Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. This week the series covers prehospital transfusion of plasma.

Author: Christiaan van Nispen, MD (Emergency Medicine Physician Resident, San Antonio, TX) and Brannon Inman (Chief Resident, Emergency Medicine Physician, San Antonio, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Prehospital Plasma during Air Medical Transport in Trauma Patients at Risk for Hemorrhagic Shock
AKA: The “PAMPer” Study
Clinical question:
In patients at risk for hemorrhagic shock, is there a mortality benefit to pre-hospital transfusion of plasma as the initial resuscitation fluid compared to the standard of care?
Study design:
- Multi-centered, cluster-randomization trial
PICO:
Population:
- Inclusion:
- Patients being transported by one of 27 participating air transportation teams from the scene of blunt or penetrating injury or from a referring ED to one of 9 participating trauma centers
- At risk for hemorrhagic shock during transport or prior to arrival of transport team, defined as at least one episode of either:
- Systolic blood pressure < 90 mm Hg AND heart rate > 108 beats per minute
- Systolic blood pressure < 70 mm Hg irrespective of heart rate
- Assumed consent for participation in trial unless patient or family voiced opposition; patients could opt out of continued participation later
- Exclusion:
- Younger than 18 years or older than 90 years
- Inability to establish intravenous and/or intraosseous access
- Isolated fall from standing mechanism of injury
- Isolated drowning mechanism of injury
- Isolated hanging mechanism of injury
- Presence of greater than 20% total body surface area burns
- Traumatic cardiac arrest lasting longer than 5 minutes
- Penetrating brain injury
- Incarcerated patients
- Pregnant patients
Intervention:
- Infusion of 2 units of universal donor or group A low titer B (<1:100) thawed plasma to patients at risk for hemorrhagic shock in addition to standard of care
- Plasma was the initial resuscitative fluid prior to advancing to the erstwhile standard of care for fluid resuscitation.
Comparator:
- Standard of care only with a goal of systolic blood pressure ≥ 90 mm Hg
- Standard of care varied by air transportation team.
- 13 of 27 air transportation teams also carried 2 units of universal donor packed red blood cells (pRBCs) which could be infused after a liter of crystalloid if one of the following conditions were present:
- Systolic blood pressure < 90 mm Hg
- Heart rate > 120 beats per minute
- Deteriorating mental status
- Capillary refill > 2 seconds
- Remainder of teams used isotonic crystalloid infusion only.
