Authors: Veronica Morgan, MD (EM Resident Physician: UTSW – Dallas, TX); Andrew Stricklin, MD (Assistant Professor of EM/Attending Physician: UTSW – Dallas, TX) // Reviewed by: Sophia Görgens, MD (EM Resident Physician, Zucker-Northwell NS/LIJ, NY); Cassandra Mackey, MD (Assistant Professor of Emergency Medicine, UMass Chan Medical School); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 75-year-old male with past history of HTN, CVA, DM II presents to the emergency department with right facial swelling since last night. He is also complaining of pain and subjective fevers.
Initial vital signs include BP of 150/85, HR 103, T 100.8, RR 18, SpO2 97% on RA. Exam reveals the patient to be ill-appearing with a focal area of swelling medially to his right ear that is warm and tender to palpation. His oral mucosa is dry. He has multiple dental caries and poor dentition overall. Massage of the area of swelling reveals purulent drainage from the oral mucosa near the right maxillary molars. The submandibular space is noted to be soft and without edema. He has no voice changes and is not in respiratory distress.
What is the most likely diagnosis?
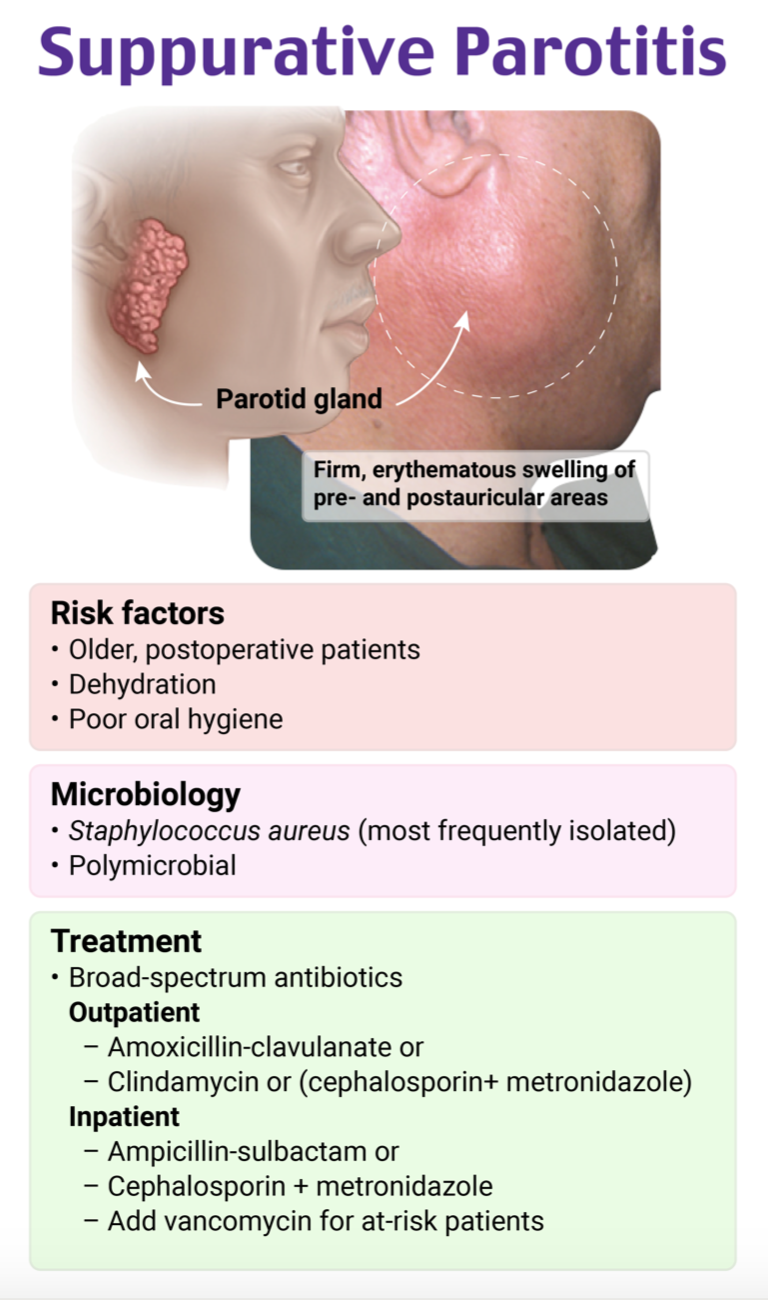
Answer: Suppurative Parotitis
Epidemiology
- Acute bacterial parotitis
- Uncommon diagnosis1
- Most likely to occur in the extremes of ages, elderly patients and neonates1
- More common in the elderly than neonates, especially those with systemic illness or recent surgical procedures2
- In post-op patients, occurs in 0.002% to 0.04%1
- Abdominal surgeries are the most common surgical procedures associated with suppurative parotitis; the reason for this is unclear
- Equal male to female ratio1
- Accounts for about 0.01% to 0.02% of hospital admissions1
- Causes
- Bacterial: Staph aureus is the most common bacterial cause. Other bacterial causes include anaerobic oral flora, Strep viridans, E. coli and other gram-negative organisms (in hospitalized patients), mycobacterium tuberculosis, GBS (in neonates)3
