Author: Christian Capanna, MD (EM Resident Physician, Advocate Christ Emergency Medicine Program) // Reviewed by: Edward Lew, MD (@elewMD); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Case
A 30-year-old woman with past medical history of type 2 diabetes presents to the emergency department with 3 days of vague abdominal/back pain, with associated subjective fever, chills, nausea and vomiting. She states she was recently seen and evaluated at an outside hospital, where she was diagnosed with a urinary tract infection and discharged home on oral antibiotics, which she has been taking for 3 days, but does not feel any better.
Vital signs include T 38.5°C, HR 110, BP 105/64, RR 21, SpO2 100% on room air
On examination, the patient appears ill. She appears dehydrated, lungs are clear to auscultation bilaterally, cardiac exam is reveals tachycardia and the patient has no tenderness in her abdomen. GU exam is grossly unremarkable, however, the patient has right sided costovertebral tenderness. She states she’s had a history of urine infections in the past, but this feels different.
Introduction
Renal abscesses are infections contained to an encapsulated region within the renal parenchyma and are often divided into cortical or corticomedullary by location (1). Perinephric abscesses on the other hand, are similar collections of infection located between Gerota’s fascia and the renal capsule (2). These infections often arise as either complications of urinary tract infections or hematogenous seeding from primary infected sites (2,3). Both disease processes represent advanced infectious processes that can be potentially lethal and represent a poor prognosis, especially in individuals more prone to infection such as the immunosuppressed. Moreover, renal abscesses are often silent clinically (2, 3, 4), and have mortality rates ranging from 1-14% (3, 5, 6). Thus, these diagnoses can be extremely challenging for providers. It is reported that only 35-38% of patients with perinephric abscesses are correctly diagnosed at the time of admission, making it a crucial disease process to review for emergency physicians (5, 6).
Differential Diagnosis
The differential diagnosis of Renal and Perirenal abscesses can include (7):
- Lobar Pneumonia
- Acute Pyelonephritis with or without papillary necrosis
- Emphysematous pyelonephritis
- Malakoplakia
- Renal Cell Carcinoma
- Hydronephrosis
- Nephrolithiasis with or without infection
Presentation
Renal and perinephric abscesses typically present with insidious symptoms including fever, vague abdominal pain, fatigue, sweats/chills, and at times, weight loss (7). Interestingly, symptoms typically thought to be present in a urinary tract infection, including dysuria, urgency etc., are often not reported in many of these patients, making it an extremely difficult disease process for emergency physicians. In various case series, the most common symptoms in these patients included lumbar pain (76.5%) and fever (53%), followed by chills (28%) and anorexia and vomiting (25%). Moreover, the most common physical exam finding was found to be costovertebral tenderness (88%) which while present in other disease processes, such as pyelonephritis, should raise the emergency physician’s awareness of a possible abscess and possible need for further imaging such as ultrasound or CT (8).
The following are known risk factors for renal and perinephric abscesses
- Diabetes mellitus, being present in up to 1/3 of cases
- Urinary tract abnormalities including nephrolithiasis, vesicoureteral reflux, neurogenic bladder, obstructive tumors etc. which were also present in up to 1/3 of cases
Diagnostics
Laboratory findings in renal/perinephric abscesses tend to be non-specific. Infectious findings such as leukocytosis, lactic acidosis, or elevated inflammatory markers such as ESR and CRP, can help point the clinician in the right direction, but are not specific or sensitive. Additionally, even urine analysis and culture findings are not always present, as this will depend on whether the abscess communicates with the collecting system, which is not always the case, particularly in infected cysts or hematogenous spread (10). For those individuals who develop an abscess from a hematogenous source, blood cultures can be helpful for determining the causative organism and thus should be obtained prior to starting antibiotics when possible.
