Author: Zackary Salem-Bango (EM Resident Physician, University of Washington) and Jonathan Warren, MD (Clinical Ultrasound and EMS Fellow, Harbor-UCLA Medical Center) // Reviewed By: Steve Field, DO; Brit Long, MD (@long_brit)
Case
A 27-year-old male with no significant past medical history presents with new onset right upper extremity heaviness and swelling 8 hours after an upper extremity weightlifting session. He takes workout supplements and ibuprofen as needed, denies any anabolic steroid use or hormone use, any recent trauma to the extremity, history of blood clots in himself or his family, or recent skin changes or infections. He has not had any recent surgical procedures; however, he does report a recent trip to a commercial health spa and had a peripheral IV placed in his right arm for vitamins and a normal saline bolus. He denies regular drinking, drug use, or cigarette smoking.
Triage VS: BP 124/65, HR 95, T 98.5 Oral, RR 15, SpO2 97% on RA.
Introduction
Indications
Upper extremity deep vein thrombosis (UEDVT), while less common than lower extremity DVTs, is an important clinical entity to diagnose especially for admitted patients with peripherally inserted central catheters (PICCs) or central venous catheters (CVC). UEDVT comprises about 5-10% of DVT cases identified annually.1 Complications related to UEDVTs include pulmonary embolism, superior vena cava syndrome, and rarely infection.
UEDVTs can be generally separated into two categories:
- Primary UEDVT
- Classically effort induced in young athletes
- Known at Paget-Schroetter Syndrome, and is a venous form of thoracic outlet syndrome2
- MUCH less common than secondary
- Subclavian vein involvement most common2
- Secondary UEDVT
- Classically catheter affiliated (CVC, PICC, power port, pacemaker wires, etc.)
- Risk Factors: cancer, surgery, trauma, acquired thrombophilia, immobilization, pregnancy, oral contraceptive use and ovarian hyperstimulation syndrome3
Classic presentations of UEDVT:
- Heaviness
- Discomfort
- Pain
- Paresthesia
- Swelling
- Pitting Edema
- Redness
- Cyanosis
- Visible collateral veins
- Fever
Can evaluate with Constan’s Score4
| Item | Points | |
| Venous material (catheter/access device) present | +1 | |
| Localized pain | +1 | |
| Unilateral pitting edema of the extremity | +1 | |
| Other diagnosis at least as likely | -1 | |
| Classification | Prevalence of UEDVT | |
| Low clinical probability | 0 | 12% |
| Intermediate clinical probability | 1 | 20% |
| High clinical probability | >2 | 70% |
Diagnosis of UE Ultrasound:
Contrast venography remains the gold standard for diagnosing UEDVT, however ultrasonography provides an acceptable method of screening for patients where UEDVT is being considered for diagnosis based on history and physical exam.
Performance of UE Ultrasound:
- Sensitivity ~97%
- Specificity ~96%
- Limited by sample size5
- No studies specifically in POCUS
- Requires experienced scanner.
- If high clinical suspicion yet negative US, consider contrast venography or MR evaluation as there are central veins that may be difficult to visualize in some patients.