- Less common are viral etiologies: mumps, HIV, influenza, coxsackie A, CMV, echovirus, enterovirus, parainfluenza1
- Predisposing factors
- Elderly: dehydration, malnutrition, sialolithiasis, neoplasm, dental infection, immunosuppression, Sjögren’s syndrome, diabetes mellitus, medications that decrease salivation4
- Neonates: prematurity, dehydration, duct stasis3
Anatomy
- Parotid gland is a salivary gland1
- Consists of a superficial lobe and a deep lobe separated by the facial nerve
- Exocrine gland that secretes saliva1
- Controlled by parasympathetic nervous system
- Stensen’s duct is the excretory duct and passes through the masseter muscles, buccinator, and into the oral mucosa lateral to the secondary maxillary molar
- Saliva contains fibronectin which promotes adherence of staphylococcal species to mucous membranes2
- Parotid gland is the salivary gland most affected by infection4
- Larger size of Stensen’s duct compared to other salivary gland ducts allows easier spread of infection
- Has less bacteriostatic secretions compared to other salivary glands

Clinical Presentation
- Complaint of acute onset of pain, swelling, and/or tenderness of one or, less commonly, both parotid glands6
- Bilateral parotitis is typically caused by mumps or inflammatory conditions such as Sjögren’s syndrome1
- Pain is worse with chewing and can radiate to the nearby ear1
- On exam, the affected gland can appear swollen, warm, erythematous, or indurated6
-
- If gland is massaged, it often exhibits purulent drainage from the Stenson’s duct into the oral mucosa
- Can have visible or palpable stone in Stensen’s duct if sialolithiasis present1
- Fever or leukocytosis can be present6
Evaluation
- Clinical diagnosis
- Purulent drainage from Stensen’s duct is diagnostic6
- Labs
- Obtain CBC, chemistry panel, gram stain and culture of purulent drainage4