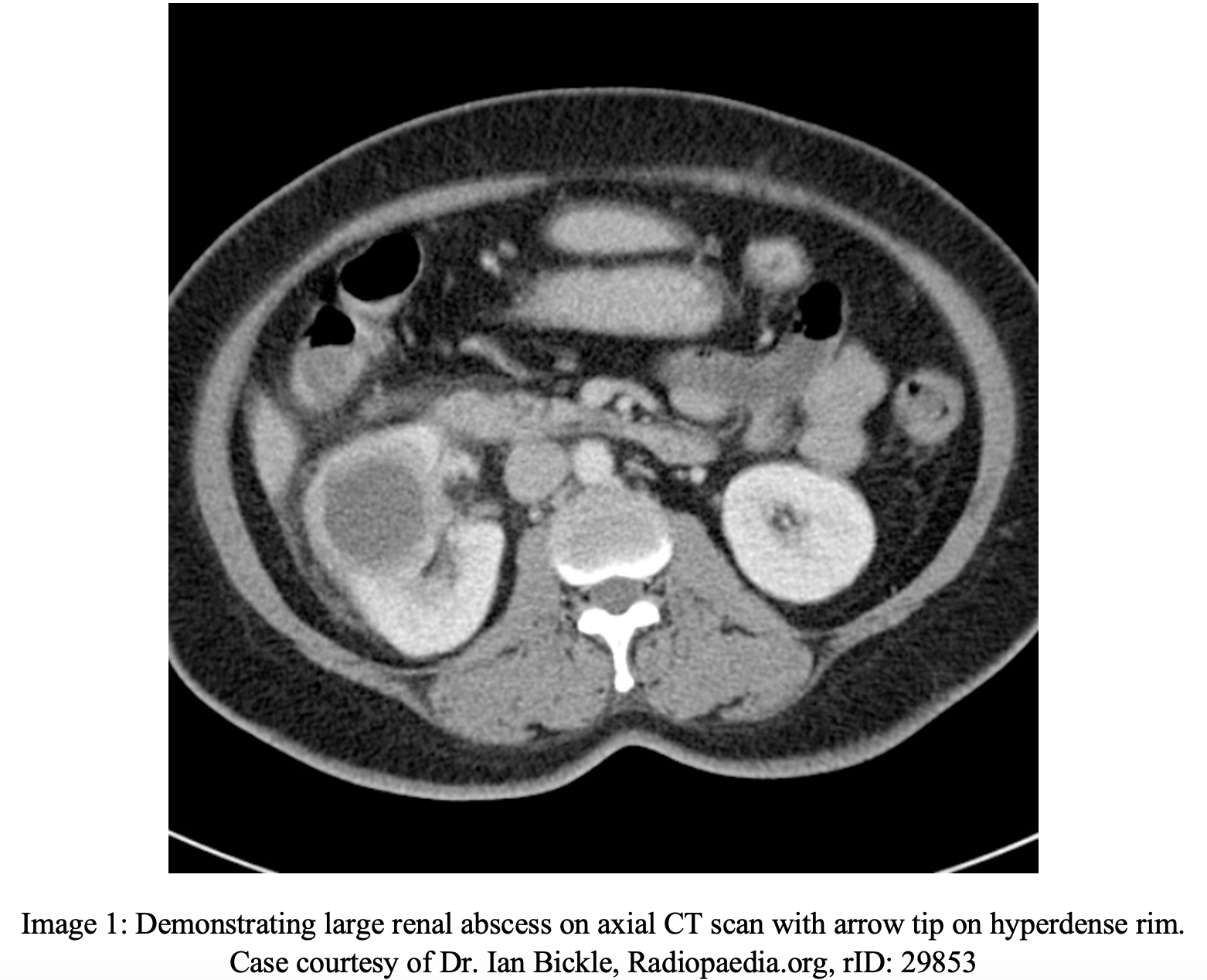
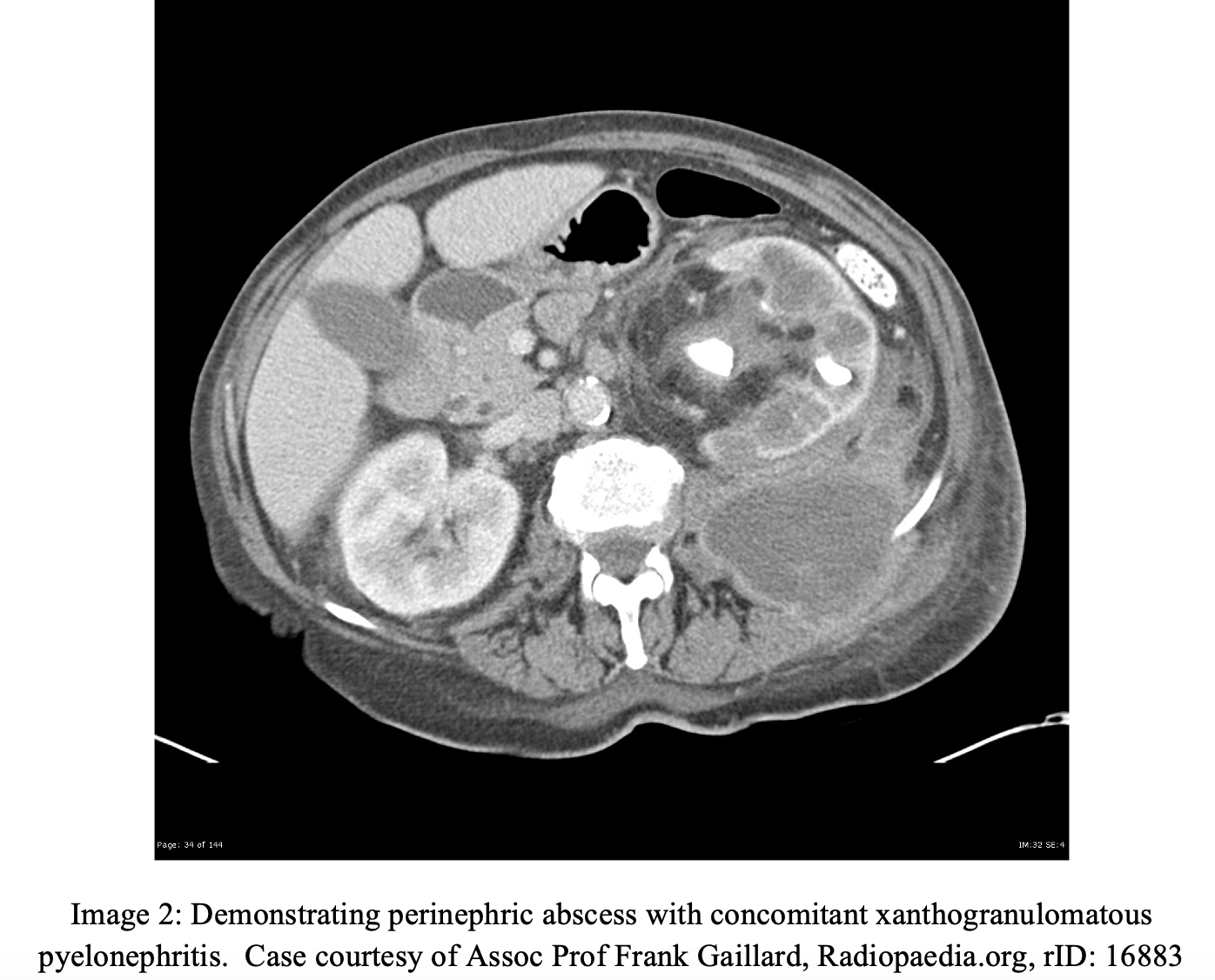
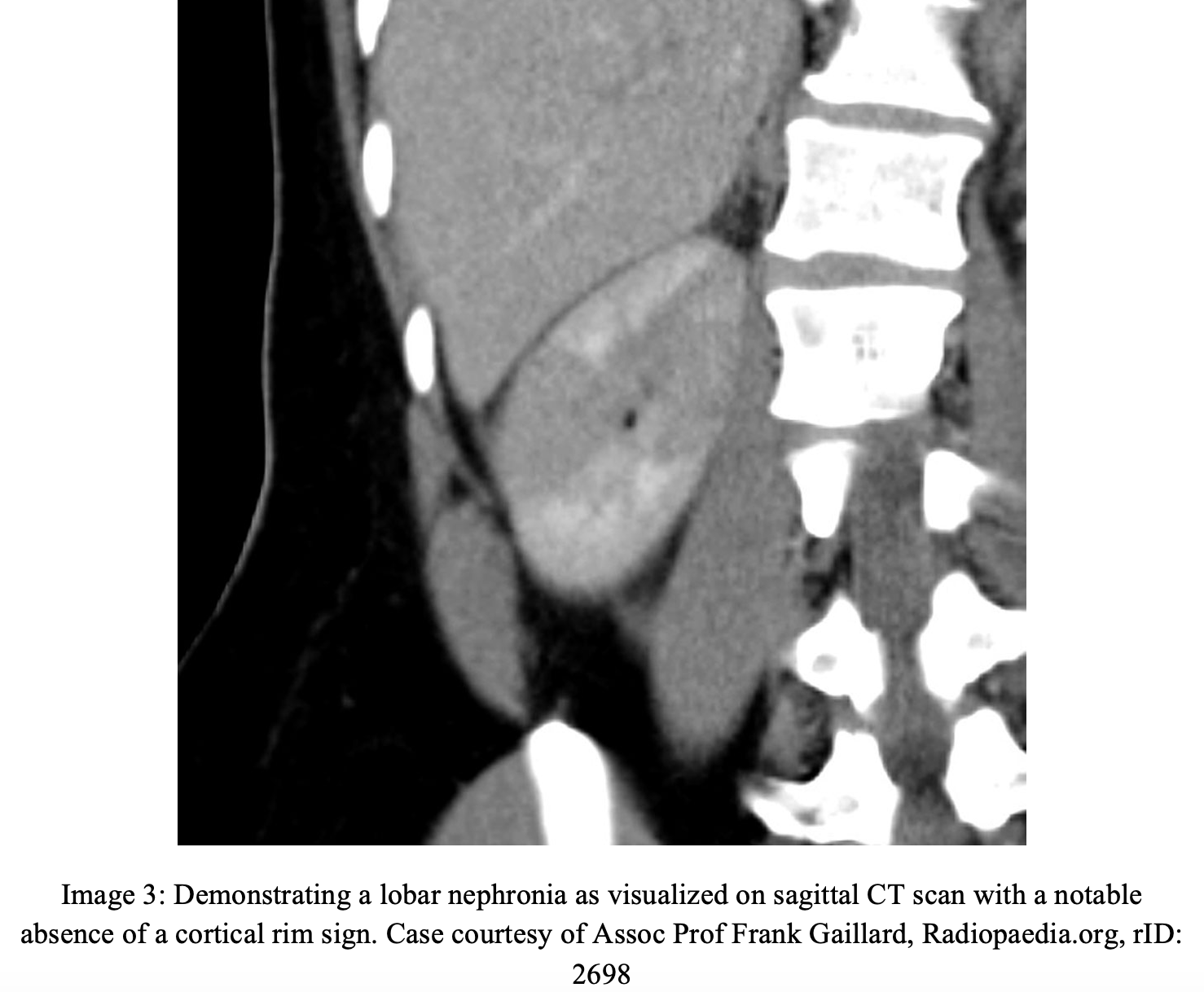
CT scan with contrast of the abdomen and pelvis is the single best diagnostic tool for the identification of renal and/or perinephric abscesses (11). On CT, renal abscesses appear as intrarenal walled-off cavities (image 1). A hyperdense rim is often visualized with IV contrast. CT may also demonstrate thickening of Gerota’s fascia, renal enlargement, decreased renal attenuation, inflammation of the parenchyma, or lobar necrosis. Focal or perirenal fluid and/or gas may also be seen (11, 12, 13). Perinephric abscesses are usually confined to the perinephric space by Gerota’s fascia, but at times have also been found to spread to other retroperitoneal structures and/or rupture into the collecting system (image 2) (13, 14). One such of these structures is the psoas musculature, creating a rarer clinical presentation of groin pain. Less commonly, there may be extension into the peritoneal cavity or take the form of a subphrenic abscess (14). In less serious, or developing, infections, a precursor structure known as a lobar nephronia can be visualized (image 3), which is often a single round or wedge shaped poorly definite lobe of the CT. This should raise the clinician’s concern for precursor to a full abscess, but a nephronia is not typically amenable to drainage (15).
