Authors: Jason Wong, MD (EM Resident Physician at University of Washington), Matthew Valento, MD (Medical Toxicologist at Washington Poison Center and University of Washington) and Jeff Riddell, MD (@Jeff__Riddell – EM Attending Physician / Education Research Fellow at University of Washington) // Edited by: Alex Koyfman, MD (@EMHighAK – EM Attending Physician, UT Southwestern Medical Center / Parkland Memorial Hospital) and Manpreet Singh, MD (@MPrizzleER – Assistant Professor of Emergency Medicine / Department of Emergency Medicine – Harbor-UCLA Medical Center)
Case: A 34-year old female presents with altered mental status. She was found this morning by her roommate significantly agitated. The roommate states that the patient initially had slurred speech and appeared uncomfortable. She was unable to answer questions and was mumbling and jittery. The roommate notes that the patient has a history of depression. She was last seen acting normally last night, although did she go out for a few drinks with friends last night.
Vitals: T: 37.8 BP: 152/120 HR: 154 RR: 20 Sat: 100% on RA
Exam is most notable for dilated pupils. Skin appears dry with mild facial flushing. No significant clonus or rigidity. She is alert and oriented x 1, unable to answer other questions. No nuchal rigidity and no other focal neurologic deficits. No signs of trauma.
While the differential in our case is broad, we will focus on the workup for toxic overdoses, specifically on a few of the common silent killers that can have life-threatening consequences if not managed appropriately. We will provide clinical pearls for presentation and management of these life-threatening overdoses.
Acetaminophen Toxicity
Acetaminophen (also known as APAP or paracetamol) is one of the most common toxic overdoses and is the most common cause of acute liver failure in the United States. Despite wide prevalence of use and high mortality risks, if identified and treated early, mortality rates are very low.1
Presentation
Classically, there are 4 stages of acetaminophen toxicity, although high clinical variability exists, depending on drug formulation, co-ingestions and pre-existing comorbidities. In Stage I, the patient may present with vague symptoms of nausea and vomiting, but will likely have normal LFTs. In Stage II, the patient may be asymptomatic. Thus, a thorough history is crucial.2,3
| Stage | Post-ingestion time | Clinical features | Laboratory Abnormalities |
| I | < 24 hours | Nausea, anorexia, vomiting, fatigue, diaphoresis | Typically normal LFTs, although may see increased, may have metabolic acidosis |
| II | 24 – 72 hours | RUQ pain and tenderness, possible hepatomegaly, may even be asymptomatic | Elevated LFTs, elevated BUN and creatinine, elevated INR |
| III | 3 – 5 days | Jaundice, hypoglycemia, coagulopathy, lethargy, confusion, coma (from significant encephalopathy) and even death. | Acute tubular necrosis with increased BUN and Creatinine, increased LFTs, increased INR, decreased glucose, decreased pH |
| IV | > 5 days | Recovery phase with improving of symptoms | Improving LFTs |
The above image is adapted from Defendi, GL 2013.
Diagnostics
Treatment guidelines are based on a timed serum acetaminophen concentration plotted on the modified Rumack-Matthew nomogram, which starts at 4 hours post-ingestion for acute ingestions. Patients that fall above the treatment line should be treated with N-acetylcysteine (NAC). However, in many of these patients, the time of ingestion is unknown. NAC can also be administered if:
- History is highly suspicious of overdose in the setting of acute liver failure or markedly elevated transaminases.
- Repeated supratherapeutic ingestions with detectable serum acetaminophen and significant hepatic injury

The above image is from Defendi, GL 2013. It includes the original Rumack-Matthew Nomogram. It displays a logarithmic graph of hours (post-ingestion) on the X-axis and acetaminophen concentration on the Y axis (ug/mL). The lower line was added on in 1981 from the FDA’s request to include a 25% margin of error.2,4,5
Treatment
NAC – NAC is the accepted antidote for acetaminophen poisoning. If given within 8 -10 hours of overdose, serious hepatotoxicity is uncommon and death is extremely rare. NAC is available in oral and IV formulations, with no studied differences between the two. Thus, the IV formula is the preferred route of administration.
