Authors: Ryan Lynch, MD ( Emergency Medicine Resident, Jackson Memorial Hospital) and Mark Supino, MD (Attending Physician, Department of Emergency Medicine, Jackson Memorial Hospital) // Edited by: Edward Lew, MD (@elewMD); Alex Koyfman, MD (@EMHighAK); and Brit Long, MD (@long_brit)
Case:
A right hand dominant 15-year-old boy presented with his father for left elbow pain and swelling after injuring himself while playing basketball. Just prior to arrival, he had jumped up and fallen directly onto the lateral surface of his left elbow. Upon initial evaluation, he had appreciable swelling and bruising involving the left elbow joint and tenderness to palpation at the lateral surface of the elbow. Additionally, he had limited range of motion (ROM) at the elbow with both elbow flexion and extension as well as with forearm supination and pronation. Neurovascular exam was intact. Radiographs revealed an intra-articular radial head fracture (Figures 1 and 2). Upon re-evaluation, the patient was still experiencing difficulty with elbow movement despite ibuprofen and ice application. Orthopedic surgery was consulted because of concern for mechanical block in the setting of an intra-articular radial head fracture.
Once the orthopedic consultant was at bedside, we aspirated a small volume of blood from the elbow joint and subsequently injected approximately 5 mL of 1% lidocaine. Following the injection of the local anesthetic, the patient was able to perform active ROM at the elbow so a mechanical block was ruled out. He was placed in a sling, encouraged to mobilize the joint early, and discharged with orthopedic follow up in 4 weeks.
Figure 1: Lateral view x-ray of the left elbow showing an intra-articular radial head fracture with anterior fat pad (black arrow) and posterior fat pad (white arrow). (1)

Why is this case important to the emergency physician?
Though many of us encounter a large volume of pediatric patients during residency, that may drastically taper off as we transition to the community. As such, it is also essential to become familiar with special circumstances of orthopedic injuries as they pertain to the pediatric population.
Elbow fractures are of particular importance because they remain one of the most commonly missed fractures by emergency medicine physicians.(2) Though elbow fractures, such as an intra-articular radial head fracture, are not high in volume, we misdiagnose them at such a large rate that they still qualify as one of the most commonly missed fractures. In turn, this leads to misdiagnosed elbow fractures being some of the most highly litigated cases of malpractice affecting emergency physicians. One study remarked that although only about 4% of pediatric fractures tend to occur at the elbow, they accounted for roughly 20% of all malpractice litigation proceedings.(3) Thus, it is important to understand how to adequately obtain a reliable exam, proper radiographic imaging, and interpret these results in order to avoid this common pitfall and ultimately benefit the patient.
How do we classify radial head fractures?
Traditionally, traumatic radial head fractures are organized using the Mason Classification system (Table 1).(4) This system accounts for multiple variables including extent of displacement, comminuted vs. non-comminuted, presence or absence of mechanical block, and association with dislocation. Interestingly, this classification system can be used diagnostically and prognostically, and to guide therapeutic management. It also features both radiographic and physical exam findings.

The presence or absence of a mechanical block can help distinguish operative vs. non-operative therapeutic management and can be the difference between sling and discharge vs. admission and surgery.(4) A Mason Type I fracture also does not require a long-arm cast but rather sling placement for 48 hours followed by relatively early mobilization.(4)
What makes the pediatric elbow so special?
As the saying goes, “children are not just smaller adults,” and the pediatric elbow is no exception. The pediatric elbow contains 6 ossification centers that present in a distinct order. One mnemonic has been used to help identify the correct order in which they appear: C.R.I.T.O.E., which stands for Capitellum, Radial head, Internal (or medial) epicondyle, Trochlea, Olecranon, and External (or lateral epicondyle).(5) This mnemonic is in chronological order in which these locations ossify, making them visible on radiographs (Table 2).
