Authors: Paraskevi (Vivian) Papas, MD (@vivpapas, EM Resident Physician, Northwell Health- North Shore University Hospital/LIJMC; Michael Sperandeo, MD (Assistant Professor, Dept of Emergency Medicine, Long Island Jewish Medical Center, Associate Program Director EMSL Medical Simulation Fellowship, Zucker School of Medicine at Hofstra/Northwell) // Reviewed by: Sophia Görgens, MD (EM Physician, Yale University, CT); Cassandra Mackey, MD (Assistant Professor of Emergency Medicine, UMass Chan Medical School); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 54-year-old woman presents to the ED with a 3-day history of progressive right arm swelling, heaviness, and dull discomfort. She recently underwent chemotherapy via a peripherally inserted central catheter (PICC) placed two weeks ago on her right side for newly diagnosed breast cancer. She denies fever, chest pain, or shortness of breath. On exam, her right upper extremity is visibly swollen from the mid-bicep to the shoulder with mild erythema, increased warmth, and prominent, dilated superficial veins across the upper arm and chest wall. A tender, palpable cord is noted over the medial aspect of the upper arm. Radial and ulnar pulses are intact, and there are no signs of infection or fluctuance around the PICC site.
Vital signs include temperature 98.4°F, heart rate 82 bpm, blood pressure 118/74 mmHg, respiratory rate 16, and oxygen saturation 99% on room air.
Doppler Ultrasound of the Right Upper Extremity reveals the following:1

Question: What is the diagnosis?
Answer: Upper Extremity Deep Vein Thrombosis
Epidemiology:
- 4-10% of DVTs are estimated to be an Upper Extremity Deep Vein Thrombosis (UEDVT.).2
- The incidence of upper extremity DVTs is increasing, likely due to the more frequent use of central venous catheters (CVCs), PICC lines, and cardiac pacemakers, in addition to oral contraceptives use.3
- Upper Extremity DVTs are broken down into two subcategories, Primary and Secondary
- Primary Upper Extremity DVT (20% of Cases)
-
- Subcategorized into upper extremity DVTs caused by venous thoracic outlet syndrome, effort-induced thrombosis, or idiopathic causes.3-5
- Thoracic Outlet Syndrome (TOS) & UEDVT
- Paget-Schroetter Syndrome (PSS)
- Idiopathic UEDVT
- No clear precipitating factor (no exertion/anatomic abnormality identified).
- May involve subtle/unrecognized compression.
- Less common; often linked to hypercoagulable states or other risk factors.3,5
-
- Secondary Upper Extremity DVT (80% of Cases)
-
