Authors: Brit Long, MD (@long_brit, EM attending physician, San Antonio, TX), Amber Cibrario, DO (@amcibrario, EM attending physician, San Antonio, TX), Zac Baker, DO (@zac_baker1, Greater San Antonio Emergency Medicine GSEP), and Manny Singh, MD (@MPrizzleER, EM Physician at Harbor-UCLA Medical Center, Torrance, CA) // Reviewed by: Alex Koyfman, MD (@EMHighAK)
Case:
A 43-year-old male presents with 1 week of fever, cough, congestion, chest pain, and shortness of breath. He is febrile, tachypneic, and mildly tachycardic. He otherwise doesn’t appear to be in severe respiratory distress, but his oxygen saturation is 77%, and his chest x-ray reveals bilateral infiltrates. What are your next steps? Does he need intubation?
Background
We are in the midst of the COVID-19 pandemic. Many parts of the world have been ravaged by this virus, but disease severity varies significantly. There are several types of patients with COVID-19: those who have mild disease who hopefully we don’t see in the ED, those with mild hypoxemia and symptoms but do well with therapy, those who are moderately to severely hypoxemic but otherwise appear well and may later develop severe symptoms, and those with hyperacute progression who decompensate quickly. The case fatality rate also varies, from less than 2% in those under age 60 years to approaching 10% by 80 years (1-6).
While severe patients with significant illness are the minority of cases, patients with hypoxemia are challenging. Recent literature suggests our strategy of early intubation may not be beneficial and may result in patient harm. What do we have that can help these patients?
This series will evaluate the patient with COVID-19 requiring respiratory support. Our first part in this series will evaluate non-invasive measures and oxygen therapy escalation.
Protection
First, patients with severe COVID-19 who may require respiratory support should be managed in a negative pressure room if possible. These patients should wear a mask while around others, including the waiting room, during transport, or being brought to their room. This includes any supplemental oxygen. If this is not possible, use a private room with closed door. Providers should be in airborne, droplet, and contact precautions with N95 (or equivalent), eye protection, droplet-resistant gown, gloves over the cuff of the gown, cap, and potentially a surgical mask over the face mask if N95s are at a premium (2-6). For more, see this post on PPEs.
Patient assessment
This is one time where you can’t just rely on a number. Many of these patients may look comfortable in the 40-80% saturation range; their hypoxemia does not fit their symptoms. Previously we thought this required intubation immediately. A better way to determine disease severity is to incorporate what the patient looks like. Most patients with hypoxemia but not in severe respiratory distress have normal lung compliance (known as the L type, with low elastance and high compliance). The L type accounts for 70% of patients (7). For these patients, oxygen is the key, not intubation. H type patients have high elastance and low compliance and resemble ARDS. This type accounts for roughly 30% (7).
- L type: Normal amount of gas in lung, low elastance, low ventilation to perfusion ratio, low lung weight, low lung recruitability. Hypoxemia may be due to loss of perfusion regulation and hypoxic vasoconstriction.
- H type: Decreased amount of gas in lung, high elastance, high right to left shunt, high lung weight, high lung recruitability.

*Update: More recent literature has questioned these phenotypes. COVID can present in a heterogeneous manner.
Oxygen Supply Choices
The first-line therapy for those with respiratory distress and/or hypoxemia is supplemental oxygen, with a goal of improving oxygen to > 88-90% and reducing their work of breathing (2-6). You have several tools at your disposal for oxygen: Nasal Cannula (NC), face mask, venturi mask, high flow nasal cannula (HFNC), and noninvasive ventilation(NIV)/noninvasive positive pressure ventilation (NIPPV) (2-6).
Oxygen Escalation Therapy
If the patient is altered, in respiratory failure, or has failed other therapies, then intubate the patient. If the patient does not require emergent intubation, we can use a strategy incorporating escalation of oxygen therapy. At each step, look at the patient, rather than just the oxygen saturation number. Ask the patient how he/she is feeling, and incorporate the respiratory rate into your assessment. If the patient is not improving and feeling worse, then move to the next step. At any point in this escalation, you can use patient repositioning/proning. We will go into this in detail in a future post.

