Written by: Jonathan Warren, MD (@jonthewookie – EM Resident, Department of Emergency Medicine – Harbor-UCLA Medical Center) and Manpreet Singh, MD (@MPrizzleER – Assistant Professor in Emergency Medicine / Department of Emergency Medicine – Harbor-UCLA Medical Center) // Edited by: Stephen Alerhand, MD (@SAlerhand, Assistant Professor of Emergency Medicine, Rutgers New Jersey Medical School)
Case #1:
A 28 year-old male presents to the emergency department (ED) after a bicycle accident where he fell onto his right side after hitting a speed bump. He is unable to touch his left shoulder with his right arm and has numbness around his deltoid. You suspect an anterior shoulder dislocation and confirm the diagnosis with x-rays. After what you suspect is a successful reduction, you wonder if there is a quicker way to confirm relocation than waiting for another x-ray.
Case #2:
A 40-year-old male presents to the ED with severe left-sided shoulder pain that has been worsening for the past two weeks. He has recently been going to the gym in an attempt to lose weight for his hypertension and has had worsening pain with shoulder press. On exam, he has painful range of motion, particularly with abduction, and has a positive Hawkin’s Test. You wonder if there is a way to expedite this patient’s care instead of referring him to his primary care physician PCP for a magnetic resonance imaging scan.
Point-of-care ultrasound (POCUS) for the shoulder can be utilized within the ED setting to decrease wait times and expedite diagnosis and disposition of patients.1 With sensitivities and specificity of 100% for dislocation and sensitivity and specificity of 100% and 97% for tendon pathology, shoulder POCUS may quickly provide diagnosis for a range of pathologies.2,3
Background Anatomy
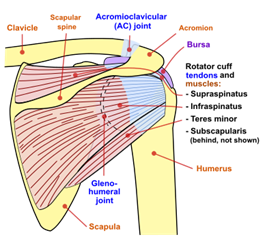
Anterior and posterior representations of the shoulder joint
(Photo Courtesy of Wikicommons (https://commons.wikimedia.org/wiki/File:Shoulder_joint.svg)
The shoulder is a ball-in-socket joint comprised of an articulation between the glenoid of the scapula and the head of the humerus. The glenoid fossa is a shallow socket joint and reinforced by a ring of thickened fibrocartilage known as the labrum. The joint is encircled by the rotator cuff, a structure comprised of the tendons from four muscles: supraspinatus, infraspinatus, teres major, and subscapularis.
The subscapularis attaches to the lesser tuberosity, while the additional three rotator cuff muscles attach to the greater tuberosity. Between the supraspinatus and subscapularis insertions sits the long head of the bicep tendon, near the rotator cuff interval (a free space between the tendons of the subscapularis and supraspinatus). Located around the joint are several bursae with the most prominent, the subacromial bursa, found below the deltoid and extending anteriorly over the rotator cuff. Finally, the acromioclavicular (AC) joint is located superior to the glenohumeral joint.
POCUS Shoulder Examination4,5
The POCUS shoulder examination consists of five primary views, evaluated in the long- and short-axis planes and with dynamic movement of the tendon in question. The examination is completed utilizing the linear probe, except where noted below.
Long Head of the Bicep
- Position: Seated, hand resting on thigh, palm facing up with probe placed along anterior glenoid.
- Landmarks: Glenoid sulcus
- Dynamic Evaluation: Active flexion/extension of the elbow
Found within the bicipital groove, the long head of the bicep tendon (LHBT) is a hyperechoic, oval-shaped structure within the sulcus of the glenoid. Translate the probe along the tendon from insertion to muscle belly to rule out any partial tears, which may appear as hypoechoic lesions, within the tendon. In the long-axis view, applying distal pressure below the probe may help straighten the tendon for optimal visualization. Note that the LHBT is in communication with the glenohumeral joint and a small amount of fluid within the structure is considered normal.


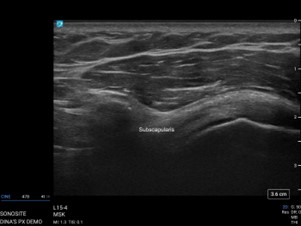
Subscapularis
- Position: Seated, arm externally rotated with elbow held against body wall. Place the probe along anterior shoulder and superior to humerus
- Landmarks: Lesser tuberosity
- Dynamic Evaluation: External/internal rotation of forearm
The length of the tendon should be evaluated in the short-axis until its insertion into the lesser tuberosity is visualized. You may visualize the muscle and tendon fibers intermixed, and any suspected abnormalities should then be visualized in two planes.
Supraspinatus
- Position: Patient in Crass or modified Crass with the probe placed anteriorly on the humeral head
- Landmarks: Greater tuberosity, acromion
- Dynamic Evaluation: Passive abduction of the arm
The Crass position has the patient assume a stance where the dorsal aspect of their hand is placed along the lumbar spine.6 However, as patients with shoulder pathology are often in significant pain, you may direct them to assume the modified Crass position: placing their hand on their ipsilateral back as if they were grabbing something from the rear pocket. Ensure that their elbow remains in the sagittal plane for optimal visualization. From the long-axis view, translating the probe medially may help evaluate the LHBT, rotator cuff interval, and subscapularis tendon as well. Dynamic evaluation should assess for the tendon smoothly diving below the acromion.


