Originally published on Ultrasound G.E.L. on 10/15/18 – Visit HERE to listen to accompanying PODCAST! Reposted with permission.
Follow Dr. Michael Prats, MD (@PratsEM), Dr. Creagh Bougler, MD (@CreaghB), and Dr. Jacob Avila, MD (@UltrasoundMD) from Ultrasound G.E.L. team!
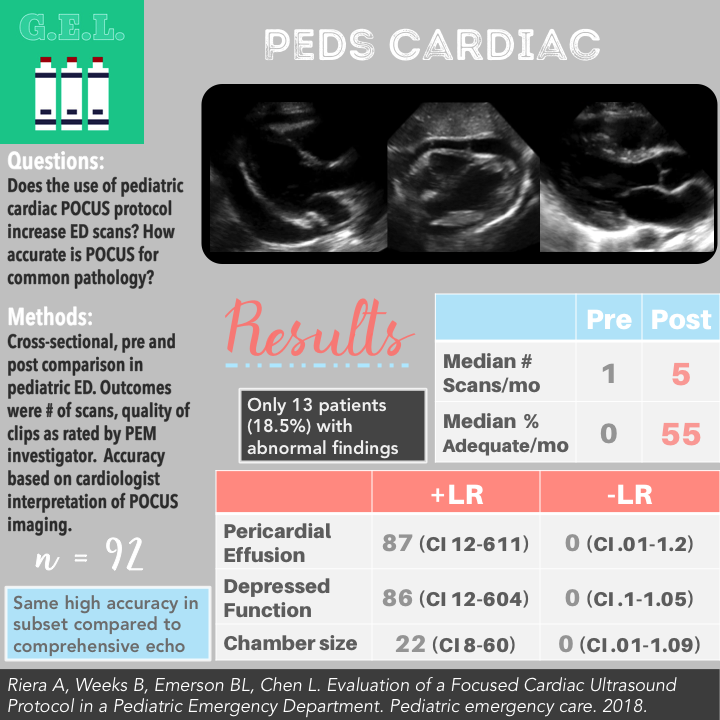
Evaluation of a Focused Cardiac Ultrasound Protocol in a Pediatric Emergency Department
Pediatric Emergency Care May 2018 (Epub) – Pubmed Link
Take Home Points
1. A pediatric cardiac POCUS protocol including significant collaboration with cardiology can increase the quantity and quality of POCUS performed.
2. Pediatric emergency physicians can accurately diagnose pericardial effusion, depressed function, and abnormal chamber size compared to cardiologist interpretation.
Background
The use of POCUS is rising in PEM
- 2013 Viera consensus educational guidelines for PEM fellows included focused cardiovascular applications
- 2015 Policy Statement on Point of Care Ultrasonography by Pediatric Emergency Physicians endorsed by American Academy of Pediatrics, highlighting the importance of using POCUS in PEM
However, minimal studies on using cardiac POCUS in PEDs. Some initial studies showing that PEM docs can recognize pericardial effusion and systolic dysfunction.
Recently more case reports demonstrating that POCUS will decrease the time to diagnosis and significantly alter management (we all have these stories…).
Questions
Does a focused cardiac ultrasound protocol increase the number of point of care ultrasound (POCUS) in a pediatric emergency department?
How does physician-sonographer performance measure against pediatric cardiologist interpretation of the video clips with regards to presence of pericardial effusion, qualitatively depressed LV function, and chamber size abnormalities?
Population
Academic tertiary care children’s hospital
Inclusion:
- Undifferentiated shock
- Cardiac arrest with return of spontaneous circulation
- Concern for pericardial effusion
- Concern for pulmonary embolus
- Unexplained dyspnea
- Exertional syncope
Design
Cross-sectional, observational, quality improvement project. Pre and post intervention comparison.
Convenience sample of PED patients up to 21 yo who received a Focused Cardiac UltraSound (FoCUS) exam at discretion of treating physician between January 2016 – December 2016
FoCUS protocol collaboratively designed between PEM and pediatric cardiology
Compared to focused cardiac scans done in the prior year (Jan 2015-Dec2015) prior to adoption of protocol/initiation of FoCUS QI project
FoCUS protocol: created by PEM POCUS director/PEM physician, reviewed by chief of cardiology.
Any abnormal finding on FOCUS triggered consultation with pediatric cardiology. Comprehensive ECHO performed at cardiologists discretion. If known cardiac patient, cardiology consulted prior to FoCUS.
Outcomes were differences between monthly median number of POCUS prior to implementation of protocol compared to after implementation. Also assessed accuracy of ED interpretation of FOCUS compared with cardiologist reviewing the FOCUS images. These PEM interpretation was also compared to comprehensive echo when performed.
Who did the ultrasounds?
34 Physicians including:
- PEM fellows
- PEM attendings
- Residents
No study-specific training. All had some training in the FoCUS exam. PEM attendings supervised trainees ultrasounds.
The Scan
Phased array transducer