- Amylase can be elevated, but is nonspecific1
- Elevated ESR/ CRP supportive of diagnosis but are nonspecific7
- Imaging
- Rarely necessary for diagnosis1
- Ultrasound: can identify abscess, sialolithiasis, stenosis7
- CT can help detect lesions in or around the parotid gland, but only has a 75% sensitivity in distinguishing if the lesion is inflammatory or neoplastic in nature 4
- When CT is combined with clinical findings and labs, sensitivity can increase to 90%4
- MRI can be used to help differentiate parotitis from neoplasm if suspected, as well as identify local invasion of surround structures4
Treatment
- Hydration, antibiotics, symptom control8
- Symptom control
- Local heat, gentle massage, sialagogues, good oral hygiene8
- Sialagogues (sour candy and sour food) are helpful for those with sialolithiasis1
- Local heat, gentle massage, sialagogues, good oral hygiene8
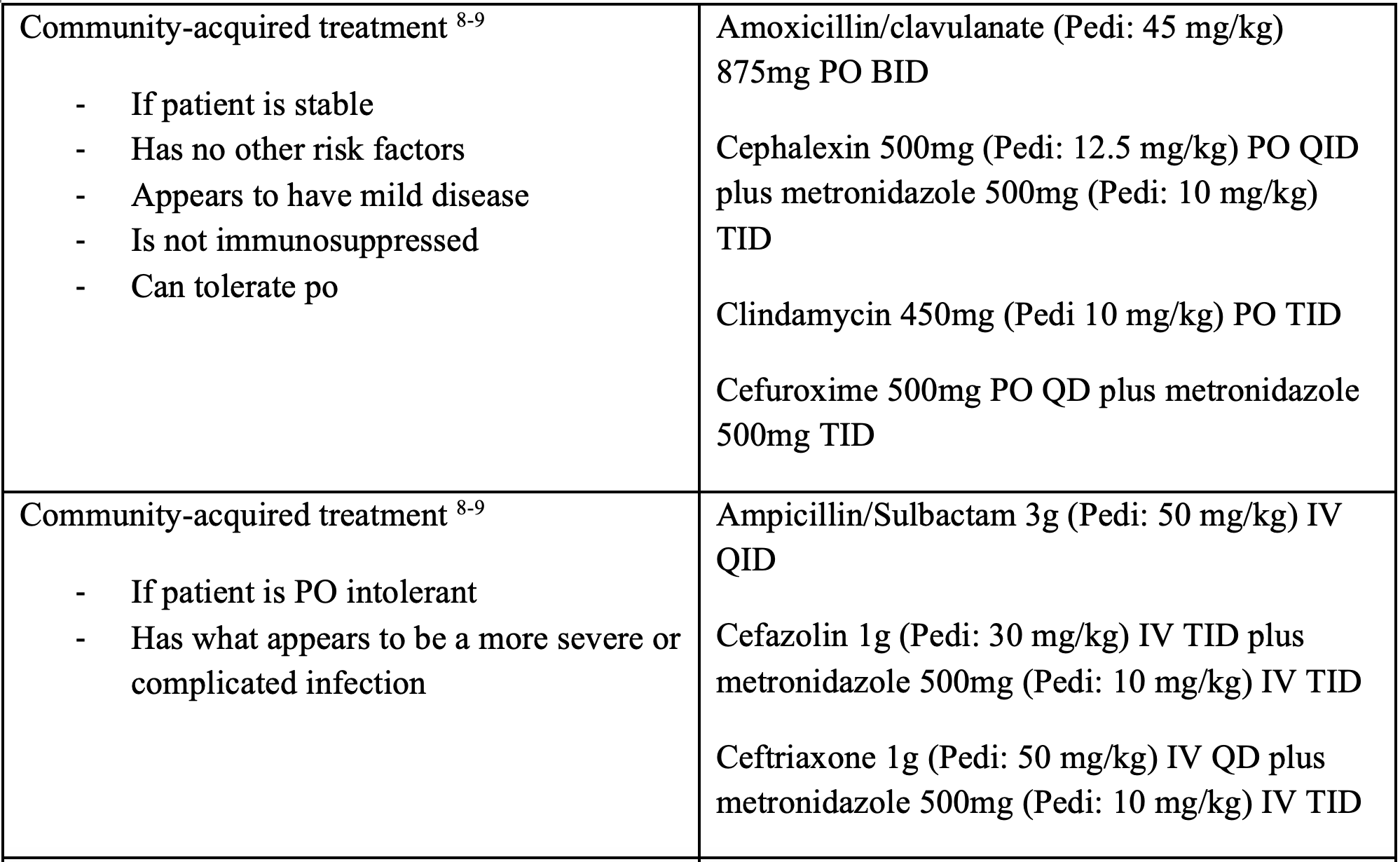
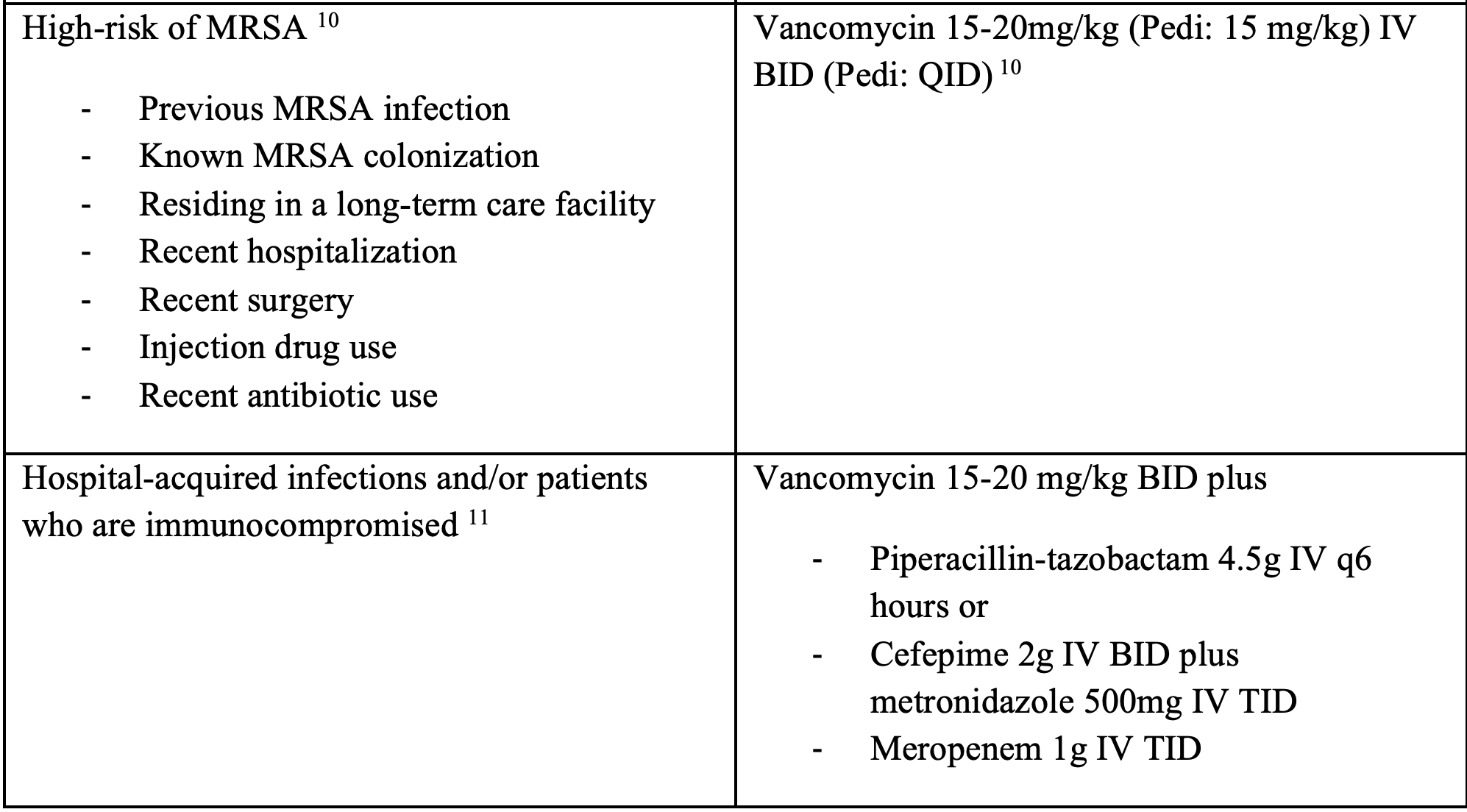
- Antibiotics
- 10-14 days of antibiotics recommended8
- Bacterial causes are far more common than viral so treat all cases of suppurative parotitis with antibiotics
- Specialist may tailor antibiotics to culture and sensitivities once resulted12
- 10-14 days of antibiotics recommended8

Consultation – ENT for surgical I&D if any of the following present:8
- Facial nerve involvement
- Spread of infection into adjacent structures (deep fascial spaces, pharyngeal space)
- Abscess formation
- No clinical improvement after 48-72 hours of antibiotics
Complications
- Include abscess, erysipelas, osteomyelitis, Lemierre syndrome, facial paralysis, airway obstruction, and sepsis1
Pearls:
- Suppurative parotitis is a clinical diagnosis
- ENT should be consulted urgently if patient presents to the ED with abscess, facial nerve involvement, or extension of infection into adjacent structures
- Staph aureus is the most common underlying cause, so consider treating for MRSA based on the patient’s risk factors