- The most common risk factors for secondary upper extremity DVT is the use of intravenous devices such as central lines, PICC lines, or pacemaker leads.
- Other common causes of secondary UEDVT include cancer associated thrombosis, surgery or trauma of the arm/shoulder, pregnancy, use of oral OCPs or ovarian hyperstimulation syndromes.3,5
- Because secondary upper extremity DVT is often linked to cancer and central venous catheters (CVCs), it typically occurs in older adults, with an average age of around 60—much older than in cases of primary UEDVT.
- Combined estrogen–progestin OCPs ↑ risk of VTE (including UEDVT, DVT, PE).5
- Estrogen → ↑ hepatic clotting factors + ↓ fibrinolysis → prothrombotic state
-
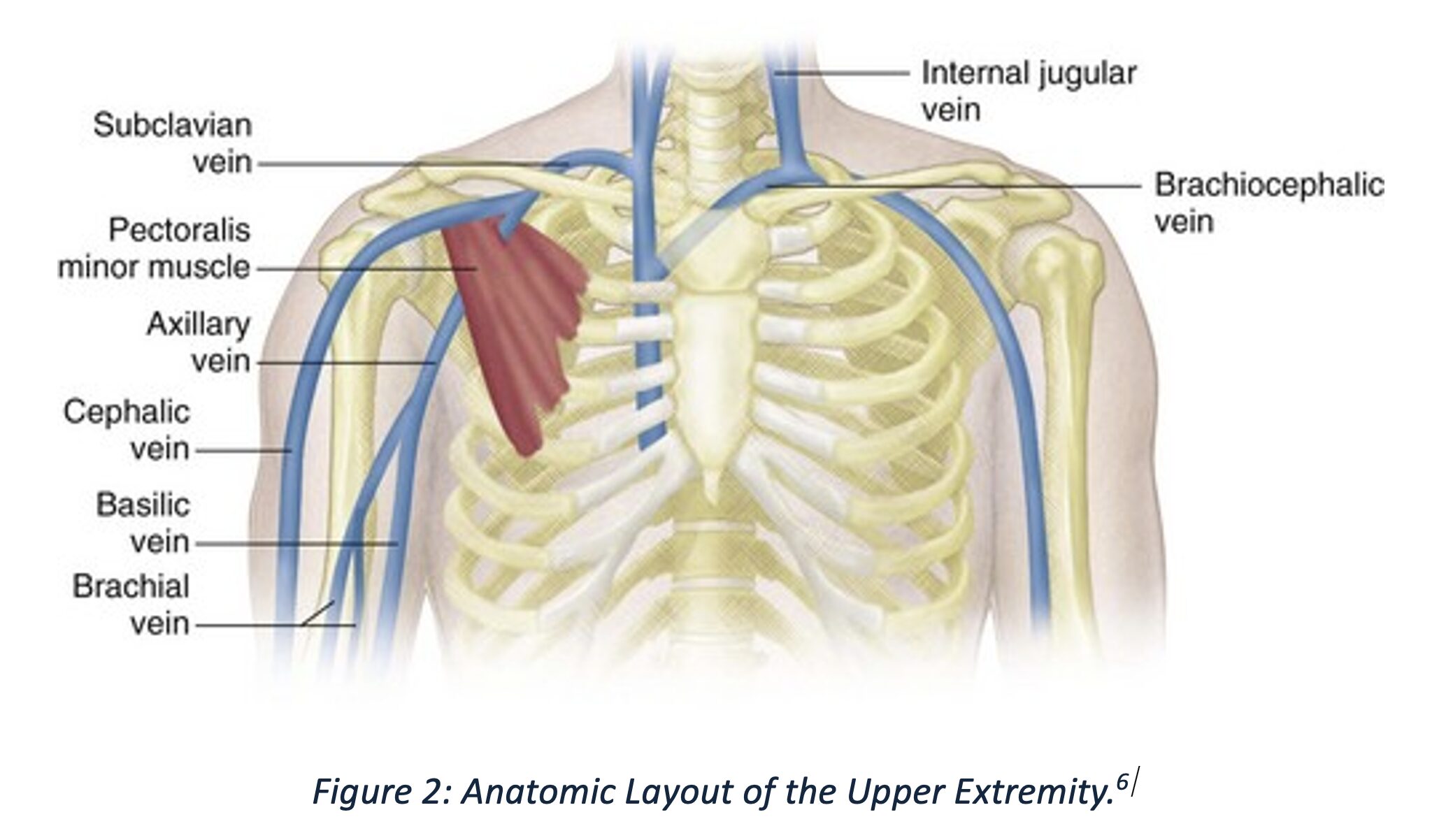
Anatomy:
- In Patients with UEDVT, the vessels most affected are the subclavian vein (62%), the axillary vein (45%), and the jugular vein (45%), with more than one thrombosis demonstrated in some cases.
- In primary UEDVT compression of the subclavian vein between the first rib and clavicle leads to endothelial injury and thrombosis.2
Clinical Presentation:
- Primary (effort-related) UEDVT, such as Paget-Schroetter syndrome, typically affects young, otherwise healthy individuals following vigorous or repetitive upper limb activity—commonly after weightlifting, sports, or manual labor.4
- Patients often report the sudden onset of swelling, heaviness, aching, or cramping in the dominant arm, sometimes following a known inciting event.
- On physical exam, there may be visible swelling of the upper extremity, dilated superficial veins across the shoulder or chest wall (Urschel’s sign), cyanosis or erythema of the limb, and tenderness along the course of the deep veins.
- Range of motion may be reduced due to pain or tightness.
- Vitals are often within normal limits, unless complicated by systemic symptoms.
- Secondary UEDVT is more common in older individuals with comorbidities and is frequently associated with indwelling devices such as central venous catheters, pacemaker leads, or malignancy.2,3,5
- These cases may present more insidiously, with gradual swelling, catheter dysfunction, or localized infection at the insertion site.
- Physical exam findings can include unilateral arm edema, erythema, tenderness, and in some cases, signs of infection such as warmth or purulence around a catheter site.
- Vital signs are typically stable unless infection or other complications are present.
- The anatomical location of the thrombus influences symptom severity:
- Thrombosis involving the subclavian or axillary veins is more likely to cause marked swelling and venous distension.