150mg/kg IV loading dose in the first hour
50mg/kg IV over the next four hours
100mg/kg IV over the 16 hours3
In the rare occasion that IV formula is not available, may start PO administration at 140mg/kg in the first four hours, followed by 70mg/kg every 4 hours for additional 17 doses. May administer with soft drink for flavoring and Zofran to reduce nausea.
The actual duration of therapy varies, as many toxicologists recommend a patient-tailored approach to cessation of NAC including the following clinical criteria: a negative acetaminophen level, normal or improving serum ALT, and improved clinical status. However, this should be discussed with your toxicologist or Poison Control Center.6
After administration of NAC, monitor for anaphylactoid reactions.7 If symptoms are too severe, the IV NAC should be discontinued and either resumed at a lower rate or switched to PO, if patient is able to tolerate.
King’s College Criteria – If you are not working at a large tertiary medical center, King’s College Criteria can be used to asses risk of fulminant hepatic failure and thus the need for referral to a transplant center.
- pH<7.3 or lactate>3 at 12 hours despite adequate fluid resuscitation OR
- All of the below:
- Creatinine > 3.4
- INR > 6.5 (avoid FFP/Vitamin K if no active bleeding to monitor INR)
- Grade 3 or 4 hepatic encephalopathy, based on the West Haven Hepatic Encephalopathy grading8
Pearls and Pitfalls
- There are various clinical presentations of acetaminophen overdose, including asymptomatic, vague nausea/vomiting, acute liver failure, and even coma. A thorough history, in combination with laboratory data, is crucial for diagnosis.
- Rule of 150s =>
- Toxic dose is approximately 150mg/kg
- Treatment with NAC should be implemented if >150 mg/kg acetaminophen level at 4 hours of presentation
- Initial dose of IV NAC is 150 mg/kg in the first hour.
- If you are working in a community hospital, consider transfer to a transplant center early if the patient has evidence of severe toxicity (King’s College criteria) or if there is worsening clinical status despite treatment.
Salicylate Toxicity
The most common salicylate is aspirin, also known as acetylsalicylic acid (ASA). Other sources of salicylate overdose include: oil of wintergreen (methyl salicylate), BenGay (topical methyl salicylate), and PeptoBismol (bismuth subsalicylate).
Presentation
The classic presentation is a combined respiratory alkalosis (earliest sign) with anion gap metabolic acidosis with the development of a metabolic contraction alkalosis later (triple mixed acid-base disturbance). Other common symptoms include nausea, vomiting, tinnitus, vertigo, and diarrhea. In severe cases, patients may develop non-cardiogenic pulmonary edema, hyperthermia, altered mental status, seizures, and coma.9
Diagnostics
Do NOT forget to draw an aspirin level for patients with altered mental status! The therapeutic range of aspirin is between 10-30 mg/dL, but patients can experience tinnitus between 25 to 45mg/dL.
There are no strict guidelines for when to start treatment, but levels above 40 mg/dL or systemic signs of toxicity should prompt initiation of therapy, while levels above 90 mg/dL may require urgent hemodialysis. Remember to obtain an ABG/VBG with lactate to evaluate acid/base status, electrolytes to determine an anion gap and evaluate renal/hepatic function.
Treatment
Although, ABCs are the initial primary management in all patients in the Emergency Department, AVOID INTUBATION if possible! Patients require their own high minute ventilation to prevent worsening of the metabolic acidosis.
- If intubating, optimize conditions to decrease the apneic period and set a minute ventilation to match the patient’s minute ventilation. (sometimes up to 30 L/min)10. Consider sodium bicarbonate bolus prior to intubation.
Decontamination with activated charcoal (if tolerated) is effective. Administer charcoal within 4 hours of ingestion, of 1g/kg, and if patients tolerate, for a total of 2-4 doses q4h.11 Whole-bowel irrigation should be reserved for large amounts of enteric-coated or extended-release forms
Sodium bicarbonate is essential in treating aspirin overdoses. It works through two mechanisms: urinary alkalinization for enhanced elimination, and increasing the proportion of ionized salicylate, which will not cross cell membranes to exert toxic effects at target organs (especially the CNS).
