Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 3-year-old male with no past medical history presents to the ED with one week of daily fevers >102°F associated with four days of rash on the trunk. His parents have been managing his fevers with acetaminophen and ibuprofen, but became worried today when they noticed redness and swelling of the tongue in addition to swelling in the hands and feet. Vital signs demonstrate a rectal temperature 39.5°C, BP 92/60, HR 130, RR 35, and SpO2 of 98%. Physical exam demonstrates an ill appearing child with bilateral conjunctival injection; erythematous tongue with dry, fissured lips; right sided cervical lymphadenopathy; an erythematous maculopapular rash on the chest, abdomen, and back; and nonpitting edema of the hands and feet. What is the most likely diagnosis?
What is the most likely diagnosis?
Answer: Kawasaki Disease (KD)
Epidemiology:
- Occurs most commonly in those between the ages 6 months to 5 years of age, with peak at 18-24 months1
- Highest rate of incidence in children of East Asian and Pacific Islander descent2
- The most common cause of acquired heart disease in children in developed countries2
- Coronary arteritis and coronary artery aneurysms occur in up to 30% of untreated children, and up to 5-7% of treated children3
- Originally described in Japan by Dr. Tomisaku Kawasaki, who noticed 50+ similar pediatric presentations between the years 1961 and 1967. Upon further research in the 1970’s, retrospective data from autopsies of those patients showed coronary aneurysms5
Pathophysiology:
- Kawasaki Disease is a vasculitis of medium sized arteries. It can especially affect the coronary arteries during the acute febrile phase2
- Damage to blood vessels is caused by infiltration of inflammatory cells causing breakdown of the elastin and collagen that provides structure to the arterial wall. This leads to dilatation and formation of aneurysms4
- Large body of research has been unable to find a specific cause of KD, however there is a suggestion of genetic predisposition as well as association with preceding infection (though no specific bacterial or viral cause has been found)4