- Brachial vein thrombosis may present with more subtle findings.
Evaluation:
- The Constans Clinical Decision Score is a validated risk stratification tool to estimate the probability of upper extremity deep vein thrombosis (UEDVT).7
-
- Assigns one point each for the following criteria:
- Presence of venous material (such as a central venous catheter or pacemaker)
- Localized pain
- Unilateral pitting edema
- Assigns one point each for the following criteria:
-
- Subtracts one point if another diagnosis is at least as plausible as UEDVT.
- The total score ranges from -1 to 3.
- A score of ≤1 indicates low probability (“unlikely”), while a score of ≥2 indicates high probability of UEDVT (“likely”).7,8
- ARMOUR Study Findings8
- Prospective, multicenter trial evaluating Constan’s score + D-dimer + ultrasound.
- Low-risk patients (Constans ≤1 + negative D-dimer):
- Imaging safely avoided in 21% (87/406 patients).
- VTE rate during 3-month follow-up: 0.4% (1/249).
- Implication: In low-risk patients, UEDVT can be ruled out without imaging or anticoagulation.
- Limitations:
- Less effective in high-risk groups (patients with CVCs, hospitalized, or cancer).
- These groups still often require imaging due to higher pretest probability and limited D-dimer specificity.8
- Laboratory evaluation:
- D-dimer (to help rule out thrombosis if low risk)
- Complete blood count (CBC) (to check for infection or anemia)
- Coagulation studies (PT, aPTT) if anticoagulation or bleeding risk assessment needed.
- Consider tests for thrombophilia (e.g., antiphospholipid antibodies, factor V Leiden, prothrombin gene mutation) in select patients with primary UEDVT or recurring VTE, depending on scenario and help patient establish appropriate follow-up. Although these tests are not necessary as they are likely “send-out” labs and will not change ED disposition, this may be helpful for the inpatient team or outpatient physicians.
- Blood cultures if infection is suspected around catheter sites and there is evidence of sepsis.
Imaging:
- Ultrasonography is the preferred first-line test for diagnosing upper extremity DVT because it’s non-invasive, radiation-free, and offers real-time evaluation of vein structure and blood flow.
- It detects signs like vein non-compressibility, clot presence, vein enlargement, reduced blood flow, and collateral veins, which strongly indicate UEDVT when matched with clinical symptoms.
- Compression ultrasonography for UEDVT has a sensitivity of approximately 97% and specificity of approximately 94–96%.9
- Ultrasonography has limitations in detecting thrombi in central veins like the subclavian and brachiocephalic due to overlying bones, making compression and clear visualization difficult.
- In such cases, or when ultrasound results are inconclusive, CT venography, MR venography, or contrast venography are preferred.9,10
- Recent studies suggest MRV is highly accurate for UEDVT (sensitivity 93%, specificity 100%) and is useful for detection of VTE in central veins and distinguishing an acute versus chronic thrombus, but limited by cost, availability, and contraindications.
- These imaging methods offer better visualization of central veins, with contrast venography considered the gold standard despite being invasive and involving radiation and contrast risks.9,10
Treatment:
- Primary UEDVT (Paget–Schroetter / Effort Thrombosis)
- Anticoagulation => immediate (DOACs, LMWH, or warfarin if contraindications).
- CDT (Catheter Directed Thrombolysis) => consider if symptoms <14d, severe, low bleeding risk.
- Why: restores patency, reduces post-thrombotic syndrome.11,12
- Surgery (first rib resection ± scalenectomy) => usually required for definitive cure.
- Why: removes anatomic compression, prevents recurrence.
- Anticoagulation alone => if poor surgical candidate or delayed presentation (>2–3 weeks).11,12
- Treat for 3–6 months, but higher recurrence risk.
- Duration
- After surgery ± CDT => 3 months.11,12
- Without surgery => 3–6 months (lean toward 6 months for recurrence prevention).
- Consults
- Hematology/Thrombosis => Concerns/questions regarding anticoagulation or drug selection.
- Vascular Surgery => definitive decompression needs suspected.
- Interventional Radiology => CDT candidate/venography required.
- Secondary UEDVT (Catheter-Associated, Malignancy, Trauma, Surgery)
- Secondary UEDVT is treated with anticoagulation for at least 3 months (UFH if renal failure, LMWH if GI/GU cancer, DOACs if other cancers or non-cancer, warfarin if others contraindicated), with management of any catheter (salvage, removal, or continuation if functional).