Relevant Anatomy:
Classically, UEDVT can present in various branches of the venous system as it leads to the central venous system and eventually the superior vena cava. UEDVT screening typically involves the following vasculature proceeding from proximal to distal: Internal jugular vein → Subclavian vein → Axillary Vein → Brachial/basilic veins.6
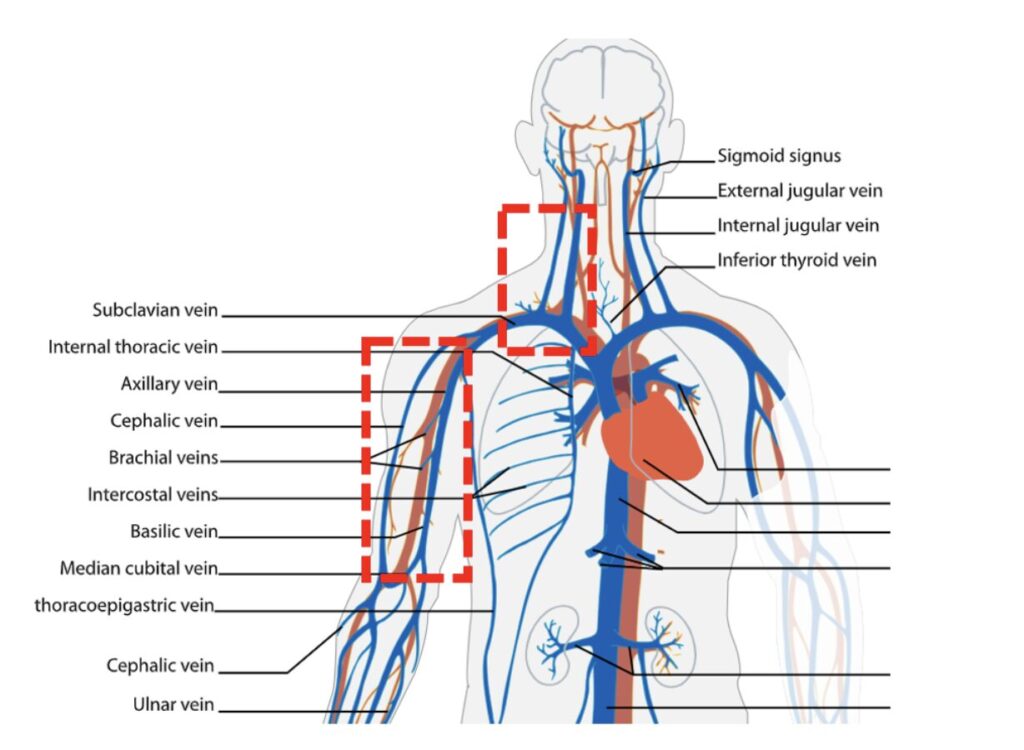
Anatomy Image 1: Relevant Anatomy for UEDVT (Image courtesy of Wikimedia)7
Scanning Technique:
Positioning and Preparation:
Sit the patient in a supine position with the arm abducted between 60 and 90 degrees into a position of comfort for the patient. The head should be rotated to the contralateral side and you may consider placing the gurney in slight Trendelenburg (which will help to engorge the upper extremity veins). Attempt to avoid hyperextension that may result in abnormal flow. For this scan, it is recommended to use a linear probe as this will provide the highest resolution for imaging vessels. In patients with larger body habitus or in areas with increased tissue such as when imaging the axillary vein, you may consider using a curvilinear probe.
Normal Findings:
For venous structures that are compressible, one should expect the lumen of the vein of interest to completely compress before deformation of the artery occurs. If compression is not possible due to anatomy, utilize color flow (see Image 2 for normal finding) or pulsed wave doppler to evaluate for flow. Increased color flow should also be seen with distal compression of the extremity, causing proximal flow augmentation. Normal flow patterns vary between individuals (as a result of depth, respiration, right heart function) and should be compared to the contralateral side if pathology is suspected. Note that color doppler may be optimized by ensuring the angle of insonation to the skin is 60 degrees or less. This can be either physical (fanning the probe) or mechanical (device correction of insonation). Overall, compression testing has a higher sensitivity than flow doppler, but the former test may be limited by anatomy5.
Internal Jugular Vein
Scan at the proximal/lateral junction of the neck and shoulder and identify the Internal Jugular Vein (IJ). The operator should then either perform a compression test or apply flow doppler across this vessel. Ideally, all vessels should be imaged in two planes.

Anatomy Image 2: Internal Jugular Vein7

Ultrasound Image 1: Left Image: A photo of the internal jugular vein (marked with *) imaged on top of the carotid artery. Right Image: This image is the same anatomy with compression demonstrating a normal exam
Junction of Subclavian and IJ
Continue scanning down to the supraclavicular region and attempt to identify the confluence of the IJ and subclavian vein. An infraclavicular approach may also be necessary depending on patient positioning and habitus. If you are having difficulty visualizing this confluence, you may try a phased array probe, which due to its smaller footprint may help to visualize the vessel around the clavicle. You may also attempt to visualize the vessels by scanning proximally in the supraclavicular region until you reach the clavicle under your probe inferiorly and then fanning the probe with the tail of the probe moving cephalad to work around the clavicle. Compression will not be possible with this view, so color doppler and pulsed wave doppler should be used to assess for thrombosis. Track along the subclavian to assess for filling defects. If you are unable to visualize any portion of a vein, you should ensure you perform distal pulsed wave doppler and proximal flow augmentation which if abnormal for either may suggest a clot within the non-visualized portion of vein. Proximal flow augmentation is the practice of compressing distal to the point of ultrasound. Typically there should be a sharp spike in color flow or doppler signal. A muted or absent increase in flow is concerning for the presence of a clot between the site of compression and the probe.