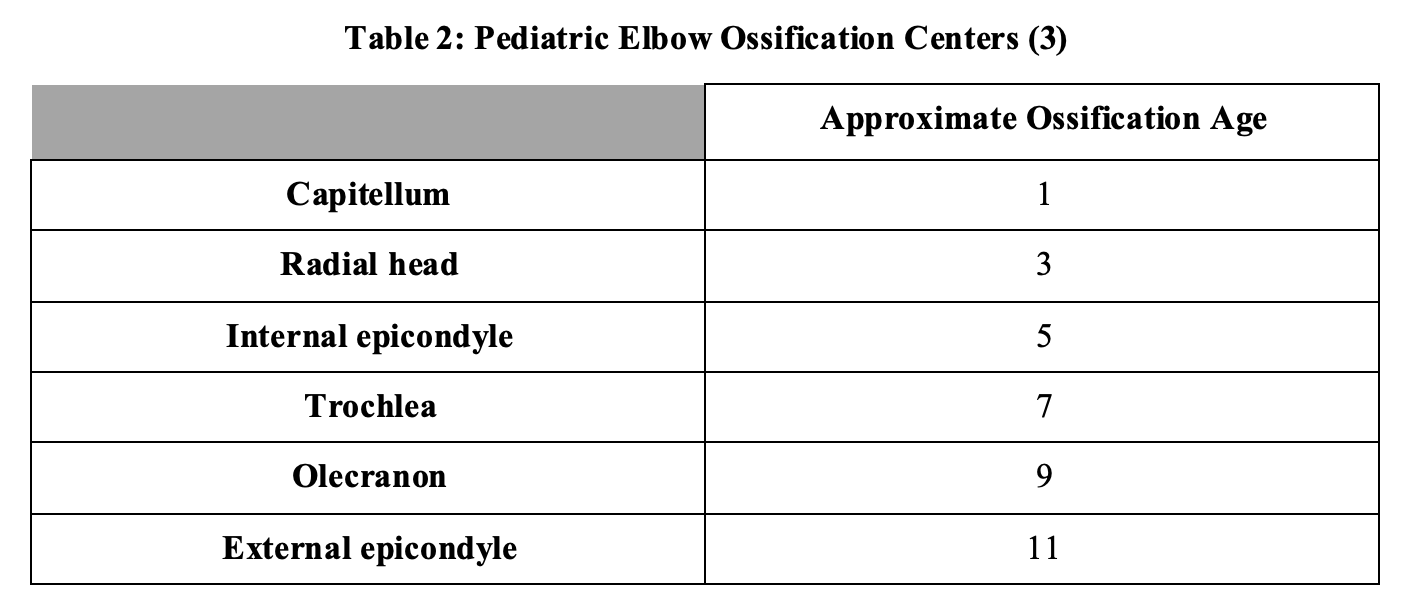
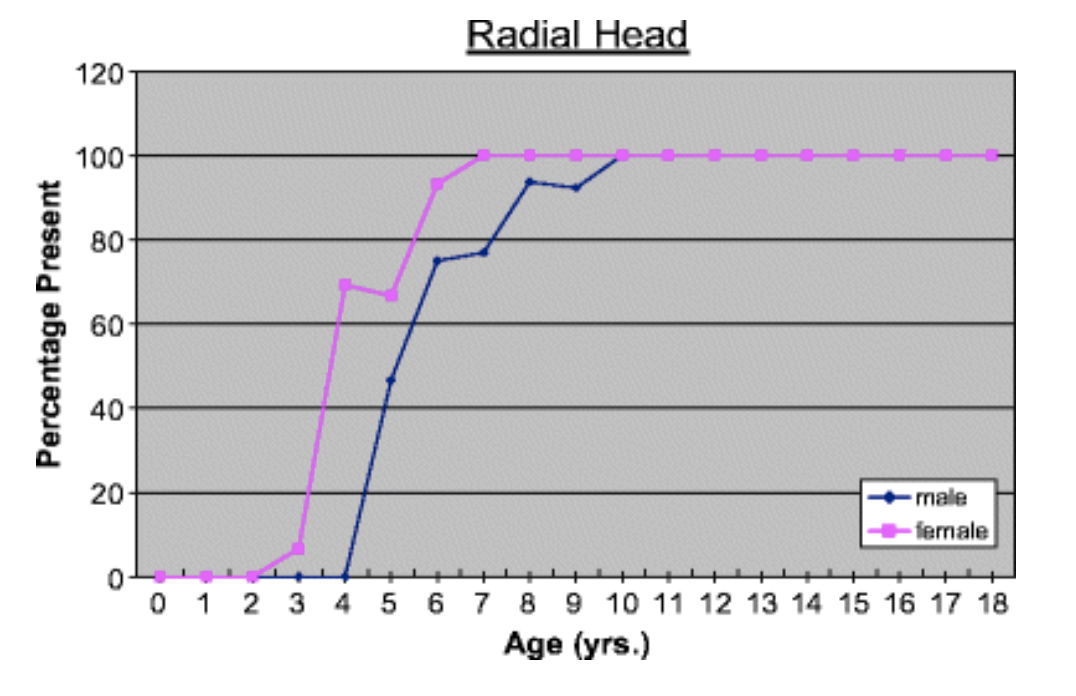
Another easy way to remember this is by pairing each ossification center with an odd number in ascending order. Though some variability exists among males and females within their respective genders, generally speaking, the elbow ossification centers of females tend to appear earlier than those of males as exhibited by Figure 2.(5)
Figure 2: Gender Differences in Appearance of Elbow Ossification Centers (5)
It is not just important to be aware of these ossification centers and the approximate ages at which they radiographically appear but it is also useful in the identification of occult ossification center fractures. For example, if a trochlear ossification center in an 8-year-old child is seen on x-ray but the internal (medial) epicondyle ossification center is not found, then one must suspect a medical epicondyle ossification center fracture-dislocation that displaced it from its normal anatomical location.(6)
Equally important as knowing when to start seeing these ossification centers on x-ray is when to know when to stop seeing them. This is otherwise known as the time they fuse together and are no longer visualized as independent structures. Similar to when they are initially ossified, there is a mnemonic that can aid in remembering the times at which they fuse: CTE-R-O-I. The Capitellum, Trochlea, and External (lateral) epicondyle ossification centers all fuse as one around the age of puberty (ages 12-14), followed by the Radial head (ages 14-16), the Olecranon (ages 15-17), and finally the Inernal (medial) epicondyle ossification center (ages 16-18).(4)
Figure 3: Below is an image of a 10 year old child with the CRITOE ossification centers
labeled. (7)