Infraspinatus and Teres Major
- Position: The patient in a seated position with hand resting on thigh, palm facing up. Place the probe posteriorly and inferior to the scapular spine.
- Landmarks: Humeral head, labrum
- Dynamic Evaluation: Passive internal/external rotation of arm
In the long-axis, the probe may be translated medially to evaluate the labrum for injury and the posterior recess for joint effusions.


From this viewpoint, you may also capture both the humeral head and the glenoid within one image to assess for dislocation or confirm reduction. If distal visualization is required, consider having the patient cross their arm across the chest to bring structures into view or utilizing the curvilinear probe.

Acromioclavicular Joint
- Position: The patient seated, hand resting on thigh with the probe placed coronally over the shoulder and in line with the clavicle.
- Landmarks: Acromion, Clavicle
- Evaluation:
- Normal joint space: ≤ 5 mm
- Dynamic: Movement of hand to touch contralateral shoulder

Pitfalls
- Anisotropy, an area within the tendon appearing hypoechoic due to an insonating beam that is not perpendicular with the tendon, is the primary pitfall in shoulder ultrasound.7 This may be confused for partial/full thickness tear and interpreted as a false positive and thus all abnormalities should be evaluated in two planes.
- Body habitus represents another pitfall, where one may not acquire adequate visualization of the bony structures of the glenohumeral joint from the posterior approach with the linear probe. In these cases, the curvilinear probe should be used.
- One additional pitfall is linear echoes that may be present within the bicipital groove after LHBT rupture that appear similar to intact fibers. Careful visualization and medial translation should be completed to evaluate for a dislocated tendon.7
Pathology
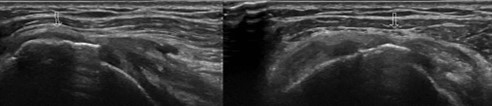
Dislocation
The most common use of the POCUS shoulder evaluation in the emergency department is to diagnose dislocation and to confirm reduction. A recent meta-analysis has found that POCUS exam for dislocation is 100% sensitive and specific with an LR+ of 11,254.8 and LR- of <0.1.2 It is an easily employed technique by both novice and experienced sonographers alike.8 Moreover, fractures associated with the dislocation were identified with a sensitivity of 96.8% and specificity of 99.7% by identifying cortical disruption on ultrasound.2
Dislocation Evaluation:
- Position: Patient seated with the hand resting on their thigh with the palm up. Place your probe posteriorly, inferior to the scapular spine
- Using the curvilinear probe may allow for increased depth.
- Landmarks: Humeral head, glenoid
- Evaluation: Use landmarks of the humeral head and the glenoid when evaluating for dislocation, and increased space between the two indicates dislocation.
Note that within the joint space there may be heterogenous echotexture, which may represent hemorrhage. A similar view can be acquired during or post-reduction to ensure that the humeral head has returned to the glenoid fossa, preventing repeated radiation exposure.9
Anterior Shoulder Joint Dislocation: From the posterior approach, a humeral head that is distal to the typical glenoid articulation as pictured here is consistent with an anterior dislocation, if appearing more proximal, this is consistent with a posterior dislocation.

Ultrasound may also be utilized to diagnose AC joint dislocation defined by an increased space between the cortical borders of the acromion and clavicle exceeding 2-3 mm compared to the contralateral side. The joint space should also further widen during dynamic evaluation. However, at this time, ultrasound has not been shown to correlate with Rockwood’s criteria or exclude fractures and x-ray is still required.10
Rotator Cuff Pathology
Diagnosing rotator cuff pathology is another common use of POCUS evaluation. Successfully diagnosed rotator cuff tears via ultrasound has the potential to reduce patient waiting times and allow for expedited referral and management.11
A note on diagnosing tears:
- Look for hypoechoic fluid and edema within the tendon sheath
- Thickness: Diagnosed in the short axis
- Partial-thickness – Does not involve entire cross-sectional area
- Full thickness – Involves entire cross-sectional area
- Length: Diagnosed in long axis
- Small: < 1 cm
- Large: 1-3 cm
- Massive: > 3 cm
Ultrasound may diagnose full-thickness tendon injuries with a sensitivity of 100% and specificity of 97% when performed by expert ultrasonographers.3 Subsequent studies have identified a similar sensitivity and specificity for partial-thickness tears.12 Tears should be described based on their location, shape, with a massive tear described as 5cm or greater.13