- 13 of 27 air transportation teams also carried 2 units of universal donor packed red blood cells (pRBCs) which could be infused after a liter of crystalloid if one of the following conditions were present:
Enrollment and Randomization:
- Initially calculated that 530 screened prehospital patients would lead to 504 eligible patients, which would provide 88% power to detect a 14% difference.
- 2 years, 8 months into the trial, enrollment was increased to 564 to account for higher-than-expected ineligible patients.
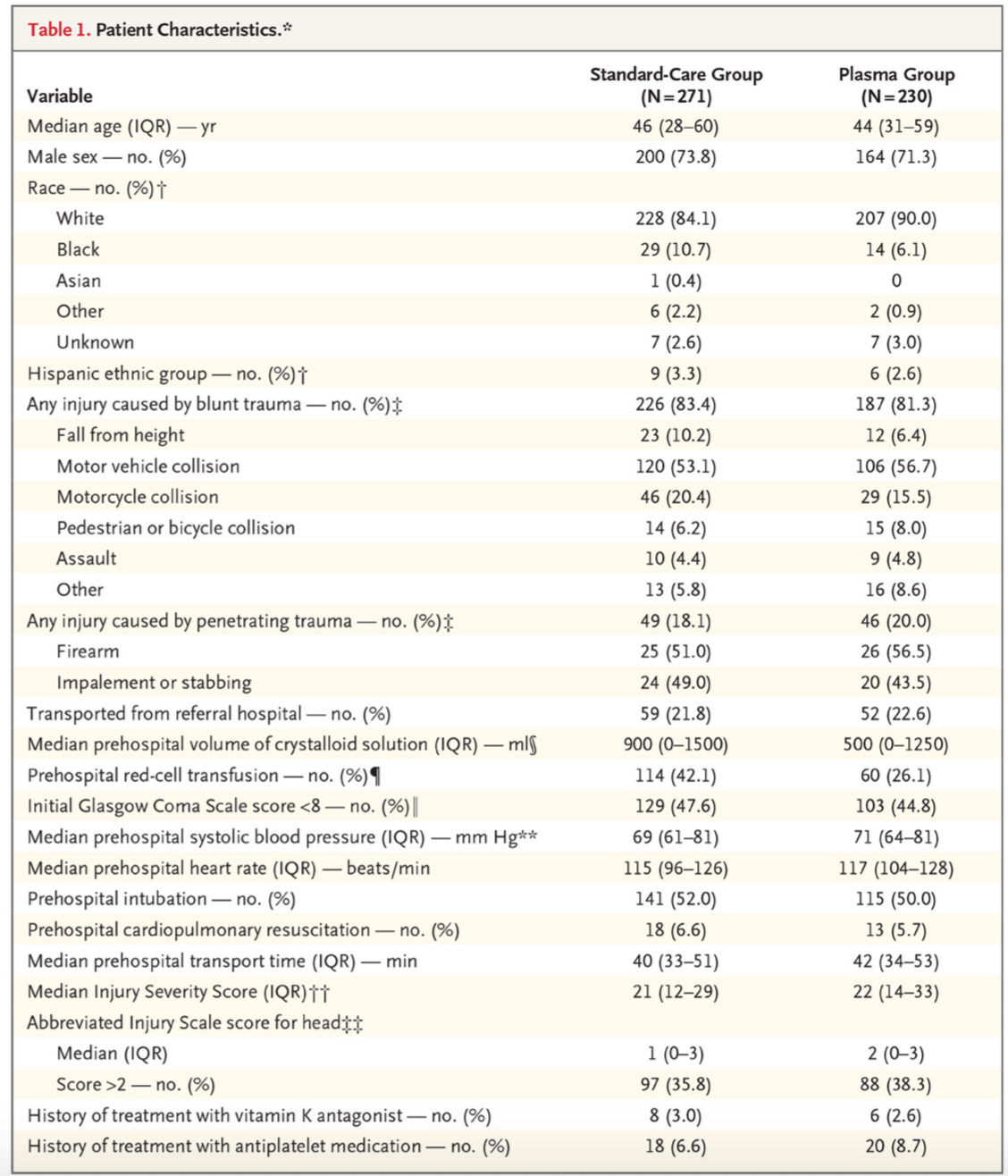
- Intervention and Comparator arms were demographically well balanced.
- Enrolled patients were largely men (72.7%), sustained injuries from blunt trauma (82.4%), and appeared at high risk for severe outcomes, given the median prehospital heart rates, systolic blood pressures, and rates of intubation reported.
- 390 enrolled at scene; 111 enrolled from referring ED.
- Due to limited shelf life of thawed plasma, randomization was clustered by air medical team base.
- Each month, each base was randomized to carry or not to carry plasma in addition to their standard of care.
- Primary outcome data was available for 96% of patients.
Outcome:
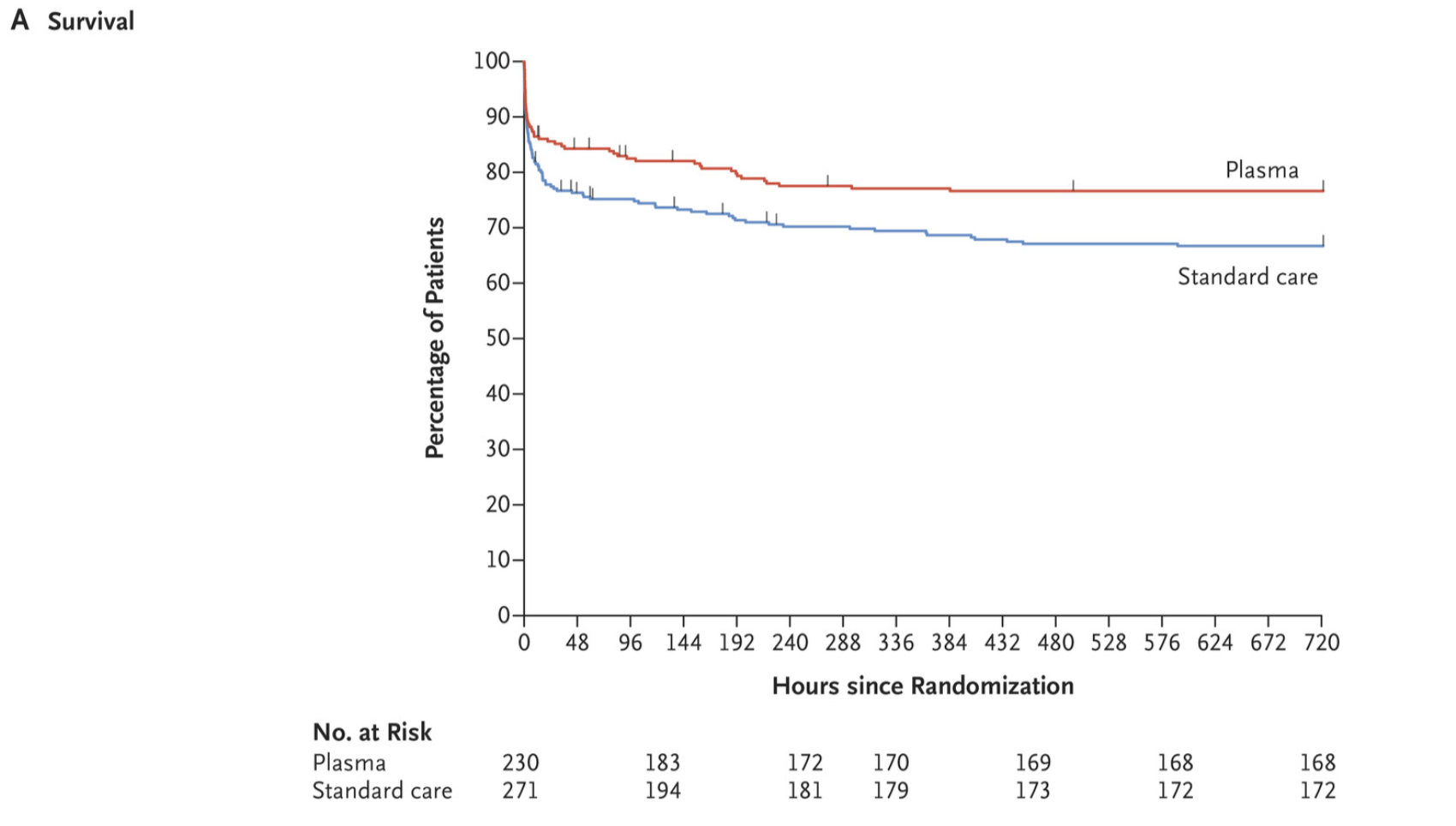
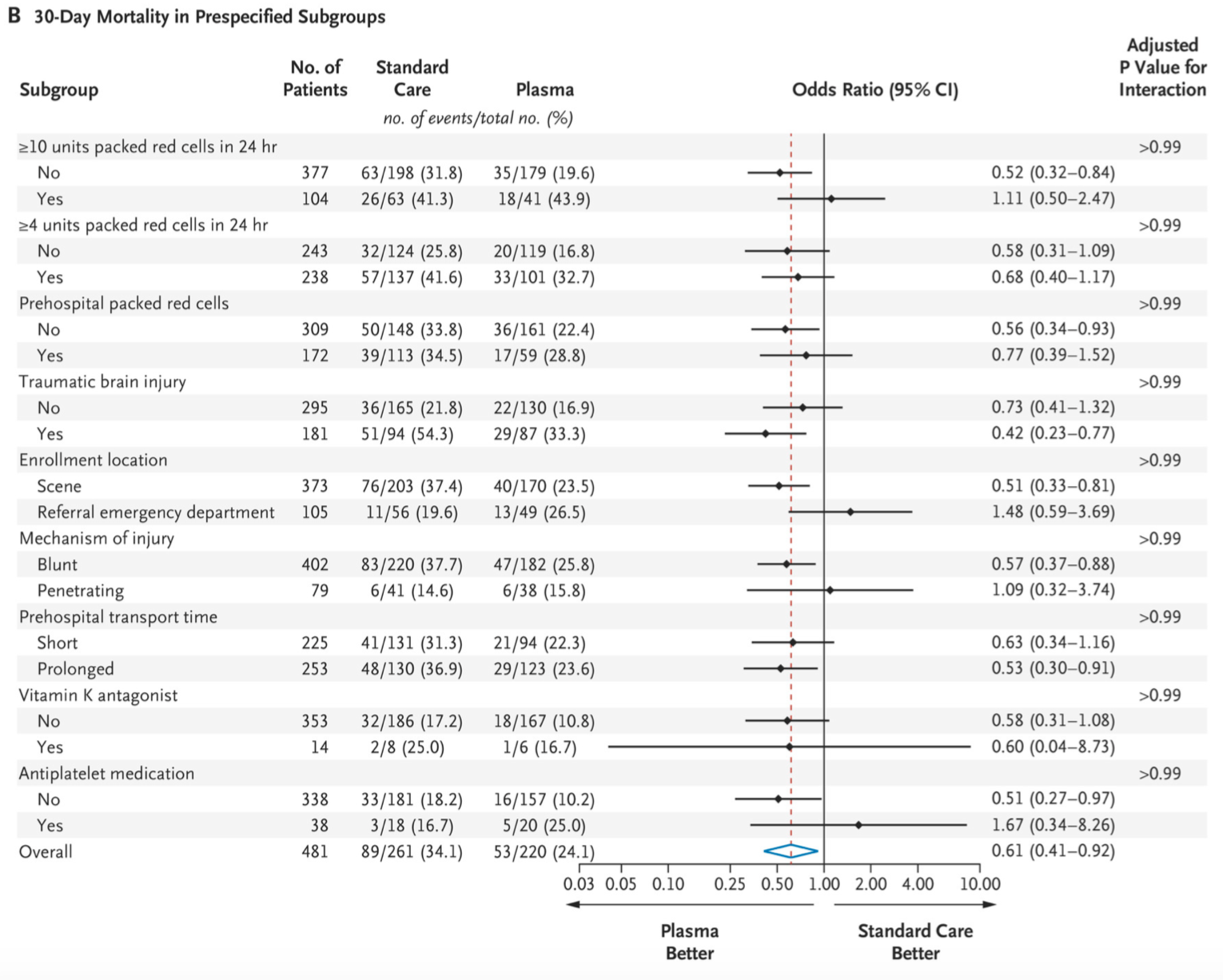