- Administer 1 to 2 meq/kg as an IV bolus, typically 1 to 2 amps of bicarbonate. This should be followed by 3 amps of bicarb in D5W at 2-3 cc/kg/hr or around 250 cc/hr, typically for 4-8 hours.3
- Be sure to correct hypokalemia caused by the sodium bicarbonate for improved urinary alkalinization.
- Goals: Blood pH 7.50 – 7.55 , Urine pH 7.5-8
Dialysis is the next step in treatment and is reserved for severe aspirin toxicity. Indications for dialysis include:3,12
| Altered mental status / seizures |
| ARDS / Hypoxemia |
| Salicylate level > 90mg/dL |
| Severe acidemia < 7.2 |
| Kidney Failure |
| Hypotension / Hemodynamic instability |
Pearls and Pitfalls
- Start treatment for aspirin overdose at 40 mg/dL or signs of systemic illness with charcoal (if patient tolerates) and sodium bicarbonate
- If salicylate levels > 90 mg/dL, AMS, significant organ dysfunction, pH < 7.2, or hemodynamic instability => emergent hemodialysis
- If possible, avoid intubation! But if intubation is necessary, attempt to match the patient’s minute ventilation!
Tricyclic Antidepressant (TCA) Toxicity
Tricyclic antidepressants (TCAs) have been used since the 1950s for depression, and include drugs such as imipramine, clomipramine, desipramine, doxepin, nortriptyline, amitriptyline, imipramine, and trimipramine. With the advent of new psychiatric drugs (SSRI, SNRI, etc.), they have become useful for neuropathic pain.
Presentation
TCAs can present with nonspecific symptoms ranging from severe agitation and confusion to significant sedation, coma, and hypotension. This wide spectrum of clinical effects results from blockade on numerous receptors including: norepinephrine/serotonin reuptake, muscarinic acetylcholine receptors, alpha-1 adrenergic receptors, sodium channels, and anti-histamine receptors. Addressed below are some of the toxic effects:
TCA toxicity3
| CNS | Altered mental status, seizures, delirium which can progress to lethargy and coma |
| Anti-cholinergic | Dilated pupils, dry mouth, dry skin, flushed and hot, urinary retention, ileus |
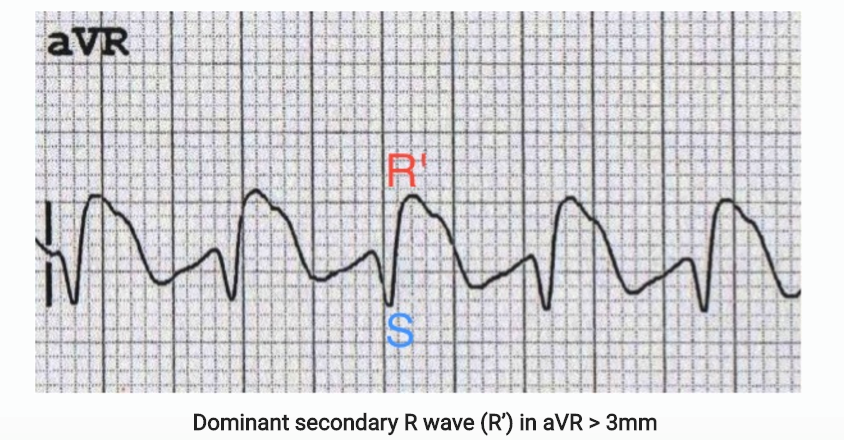
| Cardiac | Typically, patients typically present with sinus tachycardia. However, TCAs also have sodium channel blockade properties, with classic EKGs findings (see below)
– widened QRS (>120ms) with interventricular conduction delays, – terminal R wave > 3mm in aVR – potentially ventricular dysrhythmias.13 Myocardial depression can lead to refractory hypotension. |
Diagnostics
The most important diagnostic test for TCA overdose is an EKG and telemetry to monitor for interval changes or arrhythmias. Serial EKGs after treatment are necessary to monitor QRS intervals!
Treatment
Intravenous fluid boluses are the initial treatment for hypotension. Activated charcoal should be administered if within 4 hours of ingestion.
