Authors: Jacob Kirkland, MD (EM Resident Physician, UTSW – Dallas, TX); Steve Field, DO (Assistant Professor of EM/Attending Physician, UTSW – Dallas, TX) // Reviewed by: Sophia Görgens, MD (EM Physician, Northwell, NY); Cassandra Mackey, MD (Assistant Professor of Emergency Medicine, UMass Chan Medical School); Alex Koyfman, MD (@EMHighAK)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 41-year-old male with no significant past medical history presents with a deep hand laceration. The patient states they were cutting an avocado when the knife pierced through and punctured his hand. He presented to the emergency department because he is having numbness distal to the site of injury, as well as constant bleeding and some difficulty with flexing his finger. Examination reveals the following:

What is the diagnosis?
Answer: Flexor tendon injury
Epidemiology:
- Secondary to deep penetration with sharp objects or blunt trauma at tendinous attachments to bone2
- Common in young men in manual labor (20-45 years)
- Literature has conflicting data regarding dominance of hand injured2,3
- Usually injured when using a sharp object or catching a falling object
- Overall epidemiology of flexor tendon injuries is not well understood
- Commonly involve nerve injuries2
Anatomy:
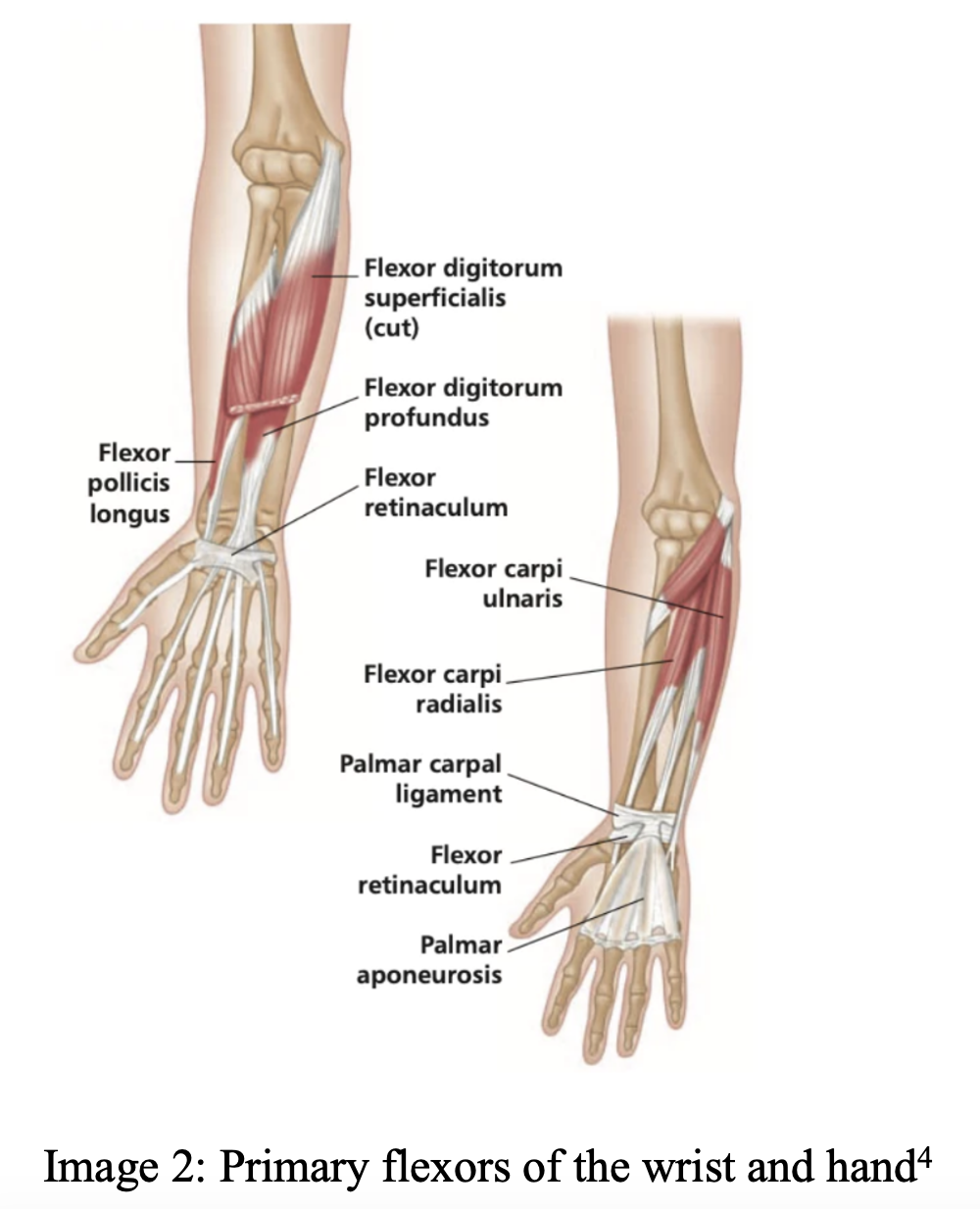
- Deeper compared to extensor tendons–injuries more likely to involve neurovascular structures
- Primary wrist flexors: flexor carpi ulnaris and radialis
- Primary thumb flexors: flexor pollicis longus and brevis
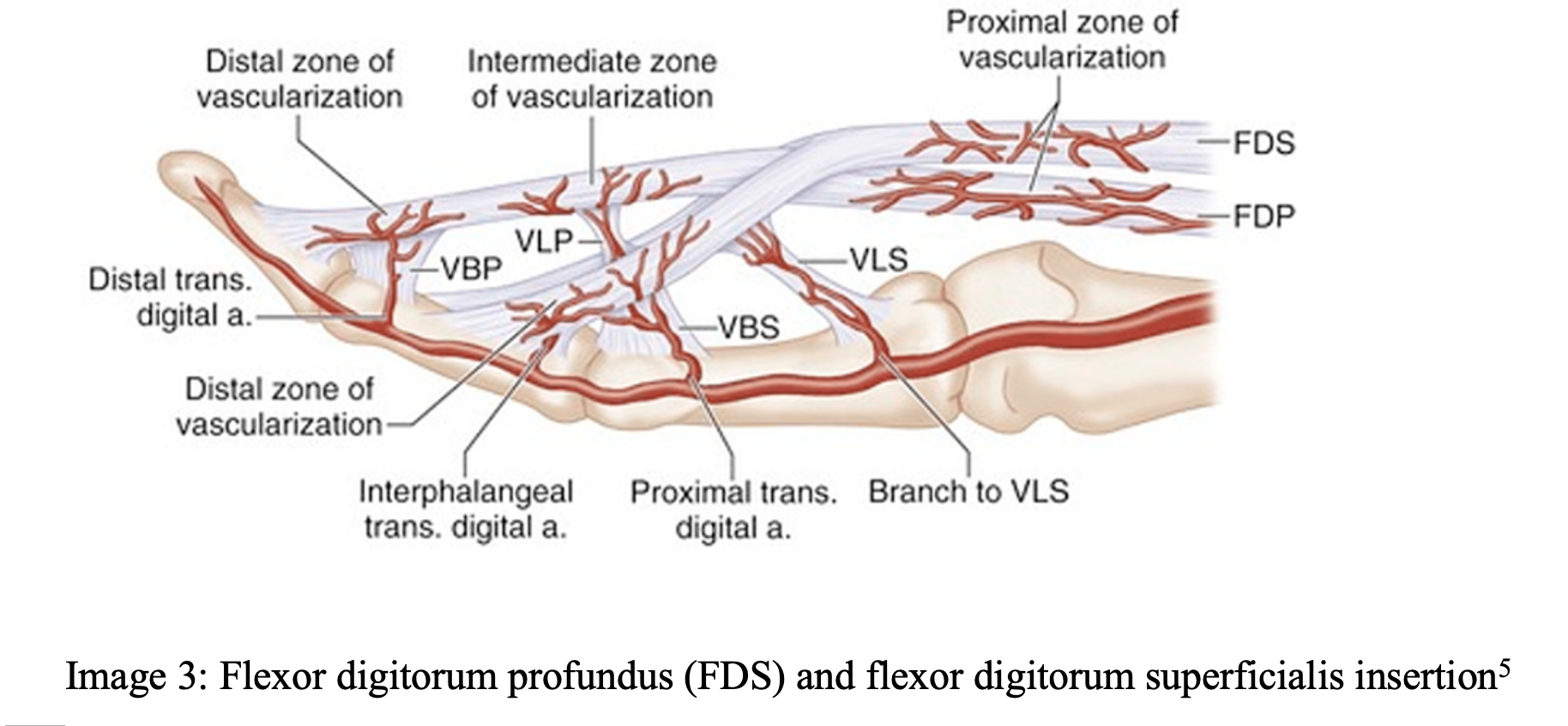
- PIP joint flexor: Flexor digitorum superficialis
- DIP joint flexors: Flexor digitorum profundus
- DIP and PIP flexors operate via a pulley system (Image 4)
Classic injuries:
Jersey finger
- Athlete grabbing for opponent’s jersey
- Forced hyperextension while DIP is in flexion
- Disruption of FDP at distal phalanx (closed injury)6,7
Clinical Presentation:
- Flexor injuries typically from deeper lacerations to the volar surface of the hand
- Loss of flexion strength or motion in effected digit
- Deeper lacerations may have neurovascular injury with loss of sensation or motor control