- Anticoagulation Choices, Doses, and Rationale
- Unfractionated Heparin (UFH)
- When preferred: In patients with UEDVT diagnosis and renal failure/dialysis (hepatic clearance, reversible, short half-life).2
- 80 U/kg IV bolus (max 5,000 U) → 18 U/kg/hr infusion.
- Monitor aPTT 1.5–2.5× or anti-Xa 0.3–0.7.
- Dose reduction (e.g., enoxaparin 30 mg SC once daily) may be considered, though caution is still advised.
- Apixaban may be considered in select cases, as it has a lower bleeding risk than warfarin in severe renal failure, but data is limited, and caution is recommended.
- When preferred: In patients with UEDVT diagnosis and renal failure/dialysis (hepatic clearance, reversible, short half-life).2
- Low Molecular Weight Heparin (LMWH)
- When preferred: In patients with cancer (specifically GI/GU Cancers), or for those treated with catheter-directed thrombolysis (CDT) (for reversibility13-16
- Safer in GI/GU cancers (less mucosal bleeding than DOACs).
- The American Society of Hematology and the American Society of Clinical Oncology both recommend DOACs or LMWH over warfarin) for both initial and long-term treatment, due to improved efficacy and comparable safety profiles in cancer-associated thrombosis.17
- Enoxaparin: 1 mg/kg SC q12h (preferred) or 1.5 mg/kg q24h.
- If CrCl <30 → 1 mg/kg SC q24h.
- Dalteparin: 200 IU/kg SC q24h (max 18,000 IU) or 100 IU/kg q12h.
- DOACs
- Why preferred: In patients without cancer, or cancer outside of the GI/GU tract:13-16 Allows for convenient oral therapy, strong efficacy vs warfarin.
- Apixaban: 10 mg PO BID × 7d → 5 mg BID (2.5 mg BID for extended phase).
- Why preferred: most favorable bleeding profile, esp. in cancer.
- Rivaroxaban: 15 mg PO BID × 21d → 20 mg daily with food (10 mg daily for extended phase).
- Edoxaban: 60 mg daily after 5–10d parenteral anticoagulation(30 mg if renal impaired/low weight).
- Dabigatran: 150 mg BID after 5–10d parenteral anticoagulation (avoid if CrCl <30).
- Warfarin
- Start with parenteral anticoauation (UFH/LMWH) for ≥5d + INR ≥2 × 2 days.15-17
- INR goal: 2–3.
- Why used:
- Mechanical heart valves, APS.
- Cost/access limitations.
- When DOACs/LMWH contraindicated.
How long does a patient require anticoagulation?
- Provoked, non-cancer => ≥3 months.16,17
- Catheter remains => anticoagulation while catheter in place + 3 months after removal.
- Cancer-associated => ≥3–6 months; extended/indefinite while cancer is active.
- Recurrent or severe thrombophilia → indefinite.
Catheter Management
- If needed & functional => keep in place, anticoagulate.16,17
- If infected, nonfunctional, or unnecessary => remove (after anticoagulation if feasible).
Catheter Occlusion (Salvage)
- Alteplase 2 mg/2 mL instilled into lumen, dwell 30–120 min, aspirate/flush.16,17
- May repeat once (80–90% success).
- Rationale: preserves vascular access in oncology/dialysis patients.


Disposition:
- Discharge:
- Most patients with an upper extremity DVT can be safely discharged if:
- Hemodynamically stable
- No contraindications to anticoagulation
- Reliable follow-up with PCP or specialist available
- Typical outpatient therapy:
- DOACs (apixaban, rivaroxaban)
- LMWH bridge to warfarin if DOAC not used
- Most patients with an upper extremity DVT can be safely discharged if:
- Admit:
- Extensive clot burden
- High bleeding risk requiring close monitoring
- Significant comorbidities complicating management
- Suspected pulmonary embolism
- Suspected underlying malignancy needing workup
- Primary UEDVT cases if patient is a candidate for catheter-directed thrombolysis.