It is also possible to identify calcific tendonitis, generally located at the enthesis of the tendons with well-defined hyperechoic structure with posterior acoustic shadowing. When identified, the provider is able to expedite referral and management for these patients.14 Ultrasound is able to detect calcifications within the tendon with a sensitivity of 79% and specificity of 88%.3
Finally, during dynamic evaluation of the supraspinatus, a physician may be able to detect subacromial impingement evidenced by bunching of the supraspinatus tendon below the acromion. Physicians can detect this with sensitivity of 81% and specificity of 95%.15
Long Head Biceps Tendon Pathology
Tears within the LHBT appear similar to those of the rotator cuff tendons. Full-thickness tears or tendon rupture may also present with two floating heads when visualized in long-axis. Tendon dislocation may present with an empty sulcus and medially displaced tendon. Partial-thickness tears and tenosynovitis of this tendon both present with hypo- or anechoic thickened tissue within the tendon. Note that this may be a difficult diagnosis as the tendon is consistent with the glenohumeral joint and may have some slight fluid present at baseline.
Conclusion:
POCUS of the shoulder is a useful skill within the ultrasound toolbelt and aids in diagnosis of shoulder dislocation and guides reduction. It may diagnose tendon tear or rupture with similar accuracy to MRI and expedite patient disposition and management.
Case #1:
Using your knowledge of shoulder POCUS, you scan his shoulder and confirm the location of the humeral head in the glenoid fossa. He is placed in a sling and referred to orthopedics for follow-up.
Case #2:
You use ultrasound to diagnose a partial supraspinatus tear in this patient. You recommend rest, NSAIDs, ice, and coordinate a referral to his primary care provider for both physical therapy and orthopedics follow-up.
References:
- Secko MA, Reardon L, Gottlieb M, Morley EJ, Lohse MR, Thode HC Jr, Singer AJ. Musculoskeletal Ultrasonography to Diagnose Dislocated Shoulders: A Prospective Cohort. Ann Emerg Med. 2020 Aug;76(2):119-128. doi: 10.1016/j.annemergmed.2020.01.008.
- Gottlieb M, Patel D, Marks A, Peksa GD. Ultrasound for the diagnosis of shoulder dislocation and reduction: A systematic review and meta-analysis. Acad Emerg Med. 2022 Jan 30. doi: 10.1111/acem.14454. Epub ahead of print. PMID: 35094451.
- Read JW, Perko M. Shoulder ultrasound: diagnostic accuracy for impingement syndrome, rotator cuff tear, and biceps tendon pathology. Journal of Shoulder and Elbow Surgery 1998;7(3):264-71.
- Gupta H, Robinson P. Normal shoulder ultrasound: anatomy and technique. Seminars in musculoskeletal radiology 2015;19(3):203-11. doi: 10.1055/s-0035-1549315 [published Online First: 2015/05/30]
- Petranova T, Vlad V, Porta F, et al. Ultrasound of the shoulder. Medical ultrasonography 2012;14(2):133-40. [published Online First: 2012/06/08]
- Crass JR, Craig EV, Thompson RC, et al. Ultrasonography of the rotator cuff: surgical correlation. Journal of clinical ultrasound : JCU 1984;12(8):487-91. doi: 10.1002/jcu.1870120806 [published Online First: 1984/10/01]
- Jamadar DA, Robertson BL, Jacobson JA, et al. Musculoskeletal sonography: important imaging pitfalls. American Journal of Roentgenology 2010;194(1):216-25.
- Lahham S, Becker B, Chiem A, et al. Pilot Study to Determine Accuracy of Posterior Approach Ultrasound for Shoulder Dislocation by Novice Sonographers. The western journal of emergency medicine 2016;17(3):377-82. doi: 10.5811/westjem.2016.2.29290 [published Online First: 2016/06/23]
- Halberg MJ, Sweeney TW, Owens WB. Bedside ultrasound for verification of shoulder reduction. Am J Emerg Med 2009;27(1):134.e5-34.e6. doi: 10.1016/j.ajem.2008.05.023 [published Online First: 2008/12/02]
- Pogorzelski J, Beitzel K, Ranuccio F, et al. The acutely injured acromioclavicular joint – which imaging modalities should be used for accurate diagnosis? A systematic review. BMC Musculoskelet Disord2017;18(1):515-15. doi: 10.1186/s12891-017-1864-y
- Chiu CH, Chen P, Chen AC, Hsu KY, Chang SS, Chan YS, Chen YJ. Shoulder ultrasonography performed by orthopedic surgeons increases efficiency in diagnosis of rotator cuff tears. J Orthop Surg Res. 2017 Apr 20;12(1):63. doi: 10.1186/s13018-017-0565-4.
- Roy JS, Braen C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. British journal of sports medicine 2015;49(20):1316-28. doi: 10.1136/bjsports-2014-094148 [published Online First: 2015/02/14]
- Serpi, F., Albano, D., Rapisarda, S., Chianca, V., Sconfienza, L. M., & Messina, C. (2021). Shoulder ultrasound: current concepts and future perspectives. Journal of ultrasonography, 21(85), e154–e161. https://doi.org/10.15557/JoU.2021.0025
- Riley DC, Kaufman M, Ward TM, et al. Emergency department diagnosis of supraspinatus tendon calcification and shoulder impingement syndrome using bedside ultrasonography. Critical ultrasound journal 2013;5(1):2. doi: 10.1186/2036-7902-5-2 [published Online First: 2013/02/13]
- Farin PU, Jaroma H, Harju A, et al. Shoulder impingement syndrome: sonographic evaluation. Radiology1990;176(3):845-49.