Evaluation:
- History should include: mechanism, occupation, handedness, time of injury, tetanus status, prior injuries6
- Examine prior to anesthesia to obtain accurate sensorimotor function6
- Isolate each joint to test strength against resistance
- Test for neurovascular deficits with light touch/pinprick sensation, doppler
- Evaluate for bruising, wounds, deformities
- Adequate anesthesia should be used for wound exploration and decontamination
- Evaluate wounds by reducing blood flow and irrigation
- Finger tourniquets should be used6
- Note wounds involving joint spaces or open fractures
- X-ray should be used to identify fractures or retained foreign bodies
- Ultrasound is effective for identifying hand fractures8
- Ultrasound may be useful to evaluate for tendon disruption9
- Evaluate the zone of injury
Zones of injury
- Tendon zones will help identify structures injured and guide further treatment

- Treatment does not vary, however important to identify zone if talking to consultant
- I: Distal to FDS insertion–contains only FDP
- II: FDS insertion to distal palmar crease–contains FDS/FDP
- III: Palm
- IV: Carpal tunnel
- V: Carpal tunnel to forearm
- TI: Distal to thumb interphalangeal (IP) joint
- TII: Base of thumb to IP joint
- TIII: Thenar eminence11
- Zones II-V are the most common areas of injury2, 11
Treatment:
- Disruption of flexor tendons should not be repaired in the ED
- Flexor tendon repair is a difficult, delicate, and precise process that requires operation
- Local hemostasis, pain control with a digital, radial, or medial nerve block depending on location of injury, and wound repair with non-absorbable sutures
- Most patients get a short course of antibiotics in open tendon injuries, but not required
- Several prospective, randomized control trials show no statistical significance in wound infection with hand lacerations12-14
- Cephalexin 500mg for 5-7 days is appropriate for the majority of open tendon injuries if they are otherwise clean
- Consider extensive contamination, open fractures, which would warrant orthopedic consultation
- Type I: open fracture with <1cm clean laceration, minimal soft tissue damage