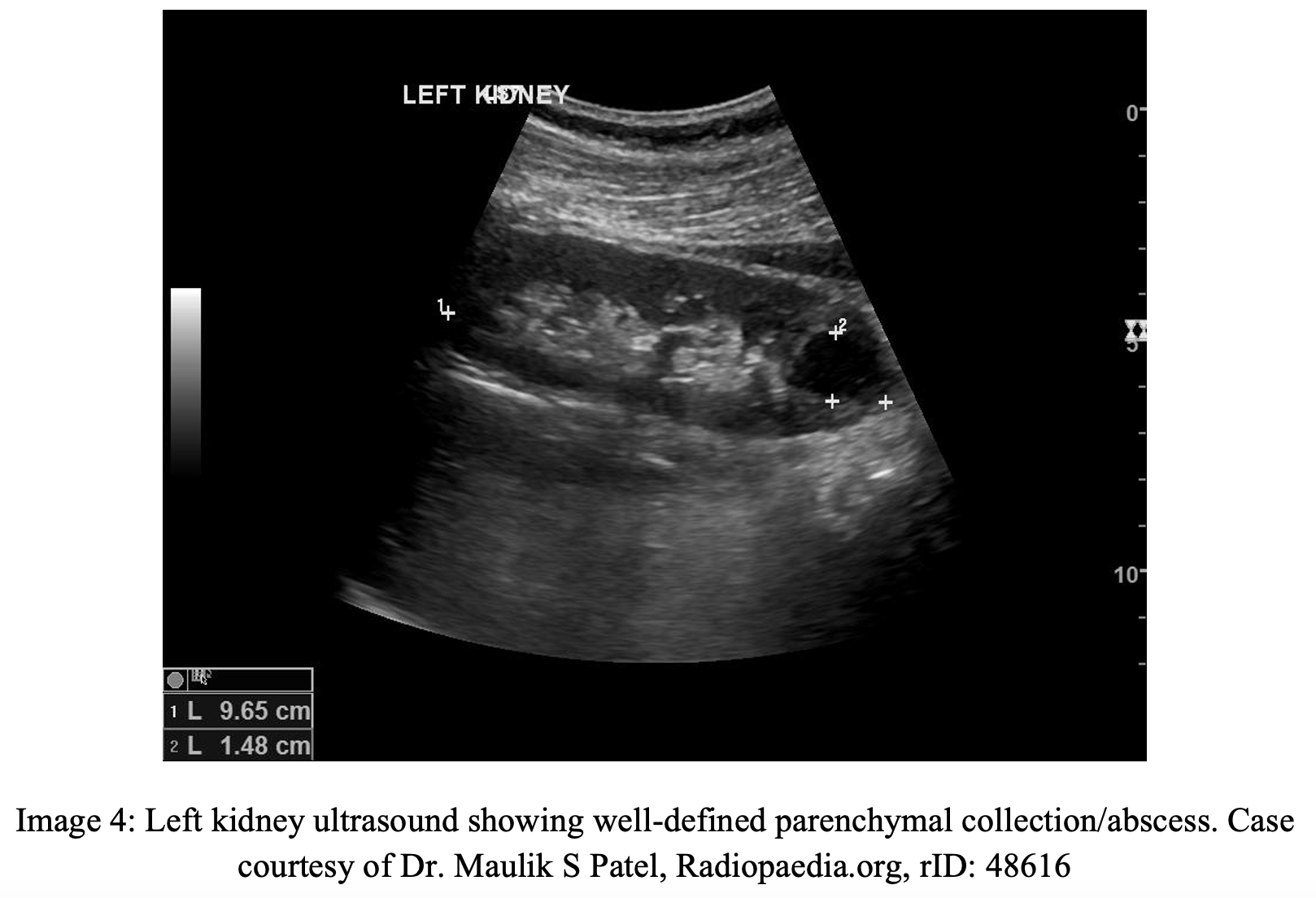
Ultrasound may also be used to visualize the abscess, which can demonstrate thick-walled cavities filled with fluid (image 4), making point of care ultrasound a modality that may detect this early, especially since this disease processes is so often missed upon its initial presentation (13).
Management
Similar to most other abscesses, the treatment of renal and perinephric abscesses focuses on the administration of antibiotics and when possible, drainage. Patients should also be given fluids, and have their fever and other symptoms, such as pain, treated as needed for patient comfort.