1. Nasal Cannula (NC): Start with a NC at 5-6 liters per minute (LPM). This provides a fraction of inspired oxygen up to 45%, but this varies based on inspiratory peak flow (5). In a patient with NC at 5 LPM with no surgical mask, the dispersion of exhaled air can reach 40 cm (8). Thus, have the patient wear a surgical mask or face mask, which drastically reduces droplet spread and aerosolization (9, 10).

2. Venturi Mask (if available): If the patient does not improve, try a Venturi mask, which provides more precise oxygen delivery between 24-60% via an entrainment device that mixes air with oxygen. Up-titrate based on patient symptoms up to 60% using specified oxygen flow rates (typically 2-15 LPM) (5). Dispersal can reach 40 cm, like the NC (8). Similar to the NC, place a face mask over the Venturi mask to reduce dispersal.
- If this is not available, use a non-breather mask up to 15 LPM. The reservoir bag should be inflated to prevent hypercapnia, which typically needs flow rates over 8 LPM (5). The dispersal is less than 10 cm at 10 LPM (8). Again, cover with face mask.

3. NC + Non-rebreather mask: Your next step is to combine NC with non-rebreather mask, covered by face mask. The NC should be at 6 LPM and non-rebreather at 15 LPM.

4. HFNC: This is your fourth step, which incorporates heated, humidified gas set at a high FiO2. This reduces anatomic dead space, work of breathing, and respiratory rate, while increasing positive pressure, compliance, and oxygen flow (5, 11). Flow rates can reach 60 LPM. Studies evaluating HFNC for hypoxemia in COVID-19 