Author: Brit Long, MD (@long_brit) // Editor: Alex Koyfman, MD (@EMHighAK)
Welcome to The EM Educator Series. These posts provide brief mini-cases followed by key questions to consider while working. The featured questions provide important learning points for those working with you, as well as vital items to consider in the evaluation and management of the specific condition discussed. This post discusses several components of sepsis evaluation and management in the ED, followed by key references.
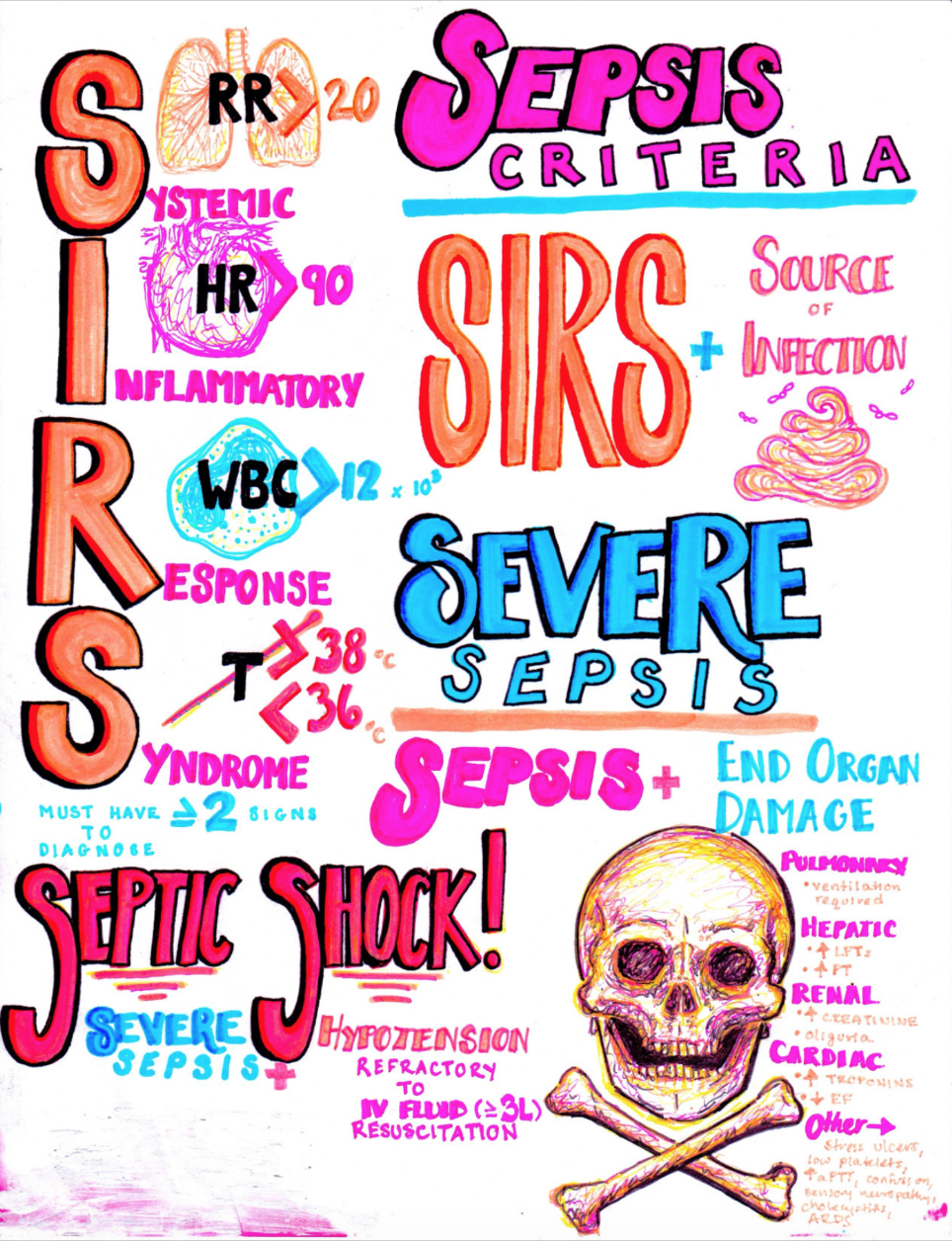
From Hanson’s Anatomy
Mini-Case #1: Diagnosis of Sepsis
A 43-year-old female presents with fever, productive cough, and malaise for one week. She has no medical problems, no allergies, and takes no medications. Exam reveals a tired-appearing woman with HR 112, BP 105/70, RR 22, Sat 93% on RA, and T 38.2. CXR shows a right lower infiltrate, with CBC 12.2, normal renal and liver function, and lactate 2.4.