- Often occurs in epidemics, with spatial and temporal clustering of cases4
Clinical Presentation:
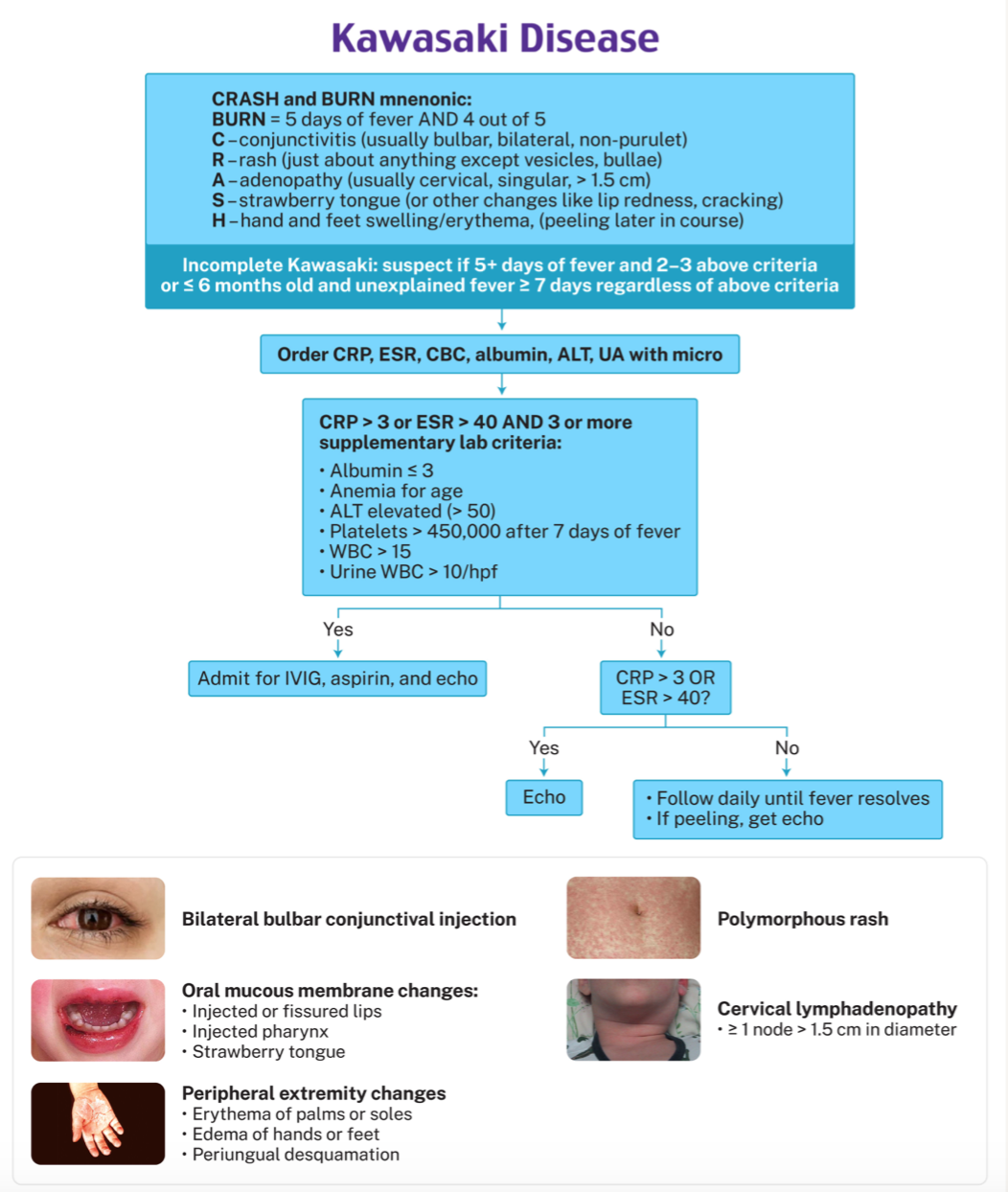
- Diagnosis of KD requires fever for 5 days, PLUS 4 out of 5 of the following criteria:5,6
- Conjunctival injection (>75%)
- Erythematous rash, most commonly involving trunk and extremities and maculopapular (70-90%)
- Lymphadenopathy, usually cervical (25-70%)
- Mucosal changes, including glossitis and/or dry, fissured lips (90%)
- Extremity changes, can include erythema, induration, and in late stages desquamation (50-85%)
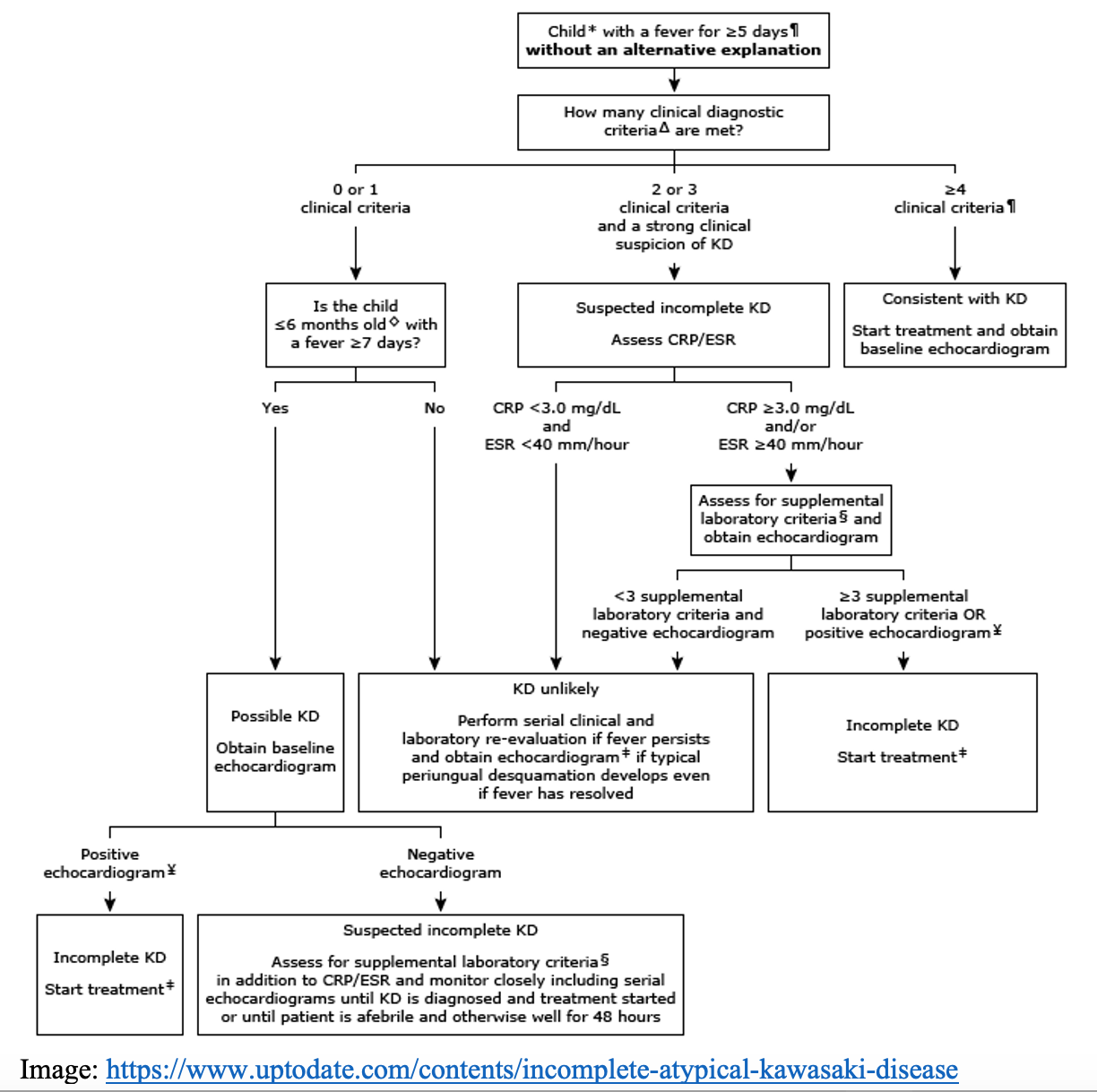
- Diagnosis of incomplete Kawasaki Disease also usually consists of fever for 5 days PLUS 2 or 3 of the following:8
- Conjunctival injection à most common findings in incomplete KD (>90%)
- Erythematous rash, most commonly involving trunk and extremities and maculopapular à (50% do not have rash for incomplete KD)
- Lymphadenopathy, usually cervical à (90% do not have adenopathy for incomplete KD)
- Mucosal changes, including glossitis and/or dry, fissured lips
- Extremity changes, can include erythema, induration, and in late states desquamation à (40% do not have finding in incomplete KD)
- There are some cases found in the literature where the other criteria are met but the child does not have a fever and still meets the definition of incomplete KD8
- In addition, incomplete KD should be suspected in patients less than six months of age with unexplained fever ≥7 days, even if they have no clinical findings of KD7

- Up to 10% of children who develop coronary artery aneurysms never meet criteria for KD, thus the American Heart Association (AHA) and American Academy of Pediatrics (AAP) created an algorithm to help clinicians identify patients that require treatment. Early consultation with a specialist is recommended in these cases7,8
Workup:
- Lab tests can support the diagnosis of KD, especially in incomplete KD cases as above.8