and other disease states have found reduction in mortality and the need for intubation and ICU admission (12-15). The World Health Organization (WHO) and Society of Critical Care Medicine SCCM) recommend HFNC over NIPPV in patients with COVID-19 and respiratory failure (2, 4). There was initial concern of aerosolization with HFNC, but this has not been demonstrated in the literature. Studies suggest HFNC was not a risk factor for transmission during SARS-CoV-1, and based on a simulation study, dispersal at 60 LPM is 4.8-17 cm (16-18). However, there may be a risk of viral dispersal with tube disconnection. These patients should be in a negative pressure room if possible, with staff wearing airborne precautions and a mask over the patient (2, 5, 6).
- Start at 100% FiO2, with the flow rate at 20-30 LPM and titrate up to a maximum of 60 LPM if needed. This will be based on patient comfort level – the higher the rate, the more uncomfortable. Keep in mind this is the opposite of what we normally do, as typically we titrate FiO2 second. See this great video for more.
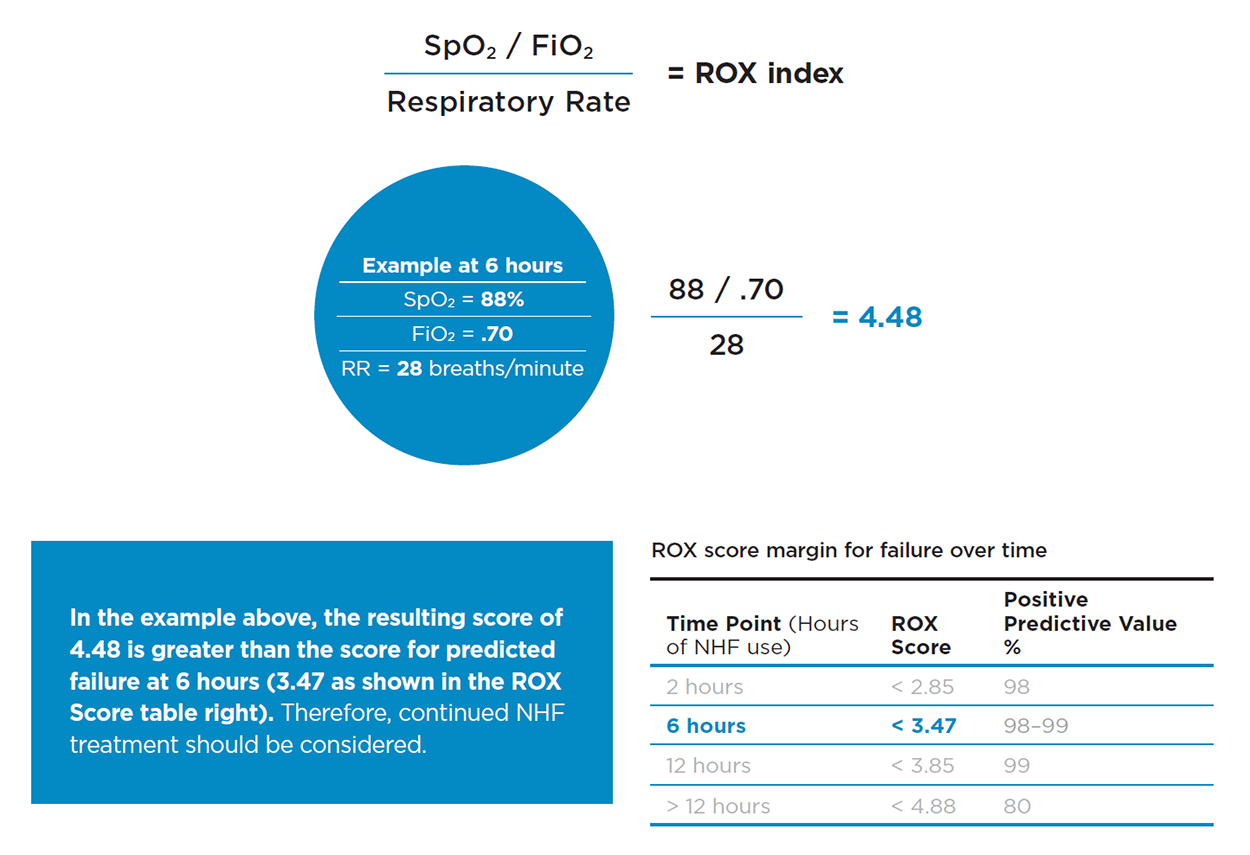
- There is a score to predict who will succeed/fail with HFNC, known as the ROX index , which is performed at 2, 6 and 12 hours (19). This is the ratio of oxygen saturation over FiO2 over respiratory rate. A value of >4.88 means the patient will likely do well with HFNC. You can access it HERE.
- Keep in mind the ROX index may assist, but it is based on low sample sizes and requires further validation. It should not replace your clinical assessment.