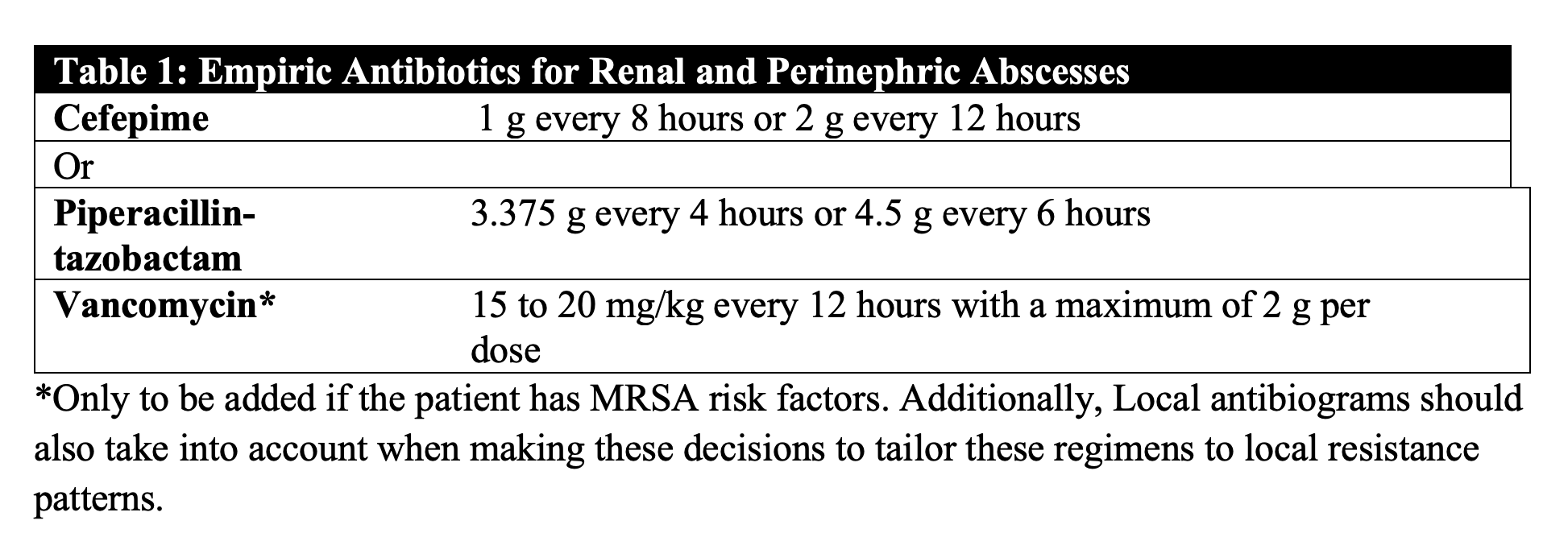
Antibiotics: Empirically, antibiotic therapy should take into account the pathogenesis of the abscess. Those associated with an infection of the collecting duct, such as pyelonephritis, should target gram negative Enterobacteriaceae which account for the large majority of infections (8) (Table 1).
Drainage: Not all renal and perinephric abscesses will require percutaneous or surgical drainage, however these decisions should be made with the help of a urology consultation. For renal abscesses, the size of the abscess is the determining factor, as those <5cm in diameter can be treated with medical therapy alone initially (16). For abscess >5cm percutaneous drainage and antibiotics is preferred given less morbidity and mortality vs. open surgical drainage (17). Placement of the drain is typically radiographically assisted and often drains are left in until drainage is minimal, typically up to 7 days. Surgical drainage or rescue nephrectomy may be required if patients fail medical treatments, or if an abscess occurs in the context of an anatomic abnormality, such as obstruction, or vesicoureteral reflux (9).
Disposition
All patients with presumed or confirmed renal or perinephric abscess should be admitted to the hospital for IV antibiotics and close monitoring with urologic consultation. Hospital length of stays have been shown to range anywhere between 5 to 31 days depending on the severity of infection, with one study showing the average hospital stay being 15 days (16).
Case Conclusion
Given that the patient had fever, tachycardia ,and persistent CVA tenderness on exam, a bedside ultrasound was obtained that showed a well-defined collection suspicious for abscess. A CT abdomen/pelvis demonstrated a renal abscess measuring approximately 6cm in diameter. Laboratory work up showed an elevated WBC to 16, with left shift. UA was negative for any signs of infection, but urine culture and blood cultures were obtained. Urology was consulted who recommended percutaneous drainage; the patient was started on IV antibiotics, fluids, given pain medication, and admitted to the hospital.