Pearls:
- Suspecting UEDVT
- Unilateral arm swelling, pain, erythema, dilated superficial veins
- Risk factors: central venous catheters, malignancy, vigorous activity
- Diagnosis
- Constans Score: limited utility
- D-dimer: helpful if low probability; less reliable in cancer/hospitalized
- Duplex US: first-line, high sensitivity/specificity
- CT/MR venography: if US non-diagnostic or central veins suspected
- Serial US: if initial study negative but suspicion persists
- Catheter Management: do not remove if functional and required => anticoagulate
- For both Primary and Secondary UEDVT Treatment
- DOACs: preferred for most
- LMWH: preferred in cancer (specifically GU/GI cancers), and if patient is a candidate for intervention. Typically associated with high out-of-pocket cost-burden
- Warfarin: alternative (inexpensive), requires bridging + INR monitoring
- Duration: ≥3 months
- Primary/Paget–Schroetter Syndrome (Effort Thrombosis)
- Start anticoagulation + early IR/vascular consult
- IR: thrombolysis if <14 days and symptomatic
- Vascular surgery: first rib resection for definitive decompression
- Multidisciplinary approach => best patency, symptom relief, return to activity
- Start anticoagulation + early IR/vascular consult

A 52-year-old man presents to the ED with swelling, erythema, and a feeling of heaviness in his right arm for the past 2 days, and the physical examination reveals nonpitting edema of the upper extremity without overlying cellulitis. Which of the following is most likely to be found in this patient if the diagnosis is upper extremity deep vein thrombosis?
A) Central venous catheter placement
B) History of smoking
C) Hypertension
D) Obesity
E) Recent international travel
Correct answer: A
Upper extremity deep vein thrombosis (DVT) represents approximately 10% of all cases of DVT and is increasingly recognized in emergency medicine practice, especially with the growing use of central venous catheters and implanted devices. Upper extremity DVT may be classified as primary (spontaneous, including effort-related thrombosis such as Paget-Schroetter syndrome) or secondary (most commonly catheter-associated). Among secondary causes, central venous catheter placement is the most significant risk factor, contributing to mechanical endothelial trauma and local venous stasis that facilitate thrombus formation.
In the emergency setting, patients with upper extremity DVT often present with arm swelling, pain, erythema, and heaviness. Physical examination may reveal nonpitting edema, dilated superficial veins, or even signs of venous congestion. Duplex ultrasonography is the initial diagnostic modality of choice and has high sensitivity and specificity for detecting thrombus in the subclavian, axillary, and brachial veins. Management typically mirrors that of lower extremity DVT and includes anticoagulation with direct oral anticoagulants or low-molecular-weight heparin, though thrombolysis or catheter removal may be indicated in select cases.
Preventive strategies for upper extremity DVT focus on minimizing catheter use when possible, using the smallest catheter size necessary, avoiding catheter placement in the subclavian vein when feasible, and removing catheters promptly when no longer needed.

Although smoking (B) is a general prothrombotic risk factor, its role is more prominent in arterial disease and lower extremity venous thrombosis. In the setting of upper extremity DVT, smoking does not have a strong independent association compared to mechanical and iatrogenic contributors such as central venous catheter use.
Hypertension (C) is a well-established risk factor for cardiovascular and cerebrovascular disease but has limited association with venous thrombosis. Its contribution to venous clot formation is minimal, particularly in comparison to localized endothelial trauma and stasis caused by central venous catheterization.
Obesity (D) is associated with an increased risk of venous thromboembolism, particularly in the lower extremities. While it may contribute to overall thrombotic risk, it is not among the leading independent risk factors for upper extremity DVT.
Prolonged immobility from travel (E) is a recognized risk factor for lower extremity DVT due to venous stasis in the legs. However, it does not confer a similarly high risk for upper extremity DVT. This patient’s symptoms are unilateral and localized to the upper extremity, where venous stasis from travel-related immobility would not be expected to play a major role.
References
- Radiopaedia.org. “Upper limb DVT (PICC line associated thrombus).” Accessed August 28, 2023. https://radiopaedia.org/cases/upper-limb-dvt-picc-line-associated-thrombus?lang=us
- Heil J, Miesbach W, Vogl T, Bechstein WO, Reinisch A. Deep Vein Thrombosis of the Upper Extremity. Dtsch Arztebl Int. 2017 Apr 7;114(14):244-249. doi: 10.3238/arztebl.2017.0244. PMID: 28446351; PMCID: PMC5415909.