What are tips on how to obtain an optimal exam when evaluating an intra-articular radial head fracture?
It is of the utmost importance to obtain the best possible physical exam on these patients in order to determine correct treatment and disposition. But as with most fractures and especially those in the pediatric population, pain can be a significant barrier. Fortunately, accessing the elbow joint in a single location can accomplish two tasks that aid in optimizing an exam. First, after the area is cleansed with betadine or chlorhexadine and a wheel of local anesthetic is placed subcutaneously beneath where the needle will be inserted, blood can be aspirated from the elbow joint.(8,9) When attempting to aspirate or inject into the elbow joint capsule, it can be accessed by entering the area between the olecranon, radial head, and lateral epicondyle of the humerus as demonstrated by Figure 3. (9,10)
Figure 4: Accessing the Elbow Joint Using Anatomical Landmarks(9)
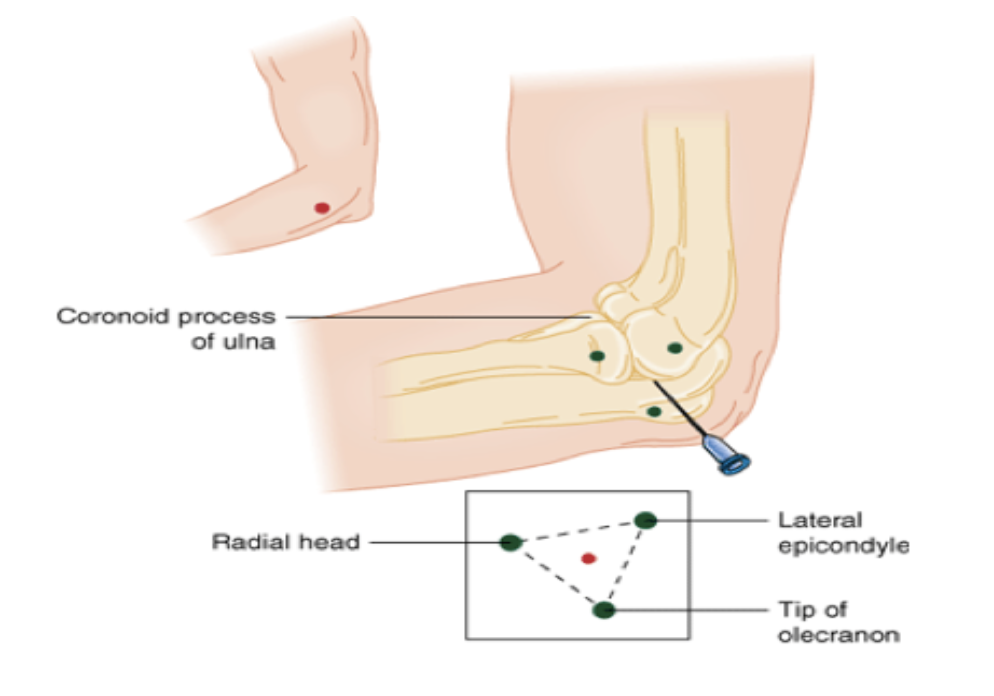
Successful aspiration of blood not only confirms proper placement within the joint itself but also serves to alleviate accrued pressure in the normally empty space, which is contributing to the patient’s discomfort.(11) When no more blood can be evacuated from the joint, the needle is held in place while a second syringe with local anesthetic is attached. From there, about 5mL of a local anesthetic such as lidocaine can be inserted for further pain relief. This effectively acts as a hematoma block for the intra-articular fracture.(11) Once blood has been aspirated from the hematoma and local anesthetic has been injected, the patient should have less discomfort and be able to fully range the elbow if there truly is no mechanical block.