- CBC with differential
- WBC > 15,000/microL
- Normocytic, normochromic anemia
- Platelets > 450,000/microL
- LFTs – ALT > 50 units/L
- CRP > 3mg/dL
- ESR > 40 mm/hour
- UA – Sterile pyuria >10 WBCs/hpf
- CBC with differential
- Formal echocardiography should be performed in all patients meeting criteria for KD7
- Initial coronary artery diameter is a factor in identifying patients at high risk for development of coronary artery aneurysm
- Patients will need repeat echocardiograms 1-2 weeks after treatment, then 4-6 weeks after treatment to monitor for cardiac sequelae3
- Early consultation is recommended with pediatric cardiology, infectious disease, and rheumatology. Consider transfer to a pediatric center at this time
Differential Diagnosis:8
- Viral infections including EBV, CMV, Adenovirus, HHV-6, MISC
- Toxic shock syndrome secondary to staphylococcal or streptococcal infections
- Drug reaction, including SJS
- Sepsis
- Systemic juvenile idiopathic arthritis
Treatment:
- IVIG 2g/kg x1 dose administered over 8-12 hours9
- Aspirin 30 to 50 mg/kg/day orally in four divided doses9
Disposition:
- Patients require admission if KD is diagnosed or suspected9
- Incomplete KD patients who do not get started on treatment will need either repeat lab work or an echocardiogram to confirm diagnosis
- If started on IVIG, patients are observed for 24 hours after completion of IVIG to confirm resolution of fever9
Pearls:
- Consider Kawasaki Disease in any child presenting with fever for 5 or more days
- If the criteria are met, consult pediatric rheumatology and/or infectious disease and start IVIG + aspirin
- Patients with suspected KD need an echocardiogram to identify cardiac sequelae

A 3-year-old boy presents to the ED with a fever. He has had a high fever of > 103°F (39.4°C) for the past week. On physical exam, you note left-sided cervical lymphadenopathy, fissuring of the lips, conjunctival injection without drainage, and a diffuse faint maculopapular rash. Which of the following is the most appropriate treatment for this patient?
