Author: Brit Long, MD (@long_brit, EM Attending Physician, San Antonio, TX) // Edited by: Alex Koyfman, MD (@EMHighAK)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
An 28-year-old male presents after high-speed MVC with facial pain and loss of consciousness. He does not remember too much, but does recall falling asleep. The next thing he knew, he woke behind the wheel. He had run into a metal traffic guard at the end of an intersection.
Triage vital signs (VS): BP 130/75, HR 82, RR 16, SpO2 96% on RA. He has severe facial pain and bruising, conjunctival hemorrhage bilaterally, and facial paresthesias.
What is the patient’s diagnosis? What’s the next step in your evaluation?
Answer: Le Fort Fracture
Background: Le Fort fractures include fractures of the midface.
- Named for the French surgeon Rene Le Fort, who evaluated these fractures by causing blunt trauma to cadavers.
- Bones include the maxilla, orbital rims, zygoma.
- All fractures will include the pterygoid processes of the sphenoids, which provide midface support.
Epidemiology:
- These are typically caused by trauma, with the mechanism of injury determining grade of injury. Most common cause of injury is MVC.
- Low-velocity mechanisms most commonly cause Le Fort I fractures, which account for over 50% of Le Fort fractures. Mechanisms include fall from standing or blunt trauma to the face.
- High-velocity mechanisms may result in high grade fractures, including type II and III. Mechanisms include high fall and high-speed MVC.
- A variety of other injuries are common with high grade Le Fort fractures, including skull fracture, head injury, and C-spine injury. Skull fracture occurs in 40% of these patients.
Classification System:
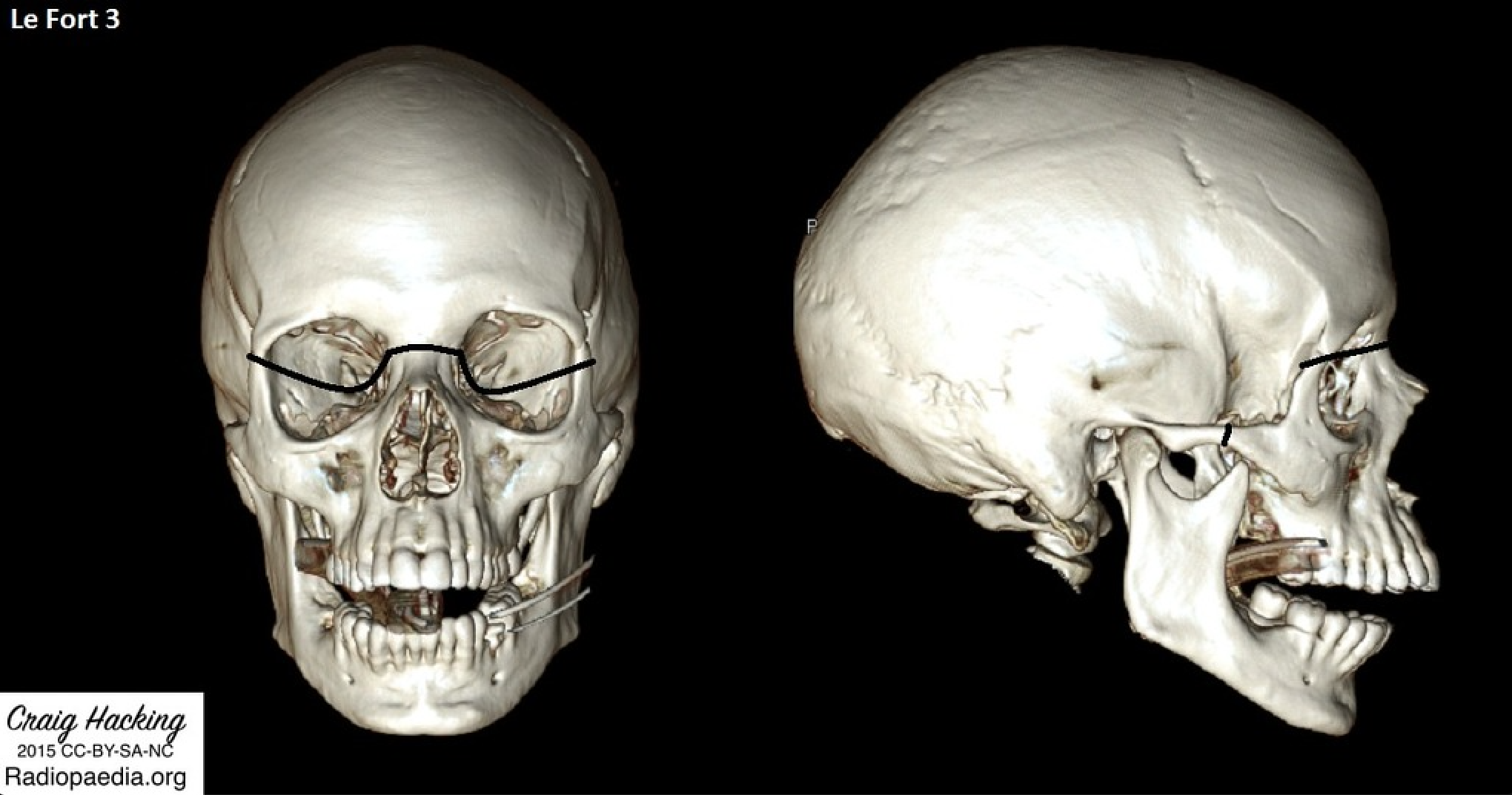
- There are three types, primarily dependent on the bones fractured and injury plane (images below from Radiopaedia).
- Type I: Transverse fracture through maxilla, occurring above roots of the teeth. The body of the maxilla is separated from the pterygoid plate and nasal septum. The maxilla and hard palate may be mobile. May occur with malocclusion, dental fractures. This fracture is usually stable.

- Type II: Fracture which extends superiorly and through central maxilla and hard palate. The nasal bridge, maxilla, lacrimal bones, orbital floors, and orbital rims are involved. These are bilateral and resemble triangles. The hard palate and nose are moveable, but not the eyes/orbits. This can be unstable or stable.