Take Home Points
- Renal and perinephric abscesses are serious, often missed diagnoses in the emergency department that are important for emergency clinicians to keep on their differential, as only 35% of renal and perinephric abscesses are correctly diagnosed in the emergency department.
- UA is not necessarily consistent with these infections unless the abscess involves the collecting system.
- Mortality of renal and perinephric abscesses can be as high as 14%.
- CT scan is the single best way to diagnosis these disease processes, but bedside ultrasound can offer a quicker diagnosis in some.
- Broad-spectrum antibiotics are the mainstay of treatment for all confirmed diagnoses and the size of the abscess (>5cm) will determine need for drainage.
- All patients with confirmed diagnosis should be admitted for continued antibiotics, culture results and urology consultation.
References
- Jaik NP, Sajuitha K, Mathew M, et al. Renal abscess. J Assoc Physicians India. 2006;54:241-243.
- Gardiner RA, Gwynne RA, Roberts SA. Perinephric abscess. BJU Int. 2011;107 Suppl 3:20-23. doi:10.1111/j.1464-410X.2011.10050.x
- Coelho RF, Schneider-Monteiro ED, Mesquita JL, Mazzucchi E, Marmo Lucon A, Srougi M. Renal and perinephric abscesses: analysis of 65 consecutive cases. World J Surg. 2007;31(2):431-436. doi:10.1007/s00268-006-0162-x
- Lin HS, Ye JJ, Huang TY, Huang PY, Wu TS, Lee MH. Characteristics and factors influencing treatment outcome of renal and perinephric abscess–a 5-year experience at a tertiary teaching hospital in Taiwan. J Microbiol Immunol Infect. 2008;41(4):342-350.
- Ko MC, Liu CC, Liu CK, et al. Incidence of renal and perinephric abscess in diabetic patients: a population-based national study. Epidemiol Infect. 2011;139(2):229-235. doi:10.1017/S095026881000107X
- Fullá J, Storme O, Fica A, et al. Abscesos renales y peri-renales: análisis de 44 casos [Renal and perinephric abscesses: a series of 44 cases]. Rev Chilena Infectol. 2009;26(5):445-451.
- Meyrier, AL. Renal and perinephric abscess. In: Post T, ed. UpToDate. Waltham, MA.: UpToDate; 2020. www.uptodate.com. Accessed July 10, 2020.
- Liu XQ, Wang CC, Liu YB, Liu K. Renal and perinephric abscesses in West China Hospital: 10-year retrospective-descriptive study. World J Nephrol. 2016;5(1):108-114. doi:10.5527/wjn.v5.i1.108
- Fowler JE Jr, Perkins T. Presentation, diagnosis and treatment of renal abscesses: 1972-1988. J Urol. 1994;151(4):847-851. doi:10.1016/s0022-5347(17)35103-0
- Hill GS. Renal infection. In: Uropathology, 1st Ed, Hill GS (Ed), Churchill Livingstone, New York 1989; 33.
- Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14(1):13-22. doi:10.1007/s10140-007-0591-3
- Huang JJ, Sung JM, Chen KW, Ruaan MK, Shu GH, Chuang YC. Acute bacterial nephritis: a clinicoradiologic correlation based on computed tomography. Am J Med. 1992;93(3):289-298. doi:10.1016/0002-9343(92)90235-4
- Gerzof SG, Gale ME. Computed tomography and ultrasonography for diagnosis and treatment of renal and retroperitoneal abscesses. Urol Clin North Am. 1982;9(1):185-193.
- Reese JH, Anderson RU, Friedland G. Splenic abscess arising by direct extension from a perinephric abscess. Urol Radiol. 1990;12(2):91-93. doi:10.1007/BF02923976
- Rosenfield AT, Glickman MG, Taylor KJ, et al. Acute focal bacterial nephritis (acute lobar nephronia). Radiology 1979; 132:553.
- Lee SH, Jung HJ, Mah SY, Chung BH. Renal abscesses measuring 5 cm or less: outcome of medical treatment without therapeutic drainage. Yonsei Med J. 2010;51(4):569-573. doi:10.3349/ymj.2010.51.4.569
- Siegel JF, Smith A, Moldwin R. Minimally invasive treatment of renal abscess. J Urol. 1996;155(1):52-55.