Obtained these focused cardiac views:
- Parasternal Long Axis
- Parasternal Short Axis
- Apical Four Chamber
- Inferior vena Cava
No subcostal view!!
5 Minute Sono – Obtaining Cardiac Windows
5 Minute Sono – Pericardial Effusion
5 Minute Sono – Cardiac Function
Results
n = 92 exams performed
The Patients
Most Common FoCUS Indications:
- Concern for effusion 50%
- Dyspnea 23%
- Concern for pulmonary embolus 12%
- Shock 9%
*13% of patients had preexisting heart condition
Ages
- 0-2 months 3%
- 2-12 months 3%
- 1-3 years 7%
- 4-12 years 22%
- 13-21 years 65%
Pathology – 13 patients (18.5%) had abnormality
- 5 effusions, 6 depressed function, 6 chamber size abnormality, 2 with all three
Primary Outcome
Pre and Post Comparison in Quantity and Quality

Accuracy of PEM FoCUS Interpretation Compared to Cardiologist’s Interpretation of FoCUS Images

Other Findings
Accuracy of PEM FoCUS Interpretation Compared to Comprehensive Echo (n = 23)
Pericardial Effusion
Sens 100%
Spec 100%
Depressed Function
Sens 100%
Spec 100%
Abnormal Chamber Size
Sens 100%
Spec 95%
Adequacy of Individual Views
- PSLA 91%
- PSSA 87%
- A4C 60%
- IVC 83%
*Note that not all of these scans were done in each case
20% of clips were limited (meaning less than adequate)
Interrater reliability (for categorizing as limited or adequate) – K = 0.9
97% adherence to protocol (according to indications)
Findings documented before end of shift 92% of time
Limitations
Pre and post study. Always room for confounders. There are other things that could have lead to increase in POCUS and the increase in POCUS adequacy.
Comparison for accuracy was to an echo within 24 hours – could have changed some pathology. However, there was only 1 case of disagreement between FOCUS and comprehensive echo.
Unknown how many cases of attempted and aborted ultrasounds. This was not tracked and could provide an overestimation of the feasibility.
There was little pathology to draw conclusions from. The FoCUS appears accurate but small numbers. Sensitivity especially questionable given that there were few true positive exams. Also, 7 of 17 abnormal scans (counting some patients more than once for multiple pathologies) had pathology on prior echos – this could have biased physician sonographers. Also there were very few children <1 yo so validity is questionable in that population.
Discussion
Cardiologist was available for consultation (consulted in 52%) of cases. Cardiologist participated in training and review sessions. Having a cardiologist involved may be an integral part to success of a focused cardiac protocol. This may be problematic for centers where cardiologists are not supportive of POCUS. Some people may want to develop a POCUS program independent of cardiology. It would be difficult to create a program as described in this paper without the cooperation of cardiology.
No measure of impact on resource utilization. They did state that there was no measurable increased in annual echocardiograms, consultations, or admissions but data not provided. This is an important consideration for the implementation of a protocol. Before suggesting that this become adopted by other centers, it would be important to examine these types of outcomes.
Take Home Points
1. A pediatric cardiac POCUS protocol including significant collaboration with cardiology can increase the quantity and quality of POCUS performed.
2. Pediatric emergency physicians can accurately diagnose pericardial effusion, depressed function, and abnormal chamber size compared to cardiologist interpretation.
Our score