Sodium bicarbonate is the primary treatment for QRS widening, arrhythmias, or hypotension associated with TCA overdoses. A normal QRS interval is < 100ms, but some toxicologists will start treatment when the QRS > 120ms. Nevertheless, administering sodium bicarbonate for QRS > 100 ms is appropriate.14
- Bicarbonate is administered at 1-2 meq/kg, which is around 2-3 amps of bicarbonate. This dose may be repeated after 5 minutes, until the QRS interval narrows and the hypotension resolves.
- After 3 doses of bicarbonate, may start a bicarbonate drip with D5W + 3 amps at a rate of 250 cc/hr, and this is typically continued 12-24 hours after the EKG has normalized.3
For refractory arrhythmias, consider lidocaine or magnesium sulfate. For seizure activity, a benzodiazepine, such as lorazepam, may be used.
You may consider intravenous lipid emulsion (ILE) therapy as last resort treatment for severe life-threatening toxicity with hemodynamic instability refractory to sodium bicarbonate. However, discussion with a toxicologist should take place prior to starting.15
Pearls and Pitfalls
- TCA toxicity can present with seizures, tachycardia, hypotension, anticholinergic toxicity, and coma.
- The most common dysrhythmia is sinus tachycardia but the classic EKG findings include cardiac conduction delays, terminal R wave in aVR, and a widened QRS.
- Treat initially with IVF resuscitation and sodium bicarbonate when QRS > 100ms or for hemodynamic instability.
- Last resort therapies for refractory arrhythmias with significant toxicity include lidocaine, magnesium, and intravenous lipid emulsion.
Iron Toxicity
Iron toxicity is most common following overdose of iron salt preparations, such as ferrous gluconate and ferrous sulfate, and other vitamin preparations, especially prenatal vitamins. Fortunately, the incidence of iron poisoning has significantly decreased with improved FDA regulations regarding packaging, education, and dosing. However, iron toxicity still occurs and it is important to recognize the presentation for appropriate management.
Presentation
There are typically 5 clinical stages of iron poisoning (see table below). Note that in stage 2 there may be a transient resolution of symptoms.
From Madiwale and Liebelt 2006, showing the 5 clinical stages of iron poisoning16
Diagnostics
The main diagnosis of iron toxicity will be a clinical diagnosis obtained from history and laboratory data/images. Serum iron concentrations will be helpful primarily to predict toxicity and treatment efficacy. An abdominal XR may be useful to evaluate for pills or pill fragments (iron tablets are typically radiopaque). However, this will not tell you about the concentration or exact size of the ingestion.
Iron Toxicity3
| Serum Iron Concentrations (mcg/dL) | Toxicity |
| 300 – 500 | GI toxicity and modest systemic toxicity |
| 500 – 1000 | Pronounced toxicity and shock |
| > 1000 | Sever toxicity with significant morbidity and mortality |
Additional tests to order include: CBC to evaluate for anemia, ABG/VBG with lactate and electrolytes to evaluate for anion-gap acidosis, and LFTs/coags to evaluate for hepatic dysfunction.
Treatment
For iron levels < 300 mcg/dL, you may observe the patient for 6 hours, and if they remain completely asymptomatic, the patient may be discharged.
Initial treatment for iron toxicity is supportive care including anti-emetics and IVFs for volume loss from GI symptoms. Consider whole bowel irrigation for larger ingested quantities with visible pills in the stomach on XR (NG tube with polyethylene glycol with up to 500 cc/hr in children or up to 2L/h in adults, until rectal effluent is clear.)17
Remember: activated charcoal will NOT bind iron
Deferoxamine is the primary treatment for iron overdose. After administration, the ferric ion excretes in the urine, usually causing a vin rose urine, which may assist in treatment management. By following the urine color change from pre and post deferoxamine, the resolution of color change may indicate very little excretion of the iron metabolite or completion of treatment. However, this is not always a reliable marker.
Table: Indications for deferoxamine3
| Hypotension / shock |
| Lethargy / coma |
| Persistent GI symptoms |
| Anion gap metabolic acidosis |
| Serum iron levels > 500 ug/dl |
- Deferoxamine – dose at 5 mg/kg/hour titrate up to 15 mg/kg/hour as tolerated
- Discuss with your toxicologist about duration of treatment and adjusting the rate after the initial 1g is administered, as current recommendations limit dosing to 6-8g within the first 24 hours.