- Type III: Rare fracture. Involves bridge of nose, medial orbital walls, lateral orbital walls, maxilla, and zygomatic arch. Entire face is unstable and may move. Lateral view of face may demonstrate “dish face” deformity, in which the central structures of the face “cave in”. This fracture is unstable.
- Type IV: Type III plus frontal bone involvement, which is unstable.
Evaluation
- Patients may present with facial bruising, nasal/oral bleeding, CSF rhinorrhea, hemotympanum, conjunctival hemorrhage, inability to smell, facial and nose disfiguration, facial emphysema, raccoon eyes, auricular hematoma, dental injuries, asymmetric pupils, exophthalmos.
- Important questions to ask the patient include: What areas hurt? What looks different when you look in the mirror? How is your vision? Any changes in your vision? Is your bite normal? Is there any tingling or numbness in your face? Have you noticed bleeding from your eyes, ears, and/or nose? Any voice changes? Any neck pain or loss of consciousness?
- Palpate face for tenderness, crepitus, and/or instability, which can detect fractures.
- Stabilize forehead the one hand, grasp teeth/hard palate with the other, and attempt to move the hard palate. If mobility is discovered, attempt to determine the level and specific areas that are mobile.
- Evaluate for C-spine injuries.
Management:
- In the patient with multisystem and/or severe injuries, address your primary survey first and stabilize the patient.
- If the airway is at risk, consider awake intubation, and prepare for a difficult airway.
- Only after the primary survey and resuscitation should you perform your ocular and facial exam in the setting of suspected Le Fort Fractures.
- Control hemorrhage of the nose/oral cavity. Anterior packing may be needed. Avoid posterior packing due to risk of skull base injuries.
- Elevate head of bead to 40-60 degrees.
- Provide IV antibiotics for sinus fractures and/or suspected CSF leaks.
Imaging
- Obtain facial CT, which images the orbits. Also obtain head CT due to high risk of intracranial injuries.
- If concern for C-spine injury is present or the patient is altered, obtain C-spine CT due to high risk of C-spine injuries. CTA of the neck is recommended by some algorithms to evaluate for craniocervical dissection.
- Plain radiographs do not have sufficient sensitivity to exclude these injuries and are not recommended.