- Statistically significant difference in primary outcome of 30-day mortality
- 53 deaths in the plasma group
- 89 deaths in standard of care group
- 2% vs. 33.0%; difference, −9.8 percentage points; 95% confidence interval, −18.6 to −1.0%; P=0.03
- There remained a 39% lower risk of death at 30 days in the plasma group when accounting for variations in pre-hospital crystalloid volume infused, pre-hospital pRBC volume infused, and clustering at the base level
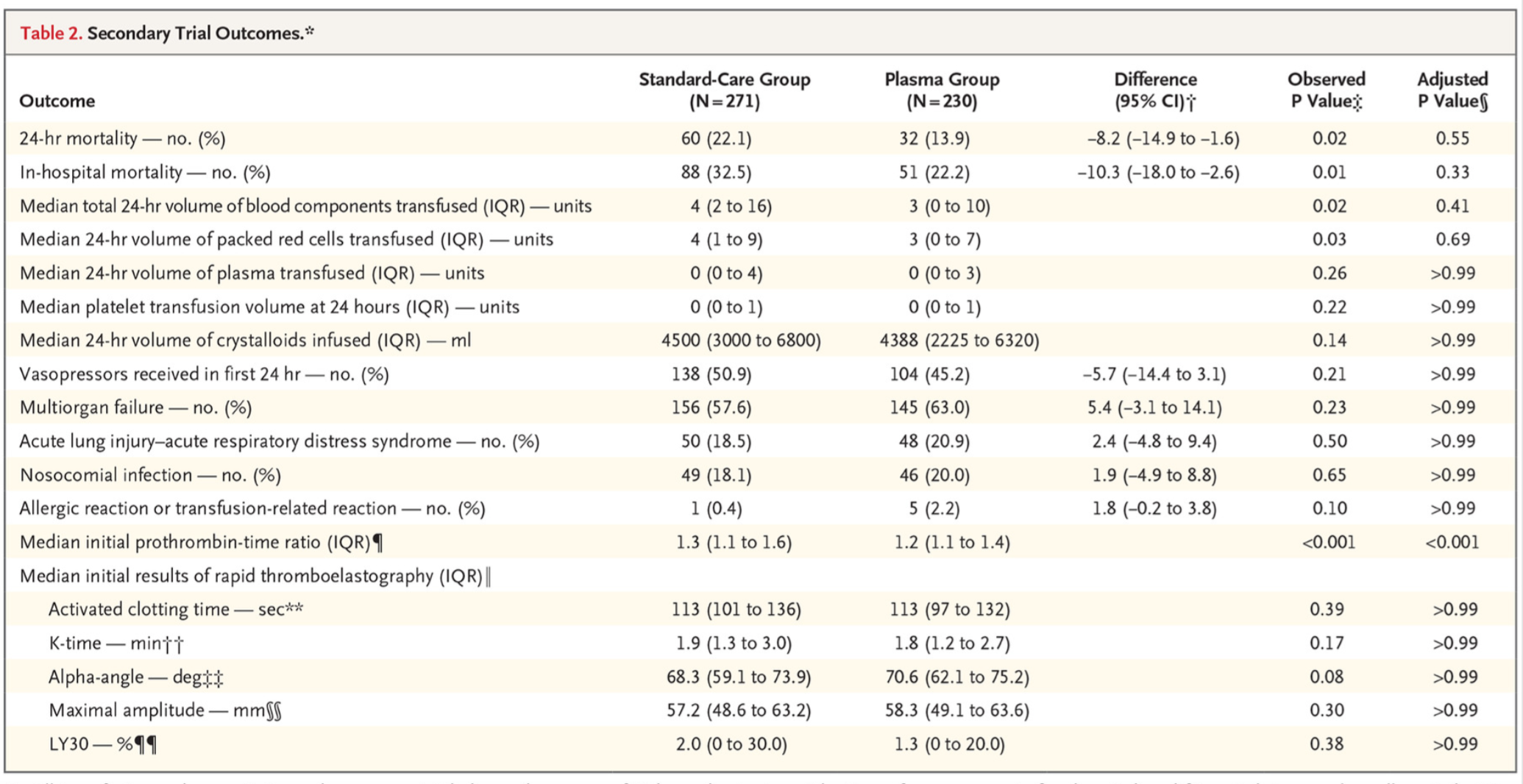
- Statistically significant difference in initial prothrombin time, which was a secondary outcome
- 1.2 in plasma group
- 1.3 in control group
- Other secondary outcomes lacked statistical significance:
- 24-hour mortality
- In-hospital mortality
- Onset of acute lung injury/acute respiratory distress syndrome
- Onset of multi-organ failure
- Median total 24-hour volume of pRBCs transfusion
- Median 24-hour volume of plasma transfusion
- Median 24-hour volume of platelet transfusion
- Vasopressor requirement in first 24 hours
- Onset of nosocomial infection
- Allergic reaction or transfusion related reaction
- Median initial results of thromboelastography
Take aways:
- Positive trial: pre-hospital plasma appears superior to standard of care alone.
- Intervention group was less likely to be administered prehospital pRBCs (26.1% vs. 42.1%) and received lower median crystalloid volume (500mL vs. 900mL) yet had better 30-day mortality outcomes.
- Effect was larger in the patients transported from scene compared to patients transported from a referring ED, suggesting that earlier plasma transfusion might be better, though more research is necessary for validation.
- Though statistically significant, it is unlikely that the 0.1 difference in initial prothrombin time is physiologically or clinically meaningful enough to account for the apparent mortality benefit.
- The study is appropriately powered and has limited loss to follow-up.
My take:
- In patients with pre-hospital signs of hemorrhagic shock, pre-hospital plasma transfusion in conjunction with pRBCs and/or crystalloid appears superior to pRBCs and/or crystalloid alone, which tracks with other recent data demonstrating that balanced transfusion and the avoidance of crystalloid are best practices.
- More research is needed to validate the results of this trial, with better standardized local protocols regarding the transfusion of other blood products and crystalloid.
References:
- Sperry JL, Guyette FX, Brown JB, et al. Prehospital Plasma during Air Medical Transport in Trauma Patients at Risk for Hemorrhagic Shock. N Engl J Med.2018; 379(18):1783. DOI 10.1056/NEJMc1811315