- Cefazolin 2 g IV three times daily in adults
- 30 mg/kg three times daily in children
- Cefazolin 2 g IV three times daily in adults
- Type II: open fracture with 1-10 cm clean laceration without extensive injury
- Same as Type 1
- Type III: open fracture >10cm with extensive soft tissue damage or heavily contaminated/farm injury
- Cefazoline 2 g IV three times daily
- Gentamicin 5-7 mg/kg IV once daily in adults
- 2.5 mg/kg IV three times daily in pediatrics15
- Type I: open fracture with <1cm clean laceration, minimal soft tissue damage
- Depending on local practice, orthopedics consultation versus urgent referral for definitive repair of lacerations16
- Open fractures of the hand should warrant orthopedic consultation
- When in doubt over extent/degree of injury and disruption of tendons, orthopedic/hand consultation for a definitive plan is reasonable
- If referring, patient will need follow up within 2-3 days for evaluation of extent of injury and possible urgent surgical repair16
- If evaluation in the emergency department and no surgery indicated urgently, sutures to be left in place for 10 days or until sooner evaluation in orthopedics clinic
Pearls
- Flexor tendon injuries should have local wound repair, splinting in flexion, and timely orthopedics follow-up for definitive surgical repair
- Complete a thorough physical exam, noting neurovascular status as well as isolated joint mobility and strength
- Patients generally have local tissue repair, splinting, and outpatient hand specialist follow up, however consider hand consultation if damage is extensive or consider transferring if no hand specialist is available for patient to follow up with
- Consider the closed injury “Jersey finger” in the patient with pain/motor deficit at the DIP

A 23-year-old man presents with 2 days of pain and swelling of his right index finger. He works as a construction worker and scratched his finger 3 days ago on a bolt. His temperature is 100.5°F (38.1°C). His finger appears swollen and is held in slight flexion. The pain is increased with passive extension of the finger. Which of the following structures is most likely infected?