5. NIPPV: Your final step in escalation before intubation is NIPPV. Continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BPAP) are your two choices. The key is that these modes provide positive pressure through the respiratory cycle, most commonly with a tight facial mask (5). If you have access to a helmet device, this may reduce viral dispersal and aerosolization. Aerosolization is a risk when using NIPPV, though a tight-fitting mask and viral filter decrease this risk. The dispersal can reach over 1.5 meters with 18 cm H20 (8, 18, 20). The SCCM recommend against NIPPV unless HFNC is not available (4). However, NIPPV has been used with success in China, Italy, and New York.
- The specific mode is an area of debate and controversial. We recommend CPAP to improve oxygenation and reduce lung injury. See this PulmCrit post for a more in-depth dive. CPAP provides a high amount of mean airway pressures, while BPAP mainly assists with ventilation and may assist those with COVID-19 plus obstructive lung or cardiac pathologies. If using NIPPV, full airborne precautions are needed, with viral filters to create a closed ventilation system.

6. Intubation: If the other measures have not resulted in patient improvement, intubation is the final step. Please see this EMCrit resource for an intubation checklist you can adapt to your specifications.
Taking this escalation in oxygen therapy step by step gives you this:

Summary:
- Place patients in negative pressure room if available, and wear appropriate airborne precautions.
- Keep in mind patients may not require immediate ventilation.
- Consider escalation of oxygen therapy: 1) NC up to 6 LPM, 2) Venturi Mask up to 50%, 3) NC at 6 LPM + Non-rebreather at 15 LPM, 4) HFNC, 5) CPAP, 6) Intubation.
- Use awake repositioning.
Tips on NIPPV and creating a CPAP device
> MUST DO in COVID patients for NIPPV
- Full PPE gear.
- Viral filter directly connected to mask before connecting to other things like end tidal, BVM, ventilator (except in the case of inline suction on the ETT in a mechanically ventilated patient).
- You will need adequate seal with Noninvasive Mask. Assure no leak.
- Keep FiO2 at 100. Titrate PEEP as needed to get Sats >88%. Some are tolerating saturations even lower than this so use clinical judgement. Don’t just treat numbers.
- Get a blood gas (preferably ABG) 5-10 minutes after to titrate your settings as needed.
- Make sure if using NIPPV that is a closed system. Some of the BIPAP machines in ED are not closed systems and you will be blowing COVID everywhere. If you are not sure ask.
> Basics on CPAP and BIPAP
- Simple Break Down of CPAP vs. BiPAP – real simple break down of noninvasive positive pressure use.
- Pressure setting in video = PEEP setting on ventilator machine.
Familiarize yourself with what vent systems you have in the department. Below we discuss some tips using the IMPACT system.
> Using a ventilator for CPAP Mode:
- IMPACT Set Up
- Key notes: Need to place connective devices in specific order to decrease exposure.
- ETT/NIV Mask
- Inline suction if ETT present (will need later so do it up front so don’t expose later)!
- Viral Filter
- End Tidal (need in place after viral filter)
- Ventilator tubing
What buttons do I push?
- How to set up CPAP on LT 1200?
CPAP on Impact 2
- Set Pressure to 0 so in CPAP
- Set FiO2 100% to start
- Set PEEP 5 to start
- Can titrate PEEP up if not meeting oxygenation requirements or down if improving.
- DO NOT GO ABOVE PEEP of 20 – consider intubation at this point. If unsure consult someone who knows (ICU, attending, etc..)
- Below is a downloadable step by step guide to using CPAP on an IMPACT 2 ventilator.
BIPAP Mode Set Up on Impact 2
> What if all my ventilators are being used or we run out?
1. How to set up CPAP without ventilator:
- Old school CPAP set up
- Need:
- High flow oxygen generator.
- Peep connective device (not typical PEEP Valve) to patient and turned on to desired PEEP – start at 5 and increase.
2. Making your own CPAP: BVM + PEEP Valve + Oxygen Flow Source
- If no machines (HFNC or vents) available or do not have above set up, this will be a good option.
- Two Methods: Watch both Videos.
- 1. NC under CPAP Mask attached to BVM with Peep Valve
-
- 2. No Nasal Cannula – Using end tidal valve to provide PEEP source – Recommended
> Why BVM with PEEP valve alone doesn’t generate CPAP?
- It will not generate pressure unless you manually bag patient, which is what we want to avoid because of aerosolization. If there is no positive pressure, this leads to de-recruitment of alveoli. These patients desaturate super fast!
> NIV:
- #1 Recommendation: CPAP mode on ventilator for patient not doing well with oxygenation escalation, but not yet needing intubation.
- #2 Recommendation: If ventilators are unavailable and you are making your own CPAP to limit aerosolization, choose second method with no nasal cannula above.
- Remember patients coming to the ED will still have heart failure exacerbations, COPD exacerbations, and other pathologies requiring NIV. Take full PPE precautions when treating these patient, but still utilize your NIV interventions.
- Full Post: EMCrit: COVID Airway Management
