Author: Kyrillos Attaalla, 4th year medical student (Rutgers New Jersey Medical School, Newark NJ) and Cynthia Santos MD (Assistant Professor Emergency Medicine, Medical Toxicology, Rutgers New Jersey Medical School) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital), and Brit Long, MD (@long_brit, EM Attending Physician, San Antonio Military Medical Center)
Case:
A 17-year-old boy with no past significant medical history is brought into the ED by his parents for erratic behavior at home. The patient has been missing school and not doing his homework. Today he was found sitting in the corner of his room with small silver containers scattered around him, and he seemed slow to respond when questioned by his mother. In the ED the patient is alert and fully oriented, and his vital signs are normal. The neurological examination is significant for a nystagmus, spasticity, ataxic gait, and diminished sensation of pressure, vibration, and touch. There also appears to be erythema on the oral and nasal mucosa. Basic laboratory tests are unremarkable except for a macrocytic anemia with a hemoglobin or 10.1 g/dL and MCV of 109 μm3.
Questions:
- What are these containers, and what do they contain?
- What are the signs of abuse?
- What is the management?
Background:
- Nitrous oxide has a long history of use. It was the first anesthetic agent and is still used in the OR and ED safely. The agent is typically mixed with oxygen.
- A whipped cream charger (aka whippit or whippet) is a steel cylinder cartridge that is filled with nitrous oxide (N2O) and is used as a whipping agent for whipped cream dispensers, See figure 1.
- N2O can also be found in spray containers of whipped cream sold in supermarkets and can be bought as tanks or cylinders (e.g., race cars, medical gases).
- Commercial N2O anesthesia machines limit the inhaled mixture to no less than 40% oxygen.
- There are various methods for inhalation that N2O abusers employ.
- By using a “cracker” and a large balloon, the user can open a N2O canister and release the gas into the balloon. The user then inhales the contents of the balloon.
- Abusers can also inhale N2O “straight from the tap” by using a cracker with the N2O canisters. The escaping gas gets very cold as it expands and can freeze tissue on contact.
- Larger tanks of the gas that can be legally purchased for food-related use can be attached to a facemask to allow continuous breathing.
- Users may try to reuse N2O (to save money) by exhaling into someone else’s mouth, or by exhaling into a bag or balloon for reinhalation.
- Reuse reduces the available O2 while increasing CO2 and makes hypoxia more likely.
- Certain occupations are at risk of chronic N2O exposure or abuse, such as [1]:
- Dental workers
- Surgical room and recovery room medical personnel or service workers
- Workers in laboratories where compressed gas cylinders are stored
Clinical Effects:
- Recreational abusers of N2O report analgesia, depersonalization, derealization, and dizziness.[2]
- Chronic abuse of N2O can lead to numerous neurological effects including ataxia, polyneuropathy, and psychosis. The neurological effects are due to its inhibition of vitamin B12.[3]
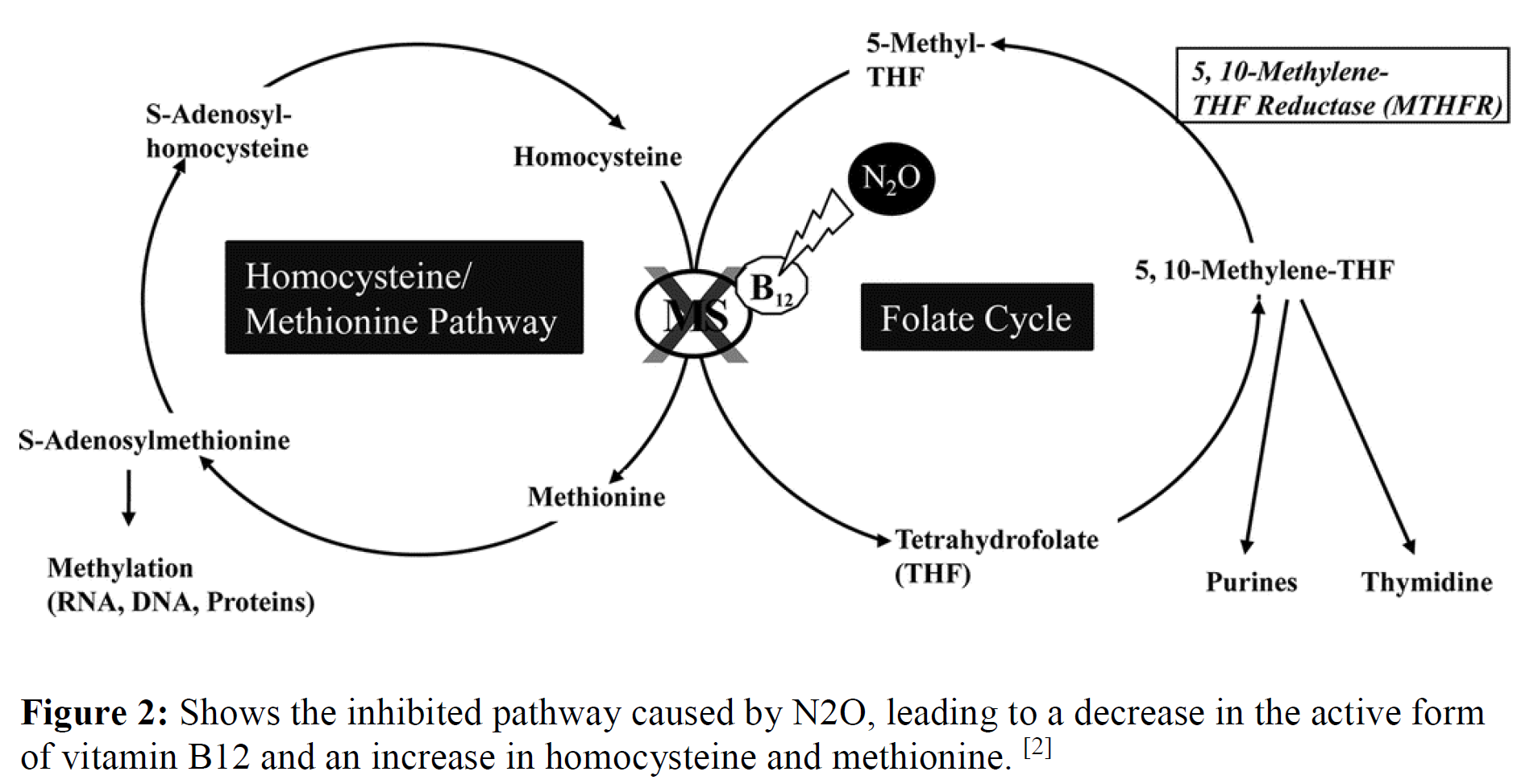
- Vitamin B12 is an important cofactor needed for methionine synthase. N2O converts vitamin B12 into its inactive form, via oxidation of its central cobalt ion. This leads to the irreversible inhibition of methionine synthase.