A) Extensor tendon sheath
B) Fingertip pulp
C) Flexor tendon sheath
D) Periosteum
Answer: C
This patient has flexor tenosynovitis, an infection of the flexor tendon sheath. The four cardinal signs (Kanavel criteria) are tenderness of the flexor tendon, symmetrical swelling of the finger, flexed posture of the finger, and pain with passive extension. All four signs may not be present early in the course of illness. Pain with passive extension is the most likely to be present early in the disease. Inoculation usually occurs by penetrating injury, which seeds the tendon sheath. Management consists of intravenous antibiotics, and hand surgery should be consulted to consider operative debridement. Unrecognized or persistent infection can lead to necrosis of the tendon.

There are no extensor tendon sheaths (A) in the hand. Therefore, the extensor tendons are less susceptible to infection. Infection of the periosteum (D) is present in osteomyelitis. Given the presence of three out of four of the cardinal signs, this patient is more likely to have flexor tenosynovitis. Felons are infections of the fingertip pulp (B). This would be characterized by localized infection of the palmar aspect of the distal phalanx.
References:
- Park CW, Juliano ML, Woodhall D. Tendon Lacerations. In: Knoop KJ, Stack LB, Storrow AB, Thurman R. eds. The Atlas of Emergency Medicine, 5e. McGraw Hill; 2021. Accessed June 24, 2023.
- Stevens KA, Caruso JC, Fallahi AKM, Patiño JM. Flexor Tendon Lacerations. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 5, 2023.
- Çalışkan Uçkun A, Yurdakul FG, Ergani HM, et al. Factors predicting reoperation after hand flexor tendon repair. El fleksör tendon onarımı sonrası reoperasyonu öngören faktörler. Ulus Travma Acil Cerrahi Derg. 2020;26(1):115-122. doi:10.14744/tjtes.2019.92590
- Kuttner, J. Stretching the Wrist Flexors. NielAsher. November 9, 2021. Accessed June 10, 2023. https://nielasher.com/blogs/video-blog/stretching-the-wrist-flexors
- Alkandari A F, Alawadhi A, Alawadhi F A, et al. (January 29, 2023) Isolated Flexor Digitorum Profundus Injuries in Flexor Zone II of the Hand: A Report of Five Cases. Cureus 15(1): e34360. doi:10.7759/cureus.34360
- Hile D, Hile L. The emergent evaluation and treatment of hand injuries. Emerg Med Clin North Am. 2015;33(2):397-408. doi:10.1016/j.emc.2014.12.009
- Scalcione LR, Pathria MN, Chung CB. The athlete’s hand: ligament and tendon injury. Semin Musculoskelet Radiol. 2012;16(4):338-349. doi:10.1055/s-0032-1327007
- Zhao W, Wang G, Chen B, et al. The value of ultrasound for detecting hand fractures: A meta-analysis. Medicine (Baltimore). 2019;98(44):e17823. doi:10.1097/MD.0000000000017823
- Rosskopf AB, Martinoli C, Sconfienza LM, et al. Sonography of tendon pathology in the hand and wrist. J Ultrason. 2021;21(87):e306-e317. doi:10.15557/JoU.2021.0052
- Bates S. Flexor Tendon Anatomy. Medscape. April 9, 2013. Accessed June 4, 2023. https://emedicine.medscape.com/article/1245236-overview
- Venkatramani H, Varadharajan V, Bhardwaj P, Vallurupalli A, Sabapathy SR. Flexor tendon injuries. J Clin Orthop Trauma. 2019;10(5):853-861. doi:10.1016/j.jcot.2019.08.005
- Grossman JAI, Adams JP, Kunec J. Prophylactic Antibiotics in Simple Hand Lacerations. 1981;245(10):1055–1056. doi:10.1001/jama.1981.03310350043021
- Roberts AH, Teddy PJ. A prospective trial of prophylactic antibiotics in hand lacerations. Br J Surg. 1977;64(6):394-396. doi:10.1002/bjs.1800640605
- Haughey RE, Lammers RL, Wagner DK. Use of antibiotics in the initial management of soft tissue hand wounds. Ann Emerg Med. 1981;10(4):187-192. doi:10.1016/s0196-0644(81)80159-x
- Levine BJ. Open Fracture. In: EMRA Antibiotic Guide. Emergency Medicine Residents’ Association; 2022:10-11.
- Roberts, James R. MD. ED Treatment of Flexor Tendon Injuries. Emergency Medicine News 33(12):p 8,9, December 2011. | DOI: 10.1097/01.EEM.0000410106.40227.cc








