Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. This week the series covers cricoid pressure in non-fasting patients during RSI.

Author: Brannon Inman (Chief Resident, Emergency Medicine Physician, San Antonio, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Effect of Cricoid Pressure Compared With a Sham Procedure in the Rapid Sequence Induction of Anesthesia
Clinical question:
In non-fasting patients undergoing RSI, does cricoid pressure prevent aspiration?
Study design:
- Randomized, double blind, single center, non-inferiority trial
PICO:
Population:
- Inclusion:
- Included “non-fasting” adults (had eaten in last 6 hours) undergoing general surgery eligible for RSI
- Had to have one of the following risk factors for aspiration:
- Emergent condition/emergent surgery
- Obesity (BMI > 30)
- Prior gastric surgery
- A known ileus
- Immediately postpartum
- Gastroparesis
- Gastroesophageal reflux
- Hiatal hernia
- Preoperative nausea/vomiting or pain
- Had to have one of the following risk factors for aspiration:
- Included “non-fasting” adults (had eaten in last 6 hours) undergoing general surgery eligible for RSI
- Exclusion:
- Pregnancy
- Contraindication to cricoid pressure (C spine trauma, laryngeal trauma, foreign body in trachea or esophagus)
- Contraindication to use of succinylcholine
- Pneumonia
- Pulmonary contusions
- Respiratory tract abnormalities
- Patients requiring alternative technique to laryngoscopy
Methods:
- Patients were randomized continuously 1:1 to the cricoid pressure and the sham cricoid pressure group (noninferiority margin 1.5)

- Patients were followed up to 28 days or hospital discharge, whichever was shorter.
- Anesthesia was induced with a rapid acting sedative (choice of sedative was up to the anesthesiologist)
- Etomidate
- Propofol
- Thiopental
- Ketamine
- All were paralyzed with succinylcholine; rocuronium was not allowed
- Intubating conditions were standardized following French guidelines.
- Aspiration was detected visually at the glottis during laryngoscopy, or by tracheal aspiration immediately following intubation
Intervention:
- Cricoid Pressure
Comparison:
- Sham procedure/Sham cricoid pressure
Outcome:
- Primary outcome:
- 6% incidence of aspiration with cricoid pressure
- 5% incidence of aspiration with sham
- Relative risk 0.90 (95% CI 0.33-2.38)