- Grigorian A, Nahmias JT. Upper Extremity Deep Venous Thrombosis. [Updated 2023 Jan 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482420/
- Alahmadi MH, Baril DT. Paget-Schroetter Syndrome. [Updated 2025 Jul 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482416/
- Hoexum F, Jongkind V, Coveliers HME, Wisselink W, Yeung KK. Long-Term Outcomes of Nonoperative and Surgical Management of Paget-Schroetter Syndrome. Journal of Endovascular Therapy. 2022;31(2):171-177. doi:10.1177/15266028221120360
- Kirsch, J. D., Hamper, U., & Scoutt, L. M. (2015, December 26). Venous sonography of the upper extremities and thoracic outlet. Radiology Key. Retrieved from https://radiologykey.com/venous-sonography-of-the-upper-extremities-and-thoracic-outlet
- Constans J, Salmi LR, Sevestre-Pietri MA, Perusat S, Nguon M, Degeilh M, Labarere J, Gattolliat O, Boulon C, Laroche JP, Le Roux P, Pichot O, Quéré I, Conri C, Bosson JL. A clinical prediction score for upper extremity deep venous thrombosis. Thromb Haemost. 2008 Jan;99(1):202-7. doi: 10.1160/TH07-08-0485. PMID: 18217155.
- Van Es N, Bleker SM, Di Nisio M, Kleinjan A, Beyer-Westendorf J, Camporese G, Kamphuisen PW, Büller HR, Bossuyt PM; ARMOUR study investigators. A clinical decision rule and D-dimer testing to rule out upper extremity deep vein thrombosis in high-risk patients. Thromb Res. 2016 Dec;148:59-62. doi: 10.1016/j.thromres.2016.10.019. Epub 2016 Oct 24. PMID: 27815967.
- Di Nisio M, Van Sluis GL, Bossuyt PM, Büller HR, Porreca E, Rutjes AW. Accuracy of diagnostic tests for clinically suspected upper extremity deep vein thrombosis: a systematic review. J Thromb Haemost. 2010 Apr;8(4):684-92. doi: 10.1111/j.1538-7836.2010.03771.x. Epub 2010 Feb 6. PMID: 20141579.
- van Dam LF, Dronkers CEA, Gautam G, Eckerbom Å, Ghanima W, Gleditsch J, van Haren GR, von Heijne A, Huisman MV, Stöger JL, Westerlund E, Kroft LJM, Klok FA. Detection of upper extremity deep vein thrombosis by magnetic resonance non-contrast thrombus imaging. J Thromb Haemost. 2021 Aug;19(8):1973-1980. doi: 10.1111/jth.15394. Epub 2021 Jun 16. PMID: 34018662; PMCID: PMC8361740.
- Espitia, Olivier, et al. “A systematic review and meta-analysis of the incidence of post-thrombotic syndromeerecurrent thromboembolism, and bleeding after upper extremity vein thrombosis.” Journal of Vascular Surgery: Venous and Lymphatic Disorders 12.1 (2024): 101688.
- Illig KA, Gober L. Optimal management of upper extremity deep vein thrombosis: Is venous thoracic outlet syndrome underrecognized? J Vasc Surg Venous Lymphat Disord. 2022 Mar;10(2):514-526. Epub 2021 Aug 2. PMID: 34352421.
- Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e419S-e496S. doi: 10.1378/chest.11-2301. Erratum in: Chest. 2012 Dec;142(6):1698-1704. PMID: 22315268; PMCID: PMC3278049.
- Montiel, F. S., Ghazvinian, R., Gottsäter, A., & Elf, J. (2017). Treatment with direct oral anticoagulants in patients with upper extremity deep vein thrombosis. Thrombosis Journal, 15(1), 26.
- Engelberger, R. P., & Kucher, N. (2012). Management of deep vein thrombosis of the upper extremity. Circulation, 126(6), 768-773.
- Valeriani E, Di Nisio M, Porceddu E, Agostini F, Pola R, Spoto S, Donadini MP, Ageno W, Porfidia A. Anticoagulant treatment for upper extremity deep vein thrombosis: A systematic review and meta-analysis. J Thromb Haemost. 2022 Mar;20(3):661-670. doi: 10.1111/jth.15614. Epub 2021 Dec 23. PMID: 34846783.
- Lyman GH, Carrier M, Ay C, Di Nisio M, Hicks LK, Khorana AA, Leavitt AD, Lee AYY, Macbeth F, Morgan RL, Noble S, Sexton EA, Stenehjem D, Wiercioch W, Kahale LA, Alonso-Coello P. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv. 2021 Feb 23;5(4):927-974. doi: 10.1182/bloodadvances.2020003442. Erratum in: Blood Adv. 2021 Apr 13;5(7):1953.