Further Reading:
Please see these great #FOAMed pieces for more:
- REBEL EM – COVID-19 Hypoxemia: A Better and Still Safe Way
- EMCrit Wee – Avoid Intubation
- EMCrit COVID Airway Management
- Thinking CC COVID Respiratroy Management
- Respiratory support for adult patients with COVID
*Update:
Based on the RECOVERY trial published in the New England Journal of Medicine, patients requiring supplemental oxygen or mechanical ventilation should receive dexamethasone, 6 mg (PO or IV), which is associated with reduced mortality.
HFNC has proven safe and improves patient comfort. This can improve respiratory fatigue and oxygenation.
Do not just focus on the oxygen saturation in determining need for intubation. Consider mental status, work of breathing, and diaphoresis in your evaluation.
Proning/awake repositioning improves oxygen saturation and reduces pulmonary ischemia. It remains controversial whether it improves lung recruitment in a significant manner.
References:
- Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID‐19) implicate special control measures. Journal of Medical Virology. 2020; http://doi.org/10.1002/jmv.25748.
- Clinical management of severe acute respiratory infection when Novel coronavirus (2019‐nCoV) infection is suspected: Interim Guidance. WHO/nCoV/Clinical/2020.3 January 28 2020.
- Ferguson N, Laydon D, Nedjati Gilani G, et al. Report 9: Impact of non‐pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. Imperial College London 16 March 2020. https://doi.org/10.25561/77482.
- Surviving Sepsis Campaign. COVID-19 Guidelines. Published March 20, 2020. Available at https://www.sccm.org/SurvivingSepsisCampaign/Guidelines/COVID-19. Accessed April 10, 2020.
- Whittle JS, Pavlov I, Sacchetti A, Atwood C, Rosenberg MS, et al. Respiratory Support for Adult Patients with COVID-19. JACEP Open 2020. Published April 2, 2020. https://doi.org/10.1002/emp2.12071
- COVID-19. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html
- Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatment for different phenotypes? Intensive Care Medicine. Available at https://www.esicm.org/wp-content/uploads/2020/04/684_author-proof.pdf
- Hui DS, Chan MT, Chow B. Aerosol dispersion during various respiratory therapies: a risk assessment model of nosocomial infection to health care workers. Hong Kong Med J. 2014; 20(suppl 4): 9‐13.
- Leonard S, Volakis LI, DeBellis R, et al. COVID-19 Transmission Assessment Report. High Velocity Nasal Insufflation (HVNI) Therapy Application in Management of COVID-19. Available at https://vapotherm.com/blog/transmission-assessment-report/
- Kluge S, Janssens U, Welte T, et al. [Recommendations for critically ill patients with COVID‐19]. Medizinische Klinik, Intensivmedizin und Notfallmedizin. 2020. https://doi.org/10.1007/s00063-020-00674-3.
- Nishimura M. High‐flow nasal cannula oxygen therapy in adults: physiological benefits, indication, clinical benefits, and adverse effects. Respir Care. 2016; 61( 4): 529‐ 541.
- Frat JP, Thille AW, Mercat A, et al. High‐flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015; 372(23): 2185‐2196.
- Wang K, Zhao W, Shu W. The experience of high-flow nasal cannula in hospitalized patients with 2019 novel coronavirus-infected pneumonia in two hospitals of Chongqing, China. Ann Intensive Care. 2020;10:37.
- Rochwerg B, Granton D, Wang DX, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta‐analysis. Intensive Care Med. 2019; 45(5): 563‐572.
- Nagata K, Morimoto T, Fujimoto D, et al. Efficacy of high‐flow nasal cannula therapy in acute hypoxemic respiratory failure: decreased use of mechanical ventilation. Respir Care. 2015; 60(10): 1390‐1396.
- Raboud J, Shigayeva A, McGeer A, et al. Risk factors for SARS transmission from patients requiring intubation: a multicentre investigation in Toronto, Canada. PLoS One. 2010; 5( 5):e10717.
- Kotoda M, Hishiyama S, Mitsui K, et al. Assessment of the potential for pathogen dispersal during high‐flow nasal therapy. J Hosp Infect. 2019. https://doi.org/10.1016/j.jhin.2019.11.010.
- Hui DS, Chow BK, Lo T, et al. Exhaled air dispersion during high‐flow nasal cannula therapy versus CPAP via different masks. Eur Respir J. 2019; 53(4). https://doi.org/10.1183/13993003.02339-2018.
- Roca O, Caralt B, Messika J, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high‐flow therapy. Am J Respir Crit Care Med. 2019; 199(11): 1368‐1376.
- Hui DS, Chow BK, Lo T, et al. Exhaled air dispersion during noninvasive ventilation via helmets and a total facemask. Chest. 2015; 147(5): 1336‐1343.









5 thoughts on “COVID-19: Oxygen Escalation Therapy and Noninvasive Ventilation”
Pingback: COVID-19 Hypoxemia: A Better and Still Safe Way - REBEL EM - Emergency Medicine Blog
Pingback: COVID-19: Oxygen Escalation Therapy and Noninvasive Ventilation (emDOCs) – RESQFOAM
Do you recommend humidification whe masal cannula is in place?
Whether to use humidification will vary based on your center. However, humidification is helpful for patient comfort, especially at higher flows. The risk of aerosolization with HFNC is low, especially when covered with a mask over the device.
Pingback: COVID-19: Coronavirus Resources | Impact EMS