Author: Rachel Bridwell, MD (@rebridwell, EM Resident Physician, San Antonio, TX) // Reviewed by: Brit Long, MD (@long_brit, EM Attending Physician, San Antonio, TX) and Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 65-year-old with a history of end stage renal disease from diabetes status post renal transplant, hyperlipidemia, and hypertension presents to the emergency department with lower abdominal pain and fevers. It started gradually over the past few days with nausea and emesis. His urine also looks “different”. On exam, his vitals include HR 112, BP 101/62, RR 22, T 101.1, SpO2 98% on RA. His is tachycardic with lower extremity edema and lower abdominal tenderness to palpation.
What’s the next step in your evaluation and treatment?
Answer: Infected Renal Graft1-20
Epidemiology:
- Renal transplant is most common solid organ transplant seen in ED visits, accounting for 73% between combined organ transplant and renal transplant1
- Both cadaveric and living donation1
- 1 year survival for kidney transplants is 96%, thus renal transplant is the most commonly seen solid organ transplant in the ED2
- Diabetes with or without hypertension is the most common reason for renal transplant, accounting for 75.6% of cases
- Other etiologies: acquired renal disorder (glomerulonephritis, SLE, sickle cell anemia, drug induced nephropathy), congenital anomalies1
- Obesity is an independent risk factor for surgical and postoperative complication in renal transplant complications3
Anatomy:
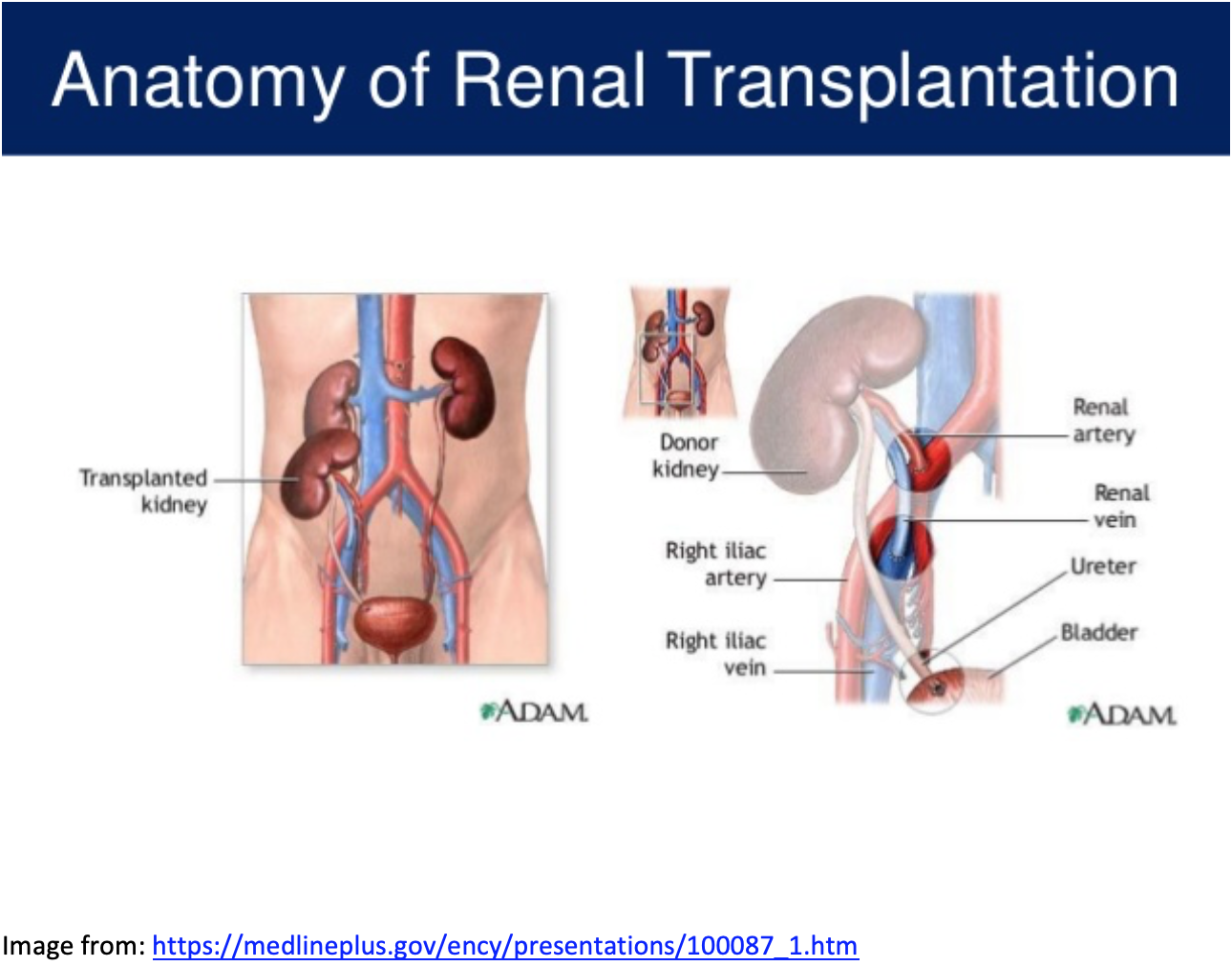
- Located in either R>L iliac fossa (~90% in R)4
- Superior mesenteric artery most commonly affected by embolic events secondary to 45 degree angle departure from aorta, which perfuses duodenum to transverse colon5
Complications:
- Infection
- Over 42 months post-transplant, 43% of patients develop UTIs6
- Inherently classified as complicated due to presence of transplant
- Significantly higher in females (68%) vs males (30%)6
- Higher rates of UTIs in cadaveric vs live donor6
- UTIs increase complications (including failure and rejection) by 2-3x7
- Vascular
- Renal artery stenosis, AV Fistulae, Pseudoaneurysms, Arterial kinking, fibromuscular dysplasia8
- Renal vein thrombosis, occurring in 0.5-4% of transplants, represents a dramatic early complication4
- Low incidence, though important cause of graft loss within first months4
- Rare renal torsion events, especially if retroperitoneal or in pediatrics9
- Renal vein thrombosis, occurring in 0.5-4% of transplants, represents a dramatic early complication4
- Surgical complications include infection, venous thromboembolism, pneumonia
- 12-15% incidence10
- Renal artery stenosis, AV Fistulae, Pseudoaneurysms, Arterial kinking, fibromuscular dysplasia8
- Over 42 months post-transplant, 43% of patients develop UTIs6
Clinical Presentation:
- Most frequent ED chief complaints:
- 3% abdominal complaints/GI
- 7% infectious
- 9% cardiovascular
- % neurologic
- 7% lab abnormalities
- 8% urinary
- 3% not otherwise specified
- Most common symptom of infection is fever, though in up to ½ of patients, fever may not be present11
Evaluation:
- Assess ABCs and VS—may be normal on early presentation but will progress to tachycardia, hypotension, and fever12
- Perform a complete physical examination:
- Palpate over transplant site, usually lower in the pelvis
- CV: high rate of cardiovascular disease in these patients and contributes to kidney perfusion13
- Laboratory evaluation: CBC, CMP, lactate, UA, Urine culture
-
-
- Most common pathogens on urine culture:
- E. coli 29%
- Enterococcocus 24%
- Staphylococcus 12%
- Klebsiella 10%
- Pseudomonas 4%
- Streptococcus 4%
- Fungal 5%
- Most common pathogens on urine culture:
-
- Imaging:
-
-
- CT:
- Can assess for structural changes, impingement, extra-renal pathology
- Contrast load may be relatively contraindicated in renal insufficiency
- Ultrasound: sensitivity 87-94% and specificity 86-100%, limited by operator experience14,15
- Evaluate for renal vein thromboses, fibromuscular dysplasia, hematoma formation, torsion9
- If performed by trained radiologist, can perform doppler of iliacs proximal and distal to anastomosis
- Other:
- Digital subtraction angiography (DSA), spatial labeling with multiple inversion pulses (SLEEK) magnetic resonance, magnetic resonance imaging (MRI) should be deferred for inpatient workup8,16
- These are found to be reliable methods of evaluating anatomic and vascular complications, avoiding some contrast loads8
- Of note, MR with contrast in renally insufficient patients may result in nephrogenic systemic fibrosis8
- DSA (MRI technology) has 100% sensitivity and 86-90% specificity16
- Digital subtraction angiography (DSA), spatial labeling with multiple inversion pulses (SLEEK) magnetic resonance, magnetic resonance imaging (MRI) should be deferred for inpatient workup8,16
- CT:
-
Treatment:
-
- IV fluids
- If suspected infection, early infectious disease consult improves mortality17
- Consult transplant physician
- Monitor urine output
- If hematoma, may require ultrasound guided percutaneous drainage4
- Stenosis and fistulae require operative management4
- Urinary tract infections: high resistance rate of trimethoprim-sulfamethoxazole (TMP-SMX), and ciprofloxacin13
- Post-transplant, patients receive TMP-SMX (Bactrim) as P. jirovecii pneumonia prophylaxis for 6 months, also acts as urinary tract infection treatment, and is first line in UTIs in transplant patients7,13
- 10% will develop extended spectrum beta lactam resistant urinary tract infections18
- Gastroenteritis is a common complaint in renal transplant recipients presenting to the ED, 27%19
Disposition:
- Early consultation with transplant team
- Vascular surgery may be needed for stenosis or thrombosis of renal vasculature20
- Of these patients presenting to ED, up to 30% require nephrology consult19
- High admission rates, approximately 57%1,11
Pearls:
- Call transplant surgeon early
- Cadaveric transplants have highest rates of inherently complicated UTIs with high resistance6
- Screen with US for vascular complications which may require inpatient further imaging and workup
- Over half of these patients get admitted
Further Reading:
#FOAMed
emDocs Transplant Infection, Rejection, and Medication Effects
emDocs Transplant Organ Specific Complications
References/Further Reading:
- Unterman S, Zimmerman M, Tyo C, et al. A descriptive analysis of 1251 solid organ transplant visits to the emergency department. West J Emerg Med. 2009;10(1):48-54. http://www.ncbi.nlm.nih.gov/pubmed/19561769. Accessed October 22, 2019.