- Educate patients on good oral hygiene to help prevent further infection

A 56-year-old man presents to the emergency department with a chief concern of facial swelling that began this morning. He notes swelling of his left cheek to the preauricular area and the angle of the mandible. It is associated with fever and dysphagia. The exam is significant for a fever of 101°F (38.3°C), a warm and firm mass on the left cheek, and purulent discharge from the left buccal mucosa opposite the second upper molar. Which of the following is the best treatment for this patient?
A) Admission and intravenous nafcillin and clindamycin
B) Discharge with oral ciprofloxacin and clindamycin for 14 days
C) Intraoral incision and drainage and discharge with clindamycin
D) Treatment with oral sialogogue such as hard candy
Answer: A
This patient presents with a clinical course consistent with suppurative parotitis. This disease is a polymicrobial infection of the parotid gland. Staphylococcus aureus and oral flora are the most common causes. Typically, patients report the acute onset of unilateral facial pain with extreme tenderness to palpation, which can be associated with difficulty opening the mouth (trismus) or difficulty swallowing (dysphagia). Furthermore, purulent material typically can be expressed from Stensen duct opposite the second upper molar on the affected side. Diagnosis can be made clinically, but an elevated lipase in the absence of pancreatitis, advanced imaging, or Gram stain from the expressed pus can be used to confirm the diagnosis. Treatment requires admission and IV antibiotics (nafcillin plus either metronidazole or clindamycin is preferred for healthy adults). The location of the infection in the face requires close monitoring initially for the spread to deeper fascial planes. Patients who improve after 48 hours may be discharged on oral antibiotics for a 10–14 day course.