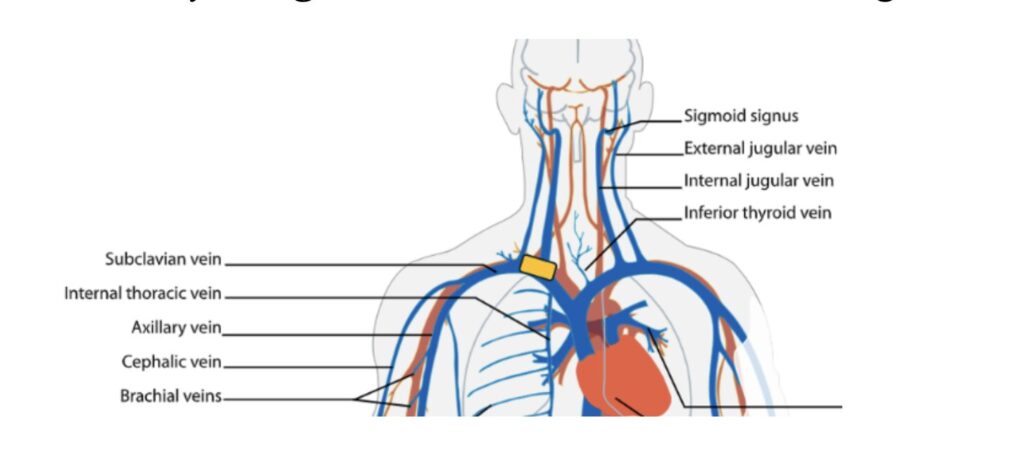
Anatomy Image 3: Subclavian and Internal Jugular Vein7

Ultrasound image 2: Left image: Demonstrating the confluence of the internal jugular (IJ) and the Subclavian Vein. Right Image: Color doppler across these respective structures with respiratory variation.
Axillary Vein
In order to obtain the next view, place the patient in a recumbent position with the respective hand placed behind their head. As you trace the subclavian laterally into the axilla, one should be able to obtain a cross-section of the axillary vein and perform a compression test. The operator can also place color flow across this structure if compression is inhibited by anatomy or habitus. Evaluation at this site may require a curvilinear probe for some patients.

Anatomy Image 4: Axillary vein7

Ultrasound Image 3: Left Image: Prior to compression, the operator should visualize the axillary vein as a large superficial vessel. Right Image: Demonstrates normal compression.
Tracking down Brachial/Basilic Veins with interval compression
Identify the Basilic/Brachial Vein and track these structures down to the antecubital fossa, providing interval compression every 1-2 cm. The basilic vein is typically superficial in comparison to the brachial vein and the latter typically courses alongside the brachial artery. Additionally, the basilic vein will be medially oriented when the patient is in the anatomic position. It should be noted that the basilic vein is technically a superficial vein and thrombosis of this vessel would be considered superficial vein thrombosis. However, if associated with a line or extensive in nature may still require anticoagulation or removal of the line. Identifying this vessel is helpful in ensuring that it is not confused for the brachial vein.

Anatomy Image 5: Brachial and Basilic Veins7

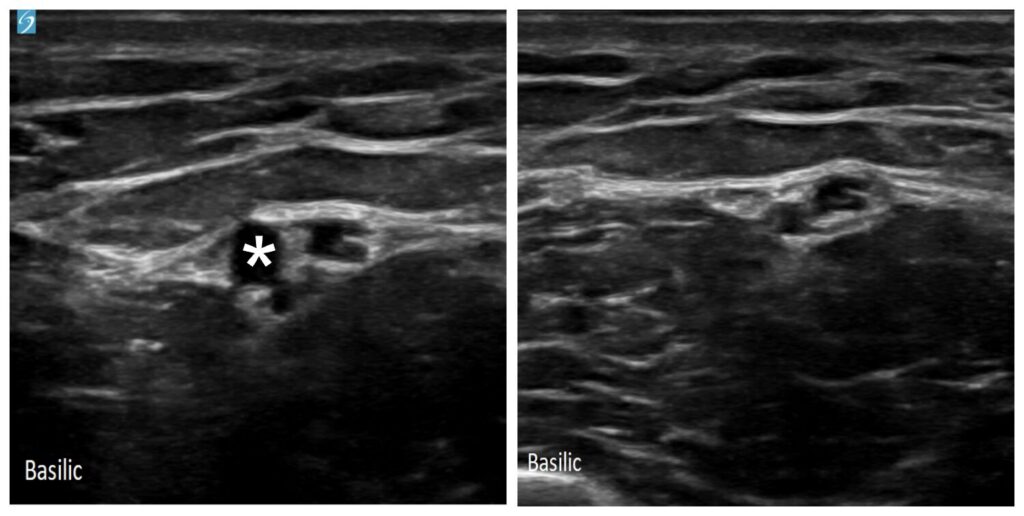
Ultrasound image 4: Left Image: Interval compression of the brachial vein. Middle Image: * indicates the basilic vein with the basilic artery deep to this structure. Right Image: Normal compression of the basilic vein.