A) Broad-spectrum antibiotics
B) High-dose methylprednisolone
C) Immune globulin and high-dose aspirin
D) Low-dose aspirin
Answer: C
This patient is exhibiting signs and symptoms consistent with Kawasaki disease (mucocutaneous lymph node syndrome). Kawasaki disease most commonly affects children < 5 years. It is the leading cause of acquired heart disease in resource-rich areas of the world, surpassing rheumatic heart disease. It has a slight male predominance. Management of Kawasaki disease includes high-dose aspirinand intravenous immune globulin (IVIG). Corticosteroids are controversial and not currently recommended. Patients should be admitted to the hospital and cardiology consulted early in their course.
Signs and symptoms of Kawasaki disease include fever for > 5 days, unilateral cervical lymphadenopathy > 1.5 cm, mucous membrane involvement (e.g., strawberry tongue or fissured lips), extremity changes (e.g. edema or erythema), bilateral nonexudative conjunctivitis without iritis, and nonvesicular rash. Diagnosis is clinical. Fever > 5 days must be present and at least 4 of the 5 aforementioned signs. If there are < 4 signs present, diagnosis may be made with evidence of coronary artery disease on echocardiography or by a constellation of laboratory tests. Imaging includes echocardiography to evaluate for complications related to Kawasaki disease, including coronary artery aneurysms, valvular incompetence, ventricular wall motion abnormalities, or pericardial effusion. Coronary artery aneurysms are detected in 25% of untreated and 5–10% of treated patients and may result in myocardial infarction or congestive heart failure. Laboratory testing may reveal thrombocytosis, sterile pyuria, leukocytosis with left shift, anemia, elevated C-reactive protein and erythrocyte sedimentation rate, and abnormal liver function tests.
Broad-spectrum antibiotics (A) are not necessary to treat Kawasaki disease. High-dose methylprednisolone (B) is not currently recommended, as steroids for Kawasaki disease are controversial. Low-dose aspirin (D) would not fully treat Kawasaki disease as high-dose aspirin is required. This is the only situation in which aspirin is recommended for administration in children, as the benefits outweigh the risks of Reye syndrome.
FOAMed:
- https://www.emdocs.net/em-in-5-kawasaki-disease/
- https://www.nuemblog.com/blog/kawasaki-disease
- https://wikem.org/wiki/Kawasaki_disease
References:
- Noorani, M., Lakhani, N. Kawasaki disease: two case reports from the Aga Khan Hospital, Dar es Salaam-Tanzania. BMC Pediatrics. 2018;18(334).https://doi.org/10.1186/s12887-018-1306-5
- McCrindle, B., Rowley, A., Newburger, J., et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. 2017;135(17):e927-e999. https://doi.org/10.1161/CIR.0000000000000484
- Rivas, M., Arditi, M. Kawasaki disease: pathophysiology and insights from mouse models. Nature Reviews Rheum. 2020;16:391-405. https://doi.org/10.1038/s41584-020-0426-0
- Sundel, R. Kawasaki disease: epidemiology and etiology. In: Post TW, ed. UpToDate;2022. Accessed December 31, 2022. https://www.uptodate.com/contents/kawasaki-disease-epidemiology-and-etiology
- Ramphul, K., Mejias, S. Kawasaki disease: a comprehensive review. Arch Med Sci Atheroscler Dis. 2018; 3: e41-e45. https://doi.org/10.5114/amsad.2018.74522
- Clinical Practice Guidelines: Kawasaki Disease. The Royal Children’s Hospital Melbourne. Updated January 2021. Accessed December 31, 2022.
- Sundel, R. Kawasaki disease: clinical features and diagnosis. In: Post TW, ed. UpToDate;2022. Accessed December 31, 2022. https://www.uptodate.com/contents/kawasaki-disease-clinical-features-and-diagnosis
- Sundel, R. Incomplete (atypical) Kawasaki disease. In: Post TW, ed. UpToDate;2022. Accessed December 31, 2022. https://www.uptodate.com/contents/incomplete-atypical-kawasaki-disease
- Sundel, R. Kawasaki disease: Initial treatment and prognosis. In: Post TW, ed. UpToDate;2022. Accessed December 31, 2022. https://www.uptodate.com/contents/kawasaki-disease-initial-treatment-and-prognosis









1 thought on “EM@3AM: Kawasaki Disease”
Pingback: Nerdfallmedizin.de - Nerdwoche am 02.07.2023