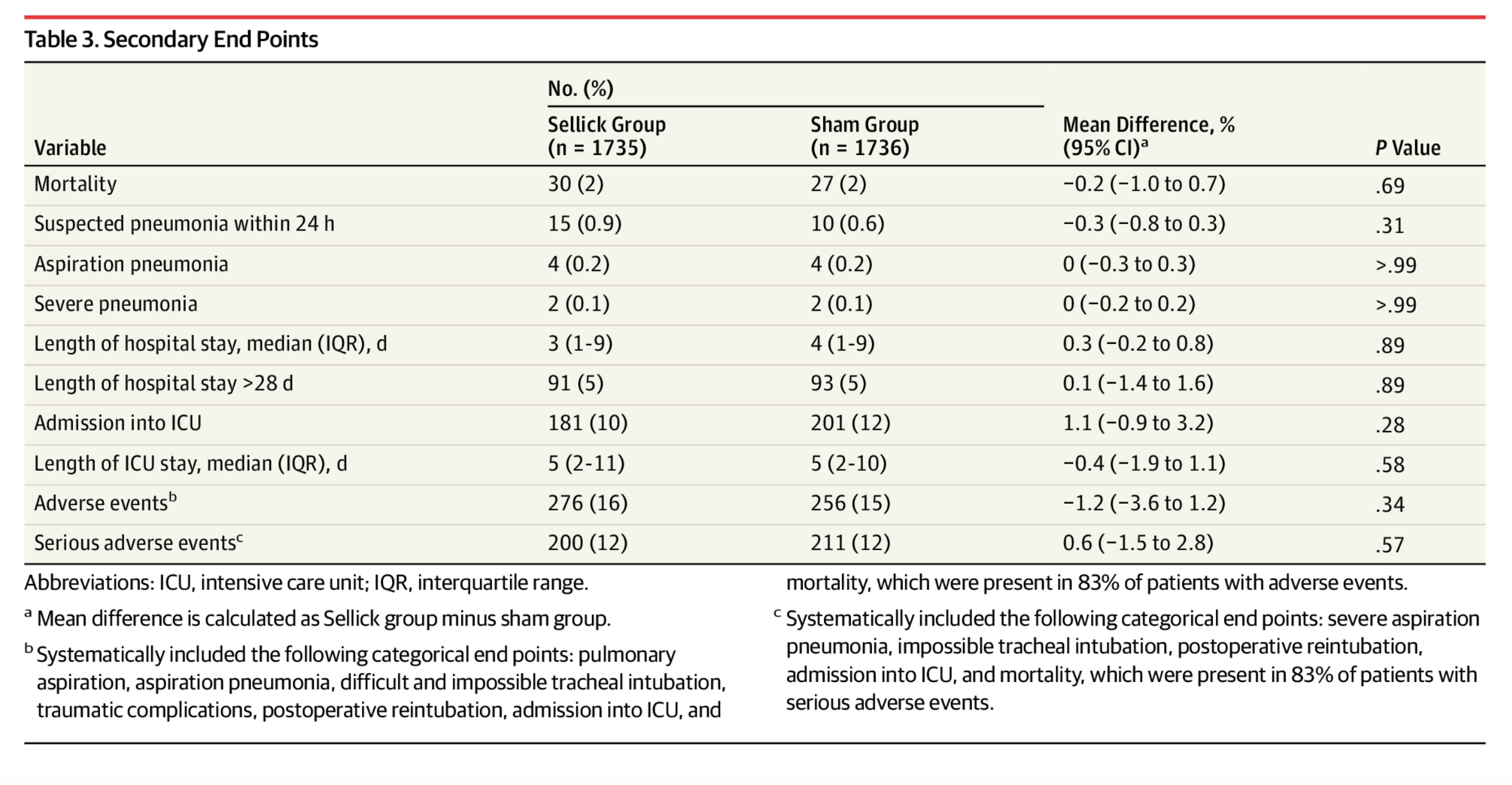
- Secondary outcome
- No statistically significant difference in secondary outcomes
Take Aways:
- Sham procedure not non-inferior to cricoid pressure
- To me, this is an odd set up design. A more interesting question would be “is cricoid pressure superior to nothing” using a superiority design. The study is set up so that sham has to prove it is non-inferior, in effect setting cricoid pressure as the standard. Likely there was a failure to show non-inferiority as the primary event (aspiration) was rare, as evidenced by large confidence intervals.
- Excluded pregnant women and children, two populations that in my experience have a tendency to vomit. This limits the external validity of the study.
- This was conducted in France, with adherence to “French guidelines,” which do not appear to be clearly outlined in the text or supplemental text. My assumption is that these guidelines would be similar to American guidelines. However, the patient population and guidelines utilized may also limit the application of the study to American patients.
- The study utilized patients undergoing surgery with the general anesthesia. It’s not immediately clear to me, whether or not these data are applicable to patients in the ED.
My take:
- This showed that sham-cricoid pressure was not non-inferior to cricoid pressure. However, there are issues with the study design, and concerns about external validity and application to a patient population I serve. In the face of lacking evidence to the contrary, I will continue not using cricoid pressure as a standard practice during emergent endotracheal intubation in the ED.
Source Article:
- Birenbaum A, Hajage D, Roche S, et al. Effect of Cricoid Pressure Compared With a Sham Procedure in the Rapid Sequence Induction of Anesthesia: The IRIS Randomized Clinical Trial [published correction appears in JAMA Surg. 2019 Jan 1;154(1):96]. JAMA Surg. 2019;154(1):9-17. doi:10.1001/jamasurg.2018.3577