- Side effects:
- Hypotension (attempt to lower the rate of infusion)
- Pulmonary toxicity / ARDS – Typically administration of deferoxamine is limited to 24 hours secondary to significant pulmonary toxicity
- Atypical infections (e.g. Yersinia)
- Side effects:
Pearls and Pitfalls:
- Charcoal will NOT be beneficial in iron overdose.
- Criteria for treatment with deferoxamine are hypotension/shock, CNS symptoms, AG metabolic acidosis, serum iron levels > 500 ug/dl or persistent GI symptoms
- Deferoxamine has the potential for significant hypotension and pulmonary toxicity. Discuss treatment dosing and duration with your toxicologist.
Case Review:
Upon arrival, patient was noted to have an anticholinergic toxidrome with dilated pupils, hot, dry skin, and altered mental status. There was initial concern for a diphenhydramine overdose with alcohol use. Fingerstick blood sugar was normal, with negative blood alcohol level. However, the initial EKG showed a widened QRS of 140ms. Further history revealed that the patient had previously been prescribed a TCA. Patient was given IVFs, benzodiazepines for agitation and bicarbonate boluses q5 minutes x 2 doses with immediate response of QRS < 100ms. She was subsequently started on a bicarbonate infusion and transferred to the ICU.
When evaluating most emergency department patients, you should have toxic overdose on your differential. A good HPI is crucial as are the ECG, serum acetaminophen and salicylate levels. “Silent Killers” can be missed if the correct history and workup are not completed. This can have fatal consequences.
Resources / Further Reading
- Bunchorntavakul C, Reddy KR. Acetaminophen-related hepatotoxicity. Clin Liver Dis 2013; 17:587.
- Defendi GL. Consultant For Pediatricians. 2013; 12(7):299-306.
- Goldfrank LR et al. Goldfrank’s Toxicologic Emergencies 10e. McGraw Hill Education. 2015
- Rumack BH, Matthew H. Acetaminophen poisoning and toxicity. Pediatrics. 1975;55(6):871-876.
- Rumack BH, Peterson RC, Koch GC, Amara IA. Acetaminophen overdoses: 662 cases with elevation of oral acetylcysteine treatment. Arch Intern Med. 1981:141(3)380-385
- Dart RC and Rumack BH. Patient-Tailored Acetylcysteine Administration. Annals of Emergency Medicine 2007:50:3
- Dawson AH, Henry DA, McEwen J. Adverse reactions to N-acetylcysteine during treatment for paracetamol poisoning. Med J Aust 1989; 150:329.
- O’Grady JG, Alexander GJ, Hayllar KM, Williams R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology 1989; 97:439.
- O’Malley GF. Emergency department management of the salicylate-poisoned patient. Emerg Med Clin North Am 2007; 25:333.
- Greenberg MI, Hendrickson RG, Hofman M. Deleterious effects of endotracheal intubation in salicylate poisoning. Ann Emerg Med 2003; 41:583.
- Barone JA, Raia JJ, Huang YC. Evaluation of the effects of multiple-dose activated charcoal on the absorption of orally administered salicylate in a simulated toxic ingestion model. Ann Emerg Med 1988; 17:34.
- Juurlink DN, Gosselin S, Kielstein JT, et al. Extracorporeal Treatment for Salicylate Poisoning: Systematic Review and Recommendations From the EXTRIP Workgroup. Ann Emerg Med 2015; 66:165.
- Burns, E. Tricyclic Overdose (Sodium-Channel Blocker Toxicity). Life in the Fastlane. Updated 7/4/2016.
- Boehnert MT, Lovejoy FH Jr. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med 1985; 313:474.
- Levine M, Brooks DE, Franken A, Graham R. Delayed-onset seizure and cardiac arrest after amitriptyline overdose, treated with intravenous lipid emulsion therapy. Pediatrics 2012; 130:e432.
- Madiwale T, Liebelt E. Iron: not a benign therapeutic drug. Curr Opin Pediatr 2006; 18:174.
- Tenenbein M. Whole bowel irrigation in iron poisoning. J Pediatr 1987; 111:142.









1 thought on “Tox Silent Killers”
Pingback: Länkar v23 | Internmedicin