Authors: Zachary Sletten, MD (EM Attending, Brooke Army Medical Center) and Simon Sarkisian, DO (EM Attending, Cooper University Hospital/US Army, Camden, NJ) // Reviewed by: Alexander Y. Sheng, MD, MHPE (@theshenger); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
You are a busy emergency medicine (EM) attending physician, and you hear about a facial laceration that just checked in. The intern asks you for help repairing the laceration, and you eagerly accompany them into the room excited to endow them with your wisdom on laceration repair. After stepping into the room, you realize you might be in over your head (no pun intended). This is not your run of the mill facial laceration.
The series will review the repair of head, eyes, ears, nose, and throat (HEENT) lacerations, with a focus on the areas where emergency physicians tend to struggle. Today we look at general principles, followed by a discussion of scalp lacerations.
General Principles
When evaluating facial lacerations, be sure to assess for additional injuries to include cranial nerve injuries. Repair should prioritize good alignment and cosmesis. Regional nerve blocks may be preferred over local anesthesia to avoid distortion of tissue. The face and scalp are highly vascular and thus unlikely to get infected. Repair can be safely performed up to 24 hours after the injury (even for dog bites)1. There is even evidence that wounds closed within 6 hours do not benefit from irrigation2. Non-gaping facial wounds <3 cm can be repaired with simple interrupted sutures in non-layered fashion without compromising cosmetic outcome3. Alternatively, for simple linear lacerations in low tension areas, tissue adhesive (glue) can be used without compromising cosmetic outcome4,5. If a layered repair seems indicated, subcutaneous sutures can be used to relieve surface tension. Non absorbable sutures (5-0/6-0) are used for repair of the epidermis and absorbable sutures (4-0/5-0) are used for mucosal repair and deep buried sutures. There is a somewhat nuanced approach to repair of the various areas of the face which will be discussed below along with review of indications for surgical consultation.
Case
A 46-year-old construction worker presents after falling from a ladder with a laceration overlying his occipital scalp. It’s oozing blood, and you try to remember how to find and repair the galea.
Scalp Lacerations

Proper management of scalp lacerations requires an understanding of the skin layers. See figure 1 above for review of the anatomy. Unless the entire outer layer, composed of the skin, superficial fascia and galea are traversed, scalp lacerations generally will not be gaping6. When evaluating a gaping wound, which raises concern for laceration through the entire outer layer, the galea itself is often difficult to appreciate and the thin periosteum (which cannot be sutured) is often mistaken for the galea. Be sure to probe with a sterile gloved finger to evaluate for fracture1. The emissary veins which are tethered open due to their connection to the connective tissue, and therefore cannot retract, may cause persistent bleeding and are also a portal for infection to enter the central nervous system and skull. For this reason, and because of the role the galea has in a symmetric eyebrow raise, repair of the galea is important. Bleeding can interfere with repair and direct pressure, everting the galea with forceps, figure-of-8 suture and lidocaine with epinephrine all can help to control bleeding for repair. Brushing the hair aside or matting it down with ointment is preferred to clipping in order to reduce the risk of infection. Repair using single, simple interrupted 3-0/4-0 non-absorbable sutures making sure to include subcutaneous fascia and galea6. As mentioned, the galea itself can be difficult to identify and buried sutures can serve as a nidus for infection so are avoided if possible. If you are able to find the galea, and a defect greater than 5mm is identified, you can attempt layered repair with 3-0 or 4-0 absorbable sutures7,8. When repairing the scalp, consider leaving long tails (potentially with a different color than the hair) to help during follow-up. Scalp wounds can be safely repaired up to 24 hours after injury.