- Methionine synthase is a key enzyme in the production of DNA, RNA, and myelin. This eventually leads to demyelination in the central and peripheral nervous system.
- Chronic use of N2O can cause a syndrome identical to subacute combined degeneration of the spinal cord, which is described in patients with vitamin B12 deficiency. The classic clinical picture of pernicious anemia includes bone marrow depression and polyneuropathy (dorsal (posterior) and lateral spinal column demyelination).
When should the ED physician suspect nitrous oxide abuse?
- A physician should be suspicious of N2O abuse with a history of substance use along with key features seen in the physical exam such as ataxia, polyneuropathy, and psychosis.[4,5,6]
- Due to N2O’s short-acting effects, most people will present asymptomatically to the ED although some may have oral and/or nasal mucosal irritation, headache, chest discomfort, and sensation of chocking.[7]
- Rarely patients may be post-hypoxic and present with altered mental status, shortness of breath, cyanosis, tachycardia, and tachypnea.[7]
- Diagnosis can be supported with the presence of megaloblastic anemia, resulting from an inhibition of formation of activated vitamin B12, leading to a functional deficiency.[9]
- Labs will show normal levels of vitamin B12 with an elevation of homocysteine and/or methionine.[9]
- Although extremely rare, methemoglobinemia is another potential complication of inhaled N2O toxicity in patients with methemoglobin reductase deficiency and in N2O overdose.[8] However, this has only occurred in patients receiving N2O therapy for analgesia or treatment for pulmonary hypertension.[8]
- Deaths from N2O are extremely rare, but when they do occur, they almost always involve a bag over the head or opening a tank in a sealed space such as a car. In these situations, death occurs when N2O is at a high enough concentration to displace all oxygen.
What is the management?
- Prehospital management for inhalant abuse is supportive, such as maintenance of cardiorespiratory function and removal of the source toxin.
- For N2O-induced neurotoxicity, treatment is administration of high dose intramuscular B12 supplementation.[3]
- Regardless of supplementation, recovery of neuropathy may be slow and incomplete.
- Methionine may provide additional benefit, but the evidence is limited.
- Bone marrow findings revert with folinic acid.
References:
- Centers for Disease Control and Prevention. Nitrous Oxide. Available at: https://www.cdc.gov/niosh/topics/nitrousoxide/default.html
- Nagele P, et al. Influence of Methylenetetrahydrofolate Reductase Gene Polymorphisms on Homocysteine Concentrations after Nitrous Oxide Anesthesia. Anesthesiology 2008; 109(1): 36-43.
- Thompson AG, Leite MI, Lunn MP, Bennett DH. Whippits, Nitrous Oxide and the Dangers of Legal Highs. Pract Neurol. 2015 Jun; 15(3): 207–209.
- Iwata K, O’Keefe GB, Karanas A. Neurologic Problems Associated with Chronic Nitrous Oxide Abuse in a Non-Healthcare Worker. Am J Med Sci. 2001;322(3):173-4.
- Miller MA, Martinez V, Mccarthy R, and Patel MM. Nitrous Oxide “whippit” Abuse Presenting as Clinical B12 Deficiency and Ataxia. Am J Emerg Med 2004; 22(2): 124.
- Sethi NK., Mullin P, Torgovnick J, and Capasso G. Nitrous Oxide ‘Whippit’ Abuse Presenting with Cobalamin Responsive Psychosis. J Med Tox 2006; 2(2): 71-74.
- Dubrey S, Smith R. Whippits: Nitrous Oxide Gas Inhalation as Recreational Drug Use. Br J Hosp Med. 2016; 77(8): 492.
- Taylor MB, Christian KG, Patel N, Churchwell KB. Methemoglobinemia: Toxicity of inhaled nitric oxide therapy. Pediatr Crit Care Med. 2001; 2(1): 99–101.
- Garakani A, Jaffe RJ, Savla D, Welch AK, Protin CA, Bryson EO, Mcdowell DM. Neurologic, Psychiatric, and Other Medical Manifestations of Nitrous Oxide Abuse: A Systematic Review of the Case Literature. Am J on Add. 2016; 25(5): 358-69.