1. How is sepsis diagnosed, and can you diagnose sepsis for this patient?
2. What are the classic components of EGDT from the Rivers et al. study?
3. With recent literature, what are essential tenants of therapy for sepsis? Is EGDT still required?
4. What is sepsis 3.0?
5. Is sepsis 3.0 ready for use in the ED?
Suggested Resources:
https://lifeinthefastlane.com/ccc/early-goal-directed-therapy-in-sepsis/
https://flippedemclassroom.wordpress.com/2012/12/14/early-goal-directed-therapy-in-sepsis/
https://emcrit.org/isepsis/isepsis-dr-nathanson-reviews-egdt/
http://rebelem.com/rebelcast-sepsis-care-in-2015/
https://coreem.net/core/surviving-sepsis-2017/
https://lifeinthefastlane.com/ccc/initial-sepsis-management/
http://foamcast.org/2016/02/21/sepsis-redefined/
http://rebelem.com/sepsis-3-0/
https://emcrit.org/pulmcrit/problems-sepsis-3-definition/
https://first10em.com/2016/02/25/sepsis-3-0/
https://emcrit.org/emcrit/sepsis-3/
http://stemlynsblog.org/sepsis-16/
Mini-Case #2: Biomarkers and Vasopressors in Sepsis
A 72-year-old male presents with abdominal and costovertebral pain, fever, and decreased PO intake. He has had multiple UTI’s in the past. He has a history of HTN, HLD, and diabetes. He is tired and ill appearing. VS are HR 112, BP 70/42, RR 25, Sat 93% on RA, and T 38.2. CXR is at patient baseline, with CBC 16.2. RFP and LFT’s are at baseline. However, his lactate is 4.1.
1. What does elevated lactate mean?
2. How should lactate be used in sepsis?
3. What other biomarkers are on the horizon, such as procalcitonin (PCT)?
4. When are vasopressors warranted?
5. What is the first line choice for vasopressor?
6. Is a central line needed for vasopressors?
Suggested Resources:
https://emcrit.org/pulmcrit/understanding-lactate-in-sepsis-using-it-to-our-advantage/
https://emcrit.org/isepsis/isepsis-understanding-lactate/
https://emcrit.org/emcrit/lactate/
https://pulmccm.org/review-articles/review-lactate-sepsis/
https://lifeinthefastlane.com/ccc/sepsis-biomarkers/
http://www.emdocs.net/sepsis-biomarkers-whats-new/
http://www.tamingthesru.com/blog/intern-diagnostics/pros-and-cons-of-procalcitonin
https://lifeinthefastlane.com/ccc/procalcitonin/
https://emcrit.org/pulmcrit/early-norepinephrine-to-stabilize-map-in-septic-shock/
https://emcrit.org/pulmcrit/sepsis-myths/
https://emcrit.org/pulmcrit/phenylephrine-epinephrine-central-access/
https://emcrit.org/emcrit/peripheral-vasopressors-extravasation/
https://emcrit.org/emcrit/non-invasive-sepsis/
http://rebelem.com/mythbuster-administration-of-vasopressors-through-peripheral-intravenous-access/
https://emcrit.org/pulmcrit/epinephrine-challenge-septic-shock/
https://emcrit.org/pulmcrit/renal-microvascular-hemodynamics-in-sepsis-a-new-paradigm/
http://www.emdocs.net/septic-shock-who-should-be-treated-with-early-pressors/
Mini-Case #3: Management of the Patient with Sepsis and Comorbidities and Dangers of Over-Resuscitation
A 72-year-old male presents with abdominal and costovertebral pain, fever, and decreased PO intake. He has had multiple UTI’s in the past. He has a history of ESRD on dialysis, severe CHF with poor EF, HTN, and diabetes. He is toxic appearing. VS are HR 115, BP 74/42, RR 23, Sat 91% on RA, and T 38.2. CXR is at patient baseline, with CBC 16.2. His lactate is 3.8.
1. How should this patient with multiple comorbidities be treated with IV fluids?
2. Are there risks to over-resuscitation?
3. If the patient is not responding to normal sepsis treatments, what should you consider? What can you be missing?
Suggested Resources:
http://www.emdocs.net/the-dangers-of-over-resuscitation-in-sepsis/
http://www.emdocs.net/how-much-is-too-much/
http://www.emdocs.net/fluid-choice-does-it-matter/
http://www.emdocs.net/sepsis-comorbidities-management-strategies/
http://www.emdocs.net/sepsis-comorbidities-management-strategies/
http://www.emdocs.net/unstable-sepsis-airway-first-not-always/
http://epmonthly.com/article/sepsis-mimics/
http://www.emdocs.net/early-sepsis-why-do-we-miss-it-and-how-do-we-improve/
http://rebelem.com/occult-causes-of-non-response-to-vasopressors/
https://emcrit.org/emcrit/stop-points/
Bonus:
Your ICU colleague asks if you’ve heard about giving patients with severe sepsis Vitamin C, hydrocortisone, and thiamine, or the “metabolic resuscitation protocol.” What does this entail?
https://emcrit.org/pulmcrit/metabolic-sepsis-resuscitation/
http://rebelem.com/the-marik-protocol-have-we-found-a-cure-for-severe-sepsis-and-septic-shock/
http://www.everydayebm.org/case-based-learning/2017/3/26/vitamincsepsis
https://emcrit.org/isepsis/isepsis-vitamin-c-hydrocortisone-thiamine-qa/