Radial and Ulnar Veins
Similar to the brachial and basilic veins, identify the radial and ulnar veins (they will run with their respective arteries). If identifying these is difficult, one can also start distally from the wrist and track backwards toward the antecubital fossa. Complete interval compression every 1-2 cm.
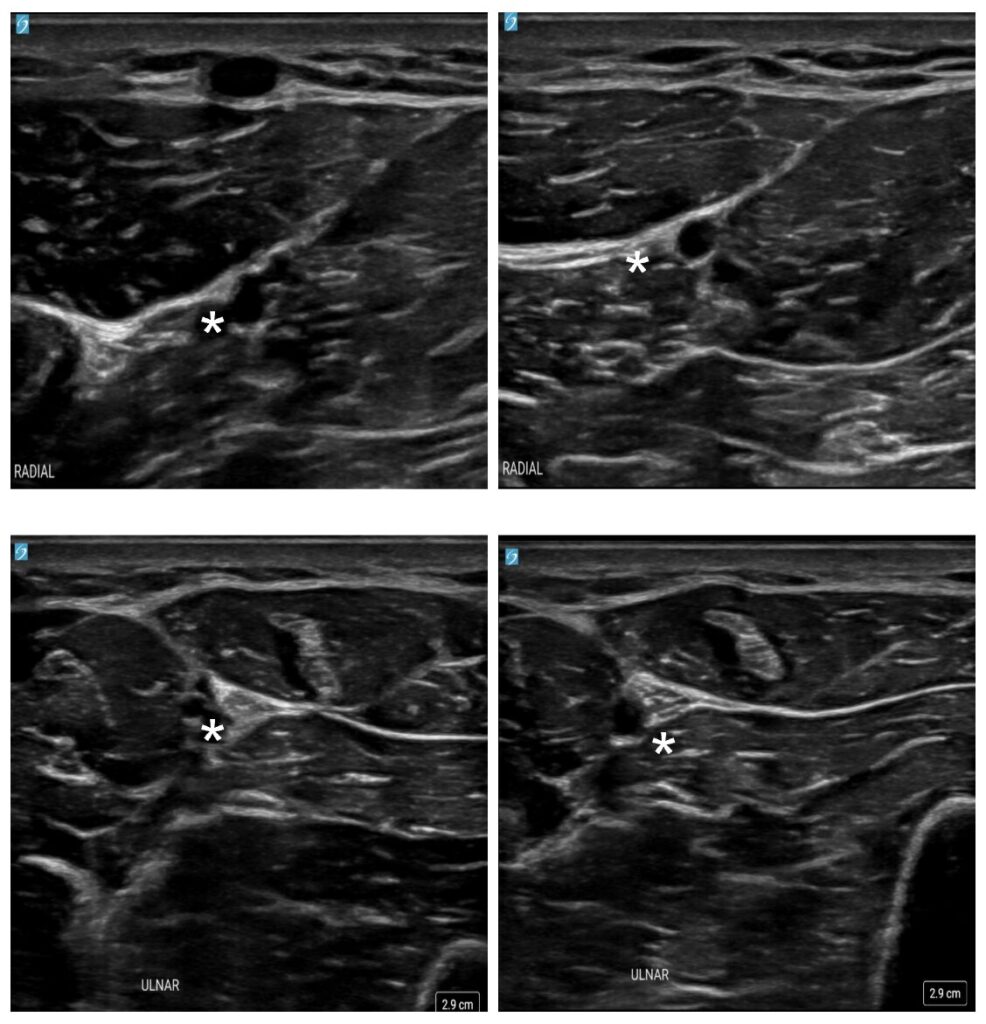
Ultrasound Image 5: Upper Left: * indicates the small radial vein. Upper Right: Normal findings with compression of the radial vein. Lower Left: * indicates the small ulnar vein. Lower Right: Normal findings with compression of the ulnar vein.