Disposition
- Most patients with Le Fort fractures will have other injuries and will be admitted. Grade of Le Fort Fracture is associated with severity of other injuries based on Injury Severity Scale.
- If an isolated stable Le Fort I or II fracture is found, the patient may be appropriate for discharge with specialist follow up.
- Discuss patient with facial trauma team, which may include oral maxillofacial surgery or otolaryngology.
- If CSF leak is found, discuss with neurosurgery.

Which bone is fractured in all types of Le Fort fractures?
A) Ethmoid bone
B) Nasal bone
C) Pterygoid plates
D) Zygoma
Answer: C
The Le Fort classification system attempts to differentiate midfacial fractures, which account for up to 20% of all facial fractures. In 1901, René Le Fort described three predominant midfacial injury patterns. Each type involves separation of a portion of the midface from the skull base. The pterygoid plates, of the sphenoid bone, must be fractured to diagnose any type of Le Fort fracture. The Le Fort I fracture is a horizontal maxillary fracture with the fracture line passing from the nasal septum to the pterygoid plate, leading to a free-floating palate. The Le Fort II fracture is a pyramidal fracture from the nasal bridge crossing the orbital rim through the maxilla to the pterygoid plates, resulting in a free-floating maxilla (and nose). The Le Fort III fracture is a transverse fracture from the nasal bridge across the orbit and zygomatic arch/frontozygomatic suture to the pterygoid plates and the base of the sphenoid, leading to a free-floating face and thus also termed craniofacial disjunction. A high-resolution computed tomography (CT) scan of the face with axial and coronal slices, and if possible, with 3D reconstruction, is ideal to define these complex fractures. Due to the reality of present-day high-speed, high-impact mechanisms in trauma from motor vehicle crashes, sports injuries, and other causes, most fractures will be a combination of more than one Le Fort type. Patients with Le Fort fractures often present dramatically and with significant hemorrhage. Therefore, aggressive protection of the airway is of primary concern. In the field and prehospital setting, it is generally safer to allow a conscious, talking patient to sit up leaning forward to protect their own airway instead of making an attempt to secure a difficult airway with limited resources and backup. Once in the emergency department, the practitioner can determine whether to proceed with intubation or whether a primary cricothyrotomy may be necessary. Le Fort fractures require admission and usually surgical repair.

The ethmoid bone (A) is involved in Le Fort type III fractures. The nasal bone (B) is fractured along the nasofrontal suture in Le Fort types II and III. Although Le Fort type I involves injury to the nasal septum, it does not involve the nasal bone. The zygoma (D) is affected in Le Fort types II and III fractures.
Further Reading:
FOAMed:
References:
- Tintinalli JE, Stapczynski JS, Ma OJ, Cline D, Meckler GD, Yealy DM. Tintinalli’s emergency medicine : a comprehensive study guide. Eight edition. ed. New York: McGraw-Hill Education; 2016.
- Marx JA, Rosen P. Rosen’s emergency medicine : concepts and clinical practice. 8th ed. Philadelphia, PA: Elsevier/Saunders; 2014.
- Phillips BJ, Turco LM. Le Fort Fractures: A Collective Review. Bull Emerg Trauma. 2017;5(4):221-30.
- Salonen EM, Koivikko MP, Koskinen SK. Multidetector computed tomography imaging of facial trauma in accidental falls from heights. Acta Radiol. 2007;48(4):449-55.
- Soong PL, Schaller B, Zix J, et al. The role of postoperative prophylactic antibiotics in the treatment of facial fractures: a randomised, double-blind, placebo-controlled pilot clinical study. Part 3: Le Fort and zygomatic fractures in 94 patients. Br J Oral Maxillofac Surg. 2014;52(4):329-33.
- Bagheri SC, Holmgren E, Kademani D, et al. Comparison of the severity of bilateral Le Fort injuries in isolated midface trauma. J Oral Maxillofac Surg. 2005;63(8):1123-9.
- Hasler RM, Exadaktylos AK, Bouamra O, et al. Epidemiology and predictors of cervical spine injury in adult major trauma patients: a multicenter cohort study. J Trauma Acute Care Surg. 2012;72(4):975-81.








