A. Abusive head trauma: recognition and the essential investigation. Arch Dis Child Educ Pract ED. 2011; 96:202-8.
- Wu SS, Ma CX, Carter RL, et al. Risk factors for infant maltreatment: a population-based study. Child Abuse Negl. 2004;28(12):1253-64.
- Kellogg ND. Evaluation of suspected child physical abuse. Pediatrics. 2007;119(6):1232-41.
- Maguire S, Mann MK, Sibert J, Kemp A. Are there patterns of bruising in childhood which are diagnostic or suggestive of abuse? A systematic review. Arch Dis Child. 2005;90(2):182-6.
- Pierce MC, Kaczor K, Aldridge S, O’flynn J, Lorenz DJ. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics. 2010;125(1):67-74.
- Laskey AL, Holsti M, Runyan DK, Socolar RR. Occult head trauma in young suspected victims of physical abuse. J Pediatr. 2004;144(6):719-22.
- Bulloch B, Schubert CJ, Brophy PD, Johnson N, Reed MH, Shapiro RA. Cause and clinical characteristics of rib fractures in infants. Pediatrics. 2000;105(4):E48.
- Ricci LR. Positive predictive value of rib fractures as an indicator of nonaccidental trauma in children. J Trauma. 2004;56(3):721.
- Barnes PM, Norton CM, Dunstan FD, Kemp AM, Yates DW, Sibert JR. Abdominal injury due to child abuse. Lancet. 2005;366(9481):234-5.
- Bax, B, Wang, N.E. Physical Abuse of Children: Identification, Evaluation, and Management. Pediatric Emergency Medicine Reports. 2012.
- Ricci LR. Positive predictive value of rib fractures as an indicator of nonaccidental trauma in children. J Trauma. 2004;56(3):721.
- Maguire SA, Kemp AM, Lumb RC, Farewell DM. Estimating the probability of abusive head trauma: a pooled analysis. Pediatrics. 2011;128(3):e550-64.
- Wood JN, Fakeye O, Mondestin V, Rubin DM, Localio R, Feudtner C. Development of hospital-based guidelines for skeletal survey in young children with bruises. Pediatrics. 2015;135(2):e312-20.
- Sittig JS, Uiterwaal CS, Moons KG, et al. Value of systematic detection of physical child abuse at emergency rooms: a cross-sectional diagnostic accuracy study. BMJ Open. 2016;6(3):e010788.
- Teeuw AH, Derkx BH, Koster WA, Van rijn RR. Educational paper: Detection of child abuse and neglect at the emergency room. Eur J Pediatr. 2012;171(6):877-85.
- Feldman KW, Tayama TM, Strickler LE, et al. A Prospective Study of the Causes of Bruises in Premobile Infants. Pediatr Emerg Care. 2017. [Epub ahead of print]
- Paul AR, Adamo MA. Non-accidental trauma in pediatric patients: a review of epidemiology, pathophysiology, diagnosis and treatment. Transl Pediatr. 2014;3(3):195-207.
Other FOAMed Resources on Pediatric Physical Abuse
- https://lifeinthefastlane.com/bakers-dozen-bs-of-bashed-baby-badness/
- https://radiopaedia.org/articles/non-accidental-injuries
- https://emergency.unboundmedicine.com/emergency/view/5-Minute_Emergency_Consult/307677/all/Abuse__Pediatric__Nonaccidental_Trauma_[nat]_
A special thanks to TREKK – Translating Emergency Knowledge for Kids for recruiting Dr. Coombs and Dr. Holland for this podcast.






1 thought on “EM Cases: Pediatric Physical Abuse Recognition and Management”
Pingback: Weekly EMNinja Template – EM Ninja