Take Home Points:
- The pediatric elbow joint is distinct because of its six ossification centers and whether or not they appear on x-ray depends on the ages at which they ossify and fuse.
- The presence of a mechanical block can be the difference between surgery and conservative management for intra-articular radial head fractures.
- Associated pain and hematoma within the elbow joint resulting from intra-articular radial head fractures can inhibit the ability to perform an optimal exam
- Intra-articular elbow joint hematoma aspiration and injection of local anesthetic can provide substantial pain relief and increases likelihood of an optimal exam
Further Reading:
- NUEM Blog: A Visual Guide to Upper Extremity Joint Aspirations
- EM Cases – Elbow Injuries – Ten Pitfalls in Diagnosis and Management
- EM in 5: Elbow X-rays
- CORE EM: Radial Head Fracture
References:
- Black, W. Scott, and Jonathan A. Becker. “Common Forearm Fractures in Adults.” American Family Physician, 15 Nov. 2009, www.aafp.org/afp/2009/1115/p1096.html.
- Freed, Howard A, and Naomi N Shields. “Most Frequently Overlooked Radiographically Apparent Fractures in a Teaching Hospital Emergency Department.” Annals of Emergency Medicine, vol. 13, no. 10, 1984, pp. 900–904., doi:10.1016/s0196-0644(84)80666-6.
- Vinz, Heinrich, and Johann Neu. “Out of Court Settlement of Malpractice Claims Relating to the Treatment of Fractures in Children: Experience of the Arbitration Board of the North German Medical Associations.” Deutsches Arzteblatt International, Deutscher Arzte Verlag, July 2009, www.ncbi.nlm.nih.gov/pmc/articles/PMC2735703/.
- Burkhart, Klaus Josef, et al. “Fractures of the Radial Head.” Hand Clinics, vol. 31, no. 4, 2015, pp. 533–546., doi:10.1016/j.hcl.2015.06.003.
- Girdany, R. Golden, et al. “Gender-Specific Pattern Differences of the Ossification Centers in the Pediatric Elbow.” Pediatric Radiology, Springer-Verlag, 1 Jan. 1970, link.springer.com/article/10.1007/s00247-008-1078-4.
- Skaggs DL: Elbow fractures in children: diagnosis and management. J Am Acad Orthop Surg 5: 303, 1997. [PMID: 10797226]
- Özdemir , M., et al. “X-Elbow.” Startradiology, 30 June 2016, www.startradiology.com/internships/general-surgery/elbow/x-elbow/index.html.
- Wimberly RL. General principles of managing orthopedic injuries. In: Herring JA, ed. Tachdjian’s Pediatric Orthopaedics. 5th ed. Philadelphia, PA: Elsevier; 2014:1199-1223.e7.
- Foocharoen T, Foocharoen C, Laopaiboon M, Tiamklang T. Aspiration of the elbow joint for treating radial head fractures. Cochrane Database Syst Rev. 2014 Nov 22. 11:CD009949.
- Ford, Will, and Amy Ford. “A Visual Guide to Upper Extremity Joint Aspirations.” NUEM Blog, NUEM Blog, 7 May 2018, nuemblog.com/blog/joint-aspiration?rq=arthrocentesis.
- Ditsios, Konstantinos T., et al. “The Effect of Haematoma Aspiration on Intra-Articular Pressure and Pain Relief Following Mason I Radial Head Fractures.” Injury, vol. 42, no. 4, 2011, pp. 362–365., doi:10.1016/j.injury.2010.09.003.