Pathology:
A DVT can be diagnosed when there is lack of compressibility in any of the structures undergoing evaluation. More specifically, if you are pressing with enough perpendicular force to indent a portion of the artery, you should be able to visualize complete venous collapse. If not, this is concerning for the presence of a DVT and the most sensitive sign on ultrasound.
You may also visualize a heterogeneous echogenicity within the lumen that corresponds to the clot. Utilizing color doppler, there will be a flow deficit within the vessel. You may supplement this with pulsed-wave doppler where with distal compression of muscles, a flow pattern will be absent. This dampening is suggestive of central thrombosis or compression of the vein due to stenosis or other structure. If present, it is important to compare these findings to the contralateral side. Below are a few examples of UEDVTs.
Similar techniques can be used to diagnose chronic UEDVT, however, this becomes significantly more complex and is beyond the scope of this article.

Ultrasound Image 6: Internal Jugular Thrombus (Sourced from The POCUS Atlas8): Large intramural thrombus located within the internal jugular vein. Lesion is multilayered with concentric hyperechoic regions interspersed with more hypoechoic ones.
Ultrasound Image 7: Basilic Vein Thrombus (Sourced from The POCUS Atlas8): Note the hyperechoic density within the lumen of this vessel. One can see surrounding structures compressing as the operator checks for a DVT but vessel lumen does not compress.
Pearls/Pitfalls:
-Be sure to adjust depth to visualize vessels properly. A good rule of thumb is that the structures of interest should fall within the middle of the operator’s screen.
-POCUS ideally should be used to rule in UEDVT. Other methods, such as comprehensive radiology performed US studies or venography can be utilized for definitive rule out.
-If there is uncertainty regarding color/doppler flow, augmentation, or compressibility of a vessel during your scan, it should be compared to the same region on the unaffected limb.
-Be careful to track along venous structures to ensure they’re actually veins! Lymph nodes can sometimes look like a non-compressible vessel but can easily be identified by scanning more distally/proximally where one would expect the vessel to course or by identifying the tree-like vascular flow within them.
-Check out https://www.emdocs.net/us-probe-pearls-and-pitfalls-for-point-of-care-ultrasound-evaluation-of-deep-vein-thrombosis/ and https://www.emdocs.net/em3am-dvt/ for more information on lower extremity DVT POCUS, workup, and treatment
Case Resolution:
POCUS reveals a thrombus within the subclavian vein as it transitions to the axillary vein at the intercostal margin. This finding is consistent with Paget-Schroetter syndrome, a form of venous thoracic outlet syndrome. The patient is placed on anticoagulation and ultimately returns home. Unfortunately, they re-present several other times with similar findings eventually requiring a first rib resection for prevention of future episodes.
References
- Muñoz, F. J. et al. Clinical outcome of patients with upper-extremity deep vein thrombosis: results from the RIETE Registry. Chest 133, 143–148 (2008).
- Engelberger, R. P. & Kucher, N. Management of Deep Vein Thrombosis of the Upper Extremity. Circulation 126, 768–773 (2012).
- Lokich, J. J. & Becker, B. Subclavian vein thrombosis in patients treated with infusion chemotherapy for advanced malignancy. Cancer 52, 1586–1589 (1983).
- Upper Limb Thrombosis: Constans Clinical Decision Score. https://practical-haemostasis.com/Clinical%20Prediction%20Scores/Formulae%20code%20and%20formulae/Formulae/Upper-limb-thromboses/Constans_score.html.
- Di nisio, M. et al. Accuracy of diagnostic tests for clinically suspected upper extremity deep vein thrombosis: a systematic review. Journal of Thrombosis and Haemostasis 8, 684–692 (2010).
- Deep Vein Thrombosis (DVT). https://www.acep.org/sonoguide/basic/dvt.
- Villarreal, L., Mariana Ruiz. English: Simplified Diagram of the Human Venous System in Anterior View. (2009). https://commons.wikimedia.org/wiki/File:Venous_system_en.svg
- Vascular. TPA https://www.thepocusatlas.com/dvt.