- Morris PJ. Transplantation – A medical miracle of the 20th century. N Engl J Med. 2004;351(26):2678-2680. doi:10.1056/NEJMp048256
- Di Cocco P, Okoye O, Almario J, Benedetti E, Tzvetanov IG, Spaggiari M. Obesity in Kidney Transplantation. Transpl Int. October 2019:tri.13547. doi:10.1111/tri.13547
- Hernández-Guedea M, Reyna-Sepúlveda F, Ponce-Escobedo A, et al. International Journal of Organ Transplantation Medicine Outcomes and Surgical Complications in Kidney Transplantation. www.ijotm.com. Accessed November 1, 2019.
- Oldenburg WA, Lau LL, Rodenberg TJ, Edmonds HJ, Burger CD. Acute Mesenteric Ischemia. Arch Intern Med. 2004;164(10):1054. doi:10.1001/archinte.164.10.1054
- Chuang P, Parikh CR, Langone A. Urinary tract infections after renal transplantation: a retrospective review at two US transplant centers. Clin Transplant. 2005;19(2):230-235. doi:10.1111/j.1399-0012.2005.00327.x
- Lee H, Le J. Urinary Tract Infections. In: PSAP Book 1. ; 2018:1-22. https://www.accp.com/docs/bookstore/psap/p2018b1_sample.pdf. Accessed November 3, 2019.
- Tang H, Wang Z, Wang L, et al. Depiction of transplant renal vascular anatomy and complications: Unenhanced MR angiography by using spatial labeling with multiple inversion pulses. Radiology. 2014;271(3):879-887. doi:10.1148/radiol.14131800
- Winter TC, Clarke AL, Campsen J. Acute torsion of a retroperitoneal renal transplant mimicking renal vein thrombosis. Ultrasound Q. 2013;29(3):203-204. doi:10.1097/RUQ.0b013e31829d35cf
- Eufrásio P, Parada B, Moreira P, et al. Surgical complications in 2000 renal transplants. In: Transplantation Proceedings. Vol 43. ; 2011:142-144. doi:10.1016/j.transproceed.2010.12.009
- Tokalak I, Başaran Ö, Emiroǧlu R, Karakayali H, Bilgin N, Haberal M. Problems in postoperative renal transplant recipients who present to the emergency unit: Experience at one center. In: Transplantation Proceedings. Vol 36. Elsevier USA; 2004:184-186. doi:10.1016/j.transproceed.2003.11.035
- Acosta S, Block T, Björnsson S, Resch T, Björck M, Nilsson T. Diagnostic Pitfalls at Admission in Patients with Acute Superior Mesenteric Artery Occlusion. J Emerg Med. 2012;42(6):635-641. doi:10.1016/J.JEMERMED.2011.03.036
- Senger SS, Arslan H, Azap ÖK, Timurkaynak F, Çağır Ü, Haberal M. Urinary Tract Infections in Renal Transplant Recipients. Transplant Proc. 2007;39(4):1016-1017. doi:10.1016/j.transproceed.2007.02.060
- Pappas P, Zavos G, Kaza S, et al. Angioplasty and Stenting of Arterial Stenosis Affecting Renal Transplant Function. Transplant Proc. 2008;40(5):1391-1396. doi:10.1016/j.transproceed.2008.04.016
- Loubeyre P, Abidi H, Cahen R, Minh VAT. Transplanted renal artery: Detection of stenosis with Color Doppler US. Radiology. 1997;203(3):661-665. doi:10.1148/radiology.203.3.9169685
- Zhang LJ, Peng J, Wen J, et al. Non-contrast-enhanced magnetic resonance angiography: a reliable clinical tool for evaluating transplant renal artery stenosis. Eur Radiol. 2018;28(10):4195-4204. doi:10.1007/s00330-018-5413-3
- Hamandi B, Husain S, Humar A, Papadimitropoulos EA. Impact of infectious disease consultation on the clinical and economic outcomes of solid organ transplant recipients admitted for infectious complications. Clin Infect Dis. 2014;59(8):1074-1082. doi:10.1093/cid/ciu522
- Alevizakos M, Nasioudis D, Mylonakis E. Urinary tract infections caused by ESBL-producing Enterobacteriaceae in renal transplant recipients: A systematic review and meta-analysis. Transpl Infect Dis. 2017;19(6):e12759. doi:10.1111/tid.12759
- Uysal E, Dokur M, Bakir H, Ikidag MA, Kirdak T, Kazimoglu H. The Reasons of Renal Transplant Recipients’ Admission to the Emergency Department; a Case Series Study. Emergency. 2016;4(4):207.
- Khaja MS, Matsumoto AH, Saad WE. Complications of Transplantation. Part 1: Renal Transplants. Cardiovasc Intervent Radiol. 2014;37(5):1137-1148. doi:10.1007/s00270-014-0851-z








