Ultrasound G.E.L. – The Venous Excess Ultrasound Grading System & Acute Kidney Injury
- Jan 28th, 2022
- Michael Prats
- categories:
Originally published on Ultrasound G.E.L. on 9/28/20 – Visit HERE to listen to accompanying PODCAST! Reposted with permission.
Follow Dr. Michael Prats, MD (@PratsEM) from Ultrasound G.E.L. team!
Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system
Ultrasound J April 2020 (Epub) – Pubmed Link
Take Home Points
1. This preliminary work presents the VExUS score as a POCUS measurement of venous congestion with potential correlation with acute kidney injury.
2. Much more research needs to be done including prospective studies with different populations and additional outcomes.
Background
Using point-of-care ultrasound to assist with management of hemodynamics is bread and butter critical care. However, most people are focusing on the cardiac function and an assessment of the preload. This paper brings up the fascinating point that we often neglect the effects that venous congestion can have on organ perfusion. They lay out many potential pathways that an increased venous pressure can be bad for organs. But is there a way to assess this?? Yes! At least there is now. Many POCUS users take a look at the IVC, but we can add to that the venous waveforms of abdominal organs. Although any one of these items can fail you, perhaps putting them all together is the way to go. This is the first published article on the VExUS (Venous Excess UltraSound) grading system which suggests a protocol for assessing and grading the amount of venous congestion in your patients.
Questions
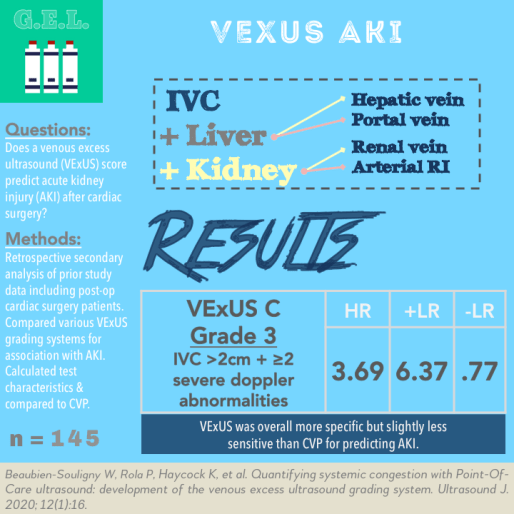
Does the VExUS score have clinical value in predicting the occurrence of acute kidney injury after cardiac surgery?
How does the VExUS compare to central venous pressure (CVP)?
Population
Inclusion:
- ≥18 years old
- Undergoing cardiac surgery with the use of cardiopulmonary bypass
Exclusion:
- Severe chronic kidney disease (GFR <15 mL/min or dialysis)
- Renal transplant
- Critical preoperative state (aborted sudden death, preoperative cardiac massage, preoperative mechanical ventilation, preoperative vasopressor/inopressor support, intraaortic balloon pump before surgery)
- AKI before surgery
- Delirium before surgery
- Known conditions that would interfere with doppler of portal system (cirrhosis, thrombosis)
Design
Post-hoc analysis of data from a prior study assessing portal flow pulsatility on post-operative cardiac surgery patients
In the prior study, they randomly screened patients the day before surgery, recruited a number of patients per day based on availability of investigators.
POCUS assessment was performed the day before surgery, at ICU admission after surgery, and daily on post-op days 1-3.
They also collected information from pre or intraop TEE, CVP from jugular central venous catheter. Labs such as NT-pro-BNP, creatinine were collected.
Acute kidney injury (AKI) defined as increased in serum creatinine > 26 umol/L within 48 hours or 50% from baseline within a week from cardiac surgery.
Clinical information such as vasopressors, inotropes were collected to calculate a vasopressor-inotrope score (VIS) that reflects an overall requirement even with different or multiple medications.
This prior article goes into these with some good figures. All of this stuff was previously published. What this article did was create a grading system putting them all together. This team included intensivists, emergency physicians, a nephrologist, and anesthesiologist.