Discharging with oral antibiotics (B) is not recommended due to the risk of the spread of infection to deeper fascial spaces. These patients need close observation, and some may require surgical drainage for source control if IV antibiotics are not showing initial improvement. Intraoral incision and drainage (C) would be indicated for suppurative odontogenic infections such as a periapical abscess. However, the location of the drainage in this patient is Stensen duct, which confirms infection of the parotid, and intraoral incision is unlikely to relieve this. Additionally, periapical abscesses are typically on the mandibular or maxillary surface just proximal to the tooth, not on the buccal surface. Treatment with an oral sialogogue (D) is advised for sialolithiasis or stones within the salivary gland or ducts. These patients present with mild to moderate pain and swelling but are afebrile and do not have purulent discharge from the duct to suggest secondary infection behind the obstruction. Initial treatment is discontinuing medications that may reduce flow, oral hygiene, hydration, and hard or sour candies to promote flow.
Further FOAMed:
http://www.emdocs.net/parotitis-and-sialadenitis/
https://pemcincinnati.com/blog/briefs-parotitis/
References:
1. Wilson M, Pandey S. Parotitis. StatPearls [Internet]. 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560735/
2. Mohammed I, Hofstetter M. Acute bacterial parotitis due to methicillin-resistant Staphylococcus aureus. Southern medical journal. 2004;97(11):1139. doi:10.1097/01.SMJ.0000140830.66461.12
3. Hamid R, Shera HA, Khurshid S, Bhat AN, Baba AA, Akhter A. Suppurative parotitis and submandibular sialadenitis. J Clin Neonatol. 2014;3(1):39-40. doi:10.4103/2249-4847.128730
4. Lampropoulos P, Rizos S, Marinis A. Acute suppurative parotitis: a dreadful complication in elderly surgical patients. Surg Infect (Larchmt). 2012;13(4):266-269. doi:10.1089/sur.2011.015
5. CCCOnline. Chapter 55: Digestive structures and function. In: CCCOnline, eds. Anatomy & Physiology. Pressbooks. https://pressbooks.ccconline.org/bio106/
6. Raad II, Sabbagh MF, Caranasos GJ. Acute bacterial sialadenitis: a study of 29 cases and review. Rev Infect Dis. 1990;12(4):591-601. doi:10.1093/clinids/12.4.591
7. Schapher M, Goncalves M, Mantsopoulos K, Iro H, Koch M. Transoral Ultrasound in the Diagnosis of Obstructive Salivary Gland Pathologies. Ultrasound Med Biol. 2019;45(9):2338-2348. doi:10.1016/j.ultrasmedbio.2019.05.019
8. Fattahi TT, Lyu PE, Van Sickels JE. Management of acute suppurative parotitis. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial surgeons. 2002;60(4):446-448. doi:10.1053/joms.2002.31234
9. WikEM contributors. Suppurative Parotitis. WikEM, The Global Emergency Medicine Wiki. September 9, 2020. Available at: https://wikem.org/w/index.php?title=Suppurative_parotitis&action=history. Accessed March 27, 2023.
10. Levine BJ. EMRA Antibiotic Guide. Emergency Medicine Residents’ Association; 2022.
11. Chow AW, Suppurative Parotitis in Adults. UpToDate. https://www.uptodate.com/contents/suppurative-parotitis-in-adults. Accessed on April 11, 2023.
12. Brook I. Diagnosis and management of parotitis. Arch Otolaryngol Head Neck Surg. 1992;118(5):469-471. doi:10.1001/archotol.1992.01880050015002
13. Kolekar S, Chincholi TS, Kshirsagar A, Porwal N. Acute neonatal parotid abscess: A rare case report. Afr J Paediatr Surg. 2016;13(4):199-201. doi:10.4103/0189-6725.194675
14. Gupta A, Kingdom T, McKernan A. Neonatal Parotitis: A Case Report. Clin Pract Cases Emerg Med. 2021;5(2);218-221. Doi:10.5811/cpcem.2021.3.51501