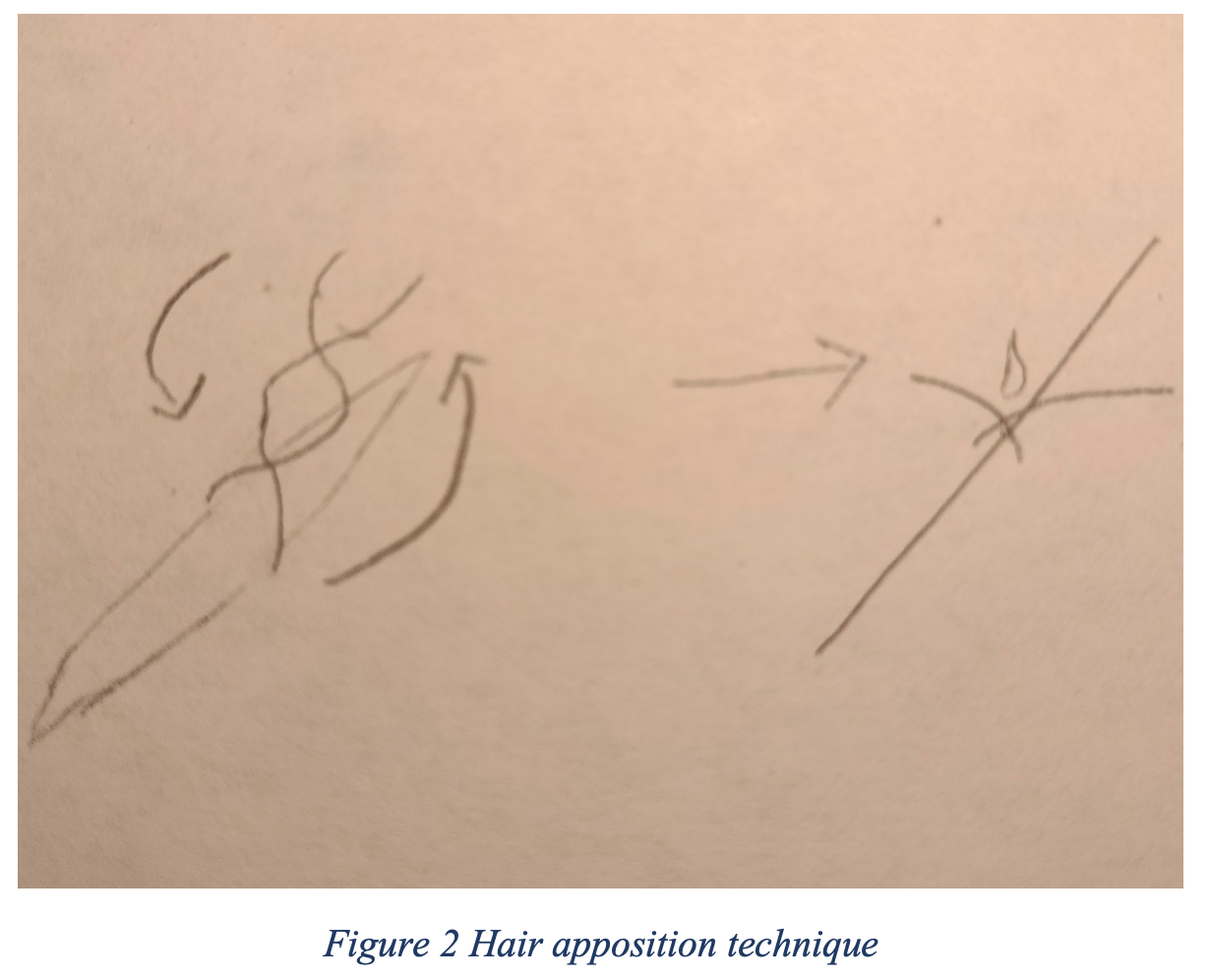
For smaller (<10 cm), simple, shallow lacerations that are hemostatic, the hair apposition technique can be considered instead of staples or simple interrupted sutures. The hair apposition technique is associated with a reduction in complications and increased satisfaction compared to staples and sutures9. This technique involves twisting 4-5 hairs that are at least a centimeter in length and then gluing the hair together, taking care not to glue the scalp/wound itself (depicted below in figure 2). For shorter hair, a clamp can be used to grasp 5-15 hairs to perform the same technique. Patients should be encouraged to avoid showering/bathing for 2 days6.
When repairing the eyebrow, avoid shaving or clipping and be fastidious about lining up hair margins. Consider a supraorbital nerve block for anesthesia10.
Stay tuned for our next piece in the series on repair of ear lacerations.
References/Further Reading
- Tintinalli JE, Ma OJ, Yealy DM, et al. Tintinalli’s emergency medicine: a comprehensive study guide. 2020.
- Hollander JE, Richman PB, Werblud M, Miller T, Huggler J, Singer AJ. Irrigation in facial and scalp lacerations: does it alter outcome? Ann Emerg Med 1998;31:73-7.
- Singer AJ, Gulla J, Hein M, Marchini S, Chale S, Arora BP. Single-layer versus double-layer closure of facial lacerations: a randomized controlled trial. Plast Reconstr Surg 2005;116:363-8; discussion 9-70.
- Farion KJ, Russell KF, Osmond MH, et al. Tissue adhesives for traumatic lacerations in children and adults. Cochrane Database of Systematic Reviews 2002.
- Holger JS, Wandersee SC, Hale DB. Cosmetic outcomes of facial lacerations repaired with tissue-adhesive, absorbable, and nonabsorbable sutures. Am J Emerg Med 2004;22:254-7.
- Roberts JR, Custalow CB. Roberts and Hedges’ clinical procedures in emergency medicine and acute care. 2019.
- Assessment and Management of Intra-Oral Lacerations. 2020. (Accessed 25 JUL, 2020, at https://www.uptodate.com/contents/assessment-and-management-of-intra-oral-lacerations?search=Assessment%20and%20Management%20of%20Intraoral%20Lacerations&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1.)
- Scalp Laceration Repair. 2020. (Accessed 18 JUL, 2020, at https://www.emrap.org/episode/emrap20203/scalplaceration.)
- Ozturk D, Sonmez BM, Altinbilek E, Kavalci C, Arslan ED, Akay S. A retrospective observational study comparing hair apposition technique, suturing and stapling for scalp lacerations. World J Emerg Surg 2013;8:27.
- Sabatino F, Moskovitz JB. Facial wound management. Emerg Med Clin North Am 2013;31:529-38.