They made 5 prototype grading systems – VExUS A, B, C, D, E, each with variations of what was considered Grade 0, 1, 2, 3
Spoiler! C was the best, it looked like this:
Normal: IVC < 2 cm
Grade 1: IVC ≥ 2 cm + normal or mild abnormalities in dopplers
Grade 2: IVC > 2 cm + Severe abnormalities in ≥1 pattern
Grade 3: IVC > 2 cm + Severe abnormalities in ≥2 patterns
They expressed the association between VExUS grades and new AKI with a hazard ratio
They first wanted to find which of their prototype grading systems was most associated with AKI, then they performed a multivariate regression.
They also calculated test characteristics and compared VExUS to different CVP cut-offs.
Who did the ultrasounds?
Two investigators trained in hepatic and renal doppler
The Scan
Curvilinear transducer

Dorsal decubitus position with head of bed at 0º or 30º. Avoid valsalva maneuver.
Probe is in mid to posterior axillary position on right side
IVC in this article it was from subxiphoid, in the original article (from which these patients were originally enrolled, it seemed to indicate the right mid-axillary line for this view as well). The maximal diameter of IVC was measured (at intrahepatic portion, 2 cm from junction of hepatic veins)
Portal vein Doppler normally should have very little pulsatility. In this study they calculated the pulsatility fraction, which is the difference in the max and min velocities divided by the max, as a percentage.
Hepatic Vein Doppler normally should have a systolic wave equal or greater than diastolic wave. In abnormal hepatic venous flow, the diastolic is larger or there is reversal of flow in systole
Intrarenal doppler pulsed wave doppler at corticomedullary junction in all three segments, during a respiratory pause after expiration. Normally there is continuous venous flow. Abnormal would be biphasic venous flow or worse – only flow during diastole. They recorded the pattern over 2 to 3 cardiac cycles. Also calculated renal arterial resistive index.
Learn how to do VEXuS from Western Sono
Results
N = 145
- Median age 66
- 21.4% had known heart failure
- 25.5% had chronic kidney disease
- 33.8% of patient had AKI after surgery
Primary Outcome – Comparison of the Different VExUS scores (A-E)
VExUS C grading system Grade 3 (severe congestion) was most strongly associated with AKI, HR 3.69 (CI 1.65-8.24)
In multivariable model remained associated after adjusting for baseline risk and other factors – HR 2.82 (CI 1.21-6.60)
VExUS C Grade 2 also associated with AKI HR 2.65 (CI 1.07-6.60)
Overall, requiring too many “severe” abnormalities led to less Grade 3 patients. Including the IVC also led to less patients with Grade 3. Grade 3 in all prototypes was associated with AKI.
Additional Findings
Test Characteristics for VExUS at ICU Admission for AKI
VExUS C Grade 3 – this one was the most specific
Specificity 96% (89-99%), +LR 6.37 (2.19-18.5)
Sensitivity 27% (15-41%), -LR 0.77 (0.65-0.91)
Best sensitivity was from most of the protocols Grade 1 – 73%
CVP was at best 77% sensitive (CVP ≥8 mmHG), and 83% specific (CVP ≥ 12 mmHg)
The cumulative fluid balance did not exactly line up with the VExUS grades. There was overlap between normal and Grades 1-3 but it looked like grade 1 was highest, then grade 3, then normal, then grade 2 had lowest (Figure 4c).
IVC dilation alone was only 41% specific for AKI.
Strengths
Introduces a novel scoring system and uses robust analysis to determine the best prototype for grading
Appropriate comparisons to CVP and serum values
Clinical relevance with outcome of acute kidney injury
Limitations
This is a derivation study where the primary purpose is determining which form of the VExUS criteria is most accurate. Therefore, we can’t draw conclusions from this data that the VExUS should be used in clinical practice.
Retrospective analysis. Only cardiac surgery patients who were not critically ill-preoperatively. It is highly likely that some of the pathophysiology changes in other populations. The spectrum of patients seen in cardiac surgery is not representative of many other populations where people may want to use VEXUS.
This is a complex skill. This study used well-trained operators. How long does this take to learn? How long does this exam take to complete? Prior studies have shown feasibility and good interrater reliability (per these authors), but we might need more of those in different settings and different populations.
AKI may not be the best marker of overall venous congestion. The authors even mention in their discussion that venous congestion will not be a factor in many cases of AKI. Unfortunately, this is the whole crux of this study. If AKI is not always related to venous congestion (which we know it is not), then having the VExUS associated with AKI, does not necessarily mean that the VExUS is associated with venous congestion. Of course – based on our understanding of pathophysiology, it certainly makes sense, but I suppose it could be measuring something different that also happens to predict AKI.
Unclear if treating physicians were blinded to POCUS results. What if certain physicians acted on them, but others did not? That could have skewed main end-point of AKI.
There is a lot of data in here. They measured each of 5 different prototypes, on 5 different days, at 4 different grades and then looked to see what stuck. This was perhaps a necessary approach this early in investigations, but ultimately we need to figure out when and how to assess this and THEN figure out the strength of that approach.
Discussion
This is great preliminary work for scouting out the VExUS score. As mentioned above, it is a derivation study. Therefore we need a prospective validation cohort to see if this association with AKI continues. However, this study does give us a solid starting point for future work. I would like to see a study that compares using the VExUS score to guide fluid management to using IVC, CVP, or even a unqualified “traditional management”. End points should focus on patient centered outcomes – days in ICU, need for diuresis, even mortality (and sure- AKI also).
The authors bring up the idea of adding RV function to the assessment. Others have suggested diastolic measures of the left heart. You could also consider looking at the lungs for fluid overload. The possibilities are endless. Did we really exhaust our other options before turning to more complicated abdominal doppler measurements? I haven’t seen many studies suggesting that echo and lung alone are inadequate. I think that this is a fascinating discussion, but I would like to see more comparisons between this and simpler options.
Summary
This was a retrospective study that looked at the use of a novel VExUS score, a POCUS measure of venous congestion incorporating abdominal organ doppler measurements. In a population of post cardiac surgery patients, they compared different iterations of the VExUS grading system for outcomes of acute kidney injury. They found that at best the VExUS had a hazard ratio of 3.69 and was specific, although not sensitive for AKI. This seemed to be better than CVP.
Take Home Points
1. This preliminary work presents the VExUS score as a POCUS measurement of venous congestion with potential correlation with acute kidney injury.
2. Much more research needs to be done including prospective studies with different populations and additional outcomes.
More Great FOAMed on this Topic
Western Sono – Solid Organ Doppler Assessment of Venous Congestion
Thinking Critical Care VExUS Mini-Tutorial
EMCrit VExuS score with Phillipe Rola
ACEP News – Venous Doppler and IV Fluid Administration
POCUS 101 – VEXUS Ultrasound Score
Critical Care Northampton – VEXUS Score
Our score

Expert Reviewer for this Post

Nik Theyyunni, MD @Heydrnik
Nik Theyyunni is the ultrasound director at the University of Michigan, Department of Emergency Medicine.
Reviewer’s Comments
This study is an interesting post-hoc analysis to determine which of several prototype VexUS grading systems best predicts AKI in a derivation cohort of post cardiac patients. While it has significant limitations, it’s a great example of how we can approach research into the nuances of holistic evaluations of patients using POCUS in a rigorous way. It’s important to note that this is essentially a derivation study. I would want to see this VExUS prototype grading system validated with a future cohort of patients to see that this relationship bears out. It would also be great to see future studies looking at this grading system in differing patient populations –for example, the physiology of AKI in sepsis is different from post-cardiac surgery patients, and it’s not clear that the same grading system would work well in both populations!
Cite this post as
Michael Prats. VExUS – Venous Congestion and Acute Kidney Injury. Ultrasound G.E.L. Podcast Blog. Published on September 28, 2020. Accessed on January 28, 2022. Available at https://www.ultrasoundgel.org/99.