Author: Danielle Rucker, MD (EM Resident Physician, UTSW, Dallas, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
An 18-year-old female presents with confusion, seizures, and fever. Patient is unable to provide history, but her mother states that she began noticing confusion 2 days ago, and the patient expressed head discomfort yesterday. She has no history of seizures, recent travel, significant family history, or drug or alcohol use. The patient does not take any medications.
Triage vital signs (VS): BP 100/82, HR 118, T 103.2 F, RR 17, SpO2 98% on RA.
The patient appears lethargic and does not follow commands. She has nuchal rigidity and is hyperreflexic with upgoing toes bilaterally.
What is the patient’s diagnosis? What is the next step in your evaluation and treatment?
Answer: Encephalitis
Background:
- Encephalitis is defined as inflammation of the brain parenchyma and differs from meningitis because of its associated brain dysfunction [1]. However, these diseases often overlap and can be referred to as meningoencephalitis. Meningitis refers to inflammation of the meninges covering the brain and is associated with an increased CSF white blood cell count. Encephalitis can also be mistaken for encephalopathy, which refers to an altered level of consciousness for 24 or more hours without evidence of CNS inflammation.
- Altered brain function can manifest in many ways, including (but not limited to) aphasia, seizures, focal neurologic deficits, altered mental status, personality changes, or movement disorders.
- It is usually differentiated from other causes of brain dysfunction by its associated fever and CSF findings.
- Between 2005-2015, hospital admissions attributed to encephalitis were around 250,000. Its incidence over the past several decades is largely unchanged [2].
- Women now have a higher documented incidence of encephalitis than men, which is thought to be due to increased recognition of autoimmune causes [3].
- Mortality is estimated to be between 5-15% and can be as high as 20% in patients admitted to the intensive care unit [4].
- Studies evaluating long-term morbidity have shown risk of decreased IQ, behavioral changes, and sustained neurologic deficits [5].
- Non-reversible poor prognostic factors include advanced age, immunosuppressed state, and co-morbidities [6].
- Reversible poor prognostic factors include thrombocytopenia, cerebral edema, and seizures [7].
Pathophysiology:
- Can either be infectious, non-infectious, or post-infectious cause.
- Infection to the central nervous system is most commonly caused by hematogenous spread resulting in direct invasion of tissue by pathogens. This leads to inflammation due to cytokine release.
- Majority of cases are due to infection, of which HSV-1 is the most common in the United States and Japanese encephalitis is the most common global cause [8, 9].
- HSV-1 is the most common cause of HSV-associated encephalitis in children and adults, while HSV-1 and HSV-2 are causes of encephalitis in neonates. HSV-1 in infants is associated with a poorer prognosis [10, 11].
- Other infectious causes include VZV, EBV, CMV, enteroviruses, arboviruses, bacteria, fungi, protozoa, and helminths.
- Etiology is often not found.
- Severity of encephalitis has not been shown to be related to the underlying cause.
- Anti-NMDA (N-methyl D-aspartate) receptor encephalitis is a common autoimmune cause of encephalitis [12].
- Normally, NMDA receptors are bound by glycine and glutamate.
- In this disease, anti-NMDA receptor antibodies bind to NMDA receptors, leading to cross-linking and internalization of the receptors. This results in a decreased number of receptors which is titer-dependent and reversible.
- It can be triggered by ovarian teratomas, other neoplasms, or infections.
- Typically has neurologic and psychiatric features, which can lead to a delayed diagnosis.
- More common in women.
- Course can be unpredictable but can also follow a stepwise fashion as outlined below:
- Prodromal flu-like illness.
- Psychotic features typically develop after this phase, which can present as hallucinations, delusions, and agitation.
- Neurologic symptoms usually occur after preceding phase, which can consist of seizures, catatonia, and impaired attention.
- Autonomic dysfunction often occurs (marked fluctuations in blood pressure, heart rate, and temperature).
- Relapse is common.
- Tick-borne encephalitis [13]:
- CNS infection transmitted to humans by tick bites.
- It is more common in adults than children.
- It is endemic in Europe and Asia, usually occurring between April and November.
- It can present with meningitis, meningoencephalitis, or encephalitis and can cause paralysis.
- Can result in significant morbidity and prognosis varies based on subtype of disease and genetics.
Anatomy:
- Inflammation of the brain parenchyma that is often coupled with meningeal inflammation.
- In general, the location of the inflammation tends to be gray matter with infectious etiologies and white matter with autoimmune etiologies [14].
Clinical Presentation:
- History [15]:
- May report a prodromal flu-like illness.
- Can present with a variety of neurologic findings, including altered mental status, seizures, and behavior change. Signs of meningeal irritations, such as neck stiffness and photophobia, may also be present. Patients often have fevers.
- Symptoms are typically present for >24 hours at time of presentation.
- Inquire about ill close contacts.
- An extensive travel and vaccination history should be performed.
- Immunocompromised individuals may have more subtle presentation.
- Physical exam [15]:
- May be non-specific besides confusion.
- Neurologic exam may reveal deficits, such as cranial nerve palsies, seizures, hemiparesis, or flaccid paralysis (indicates spinal cord involvement).
- Rash may be present in certain cases (for instance, vesicular rash with VZV or HSV).
- Findings that may point you in a specific direction:
- Lower cranial nerve palsies (disorders of 9th-12th cranial nerves): consider rhombencephalitis, which refers to inflammation of the brainstem or cerebellum.
- Deafness: consider mumps encephalitis, especially in un- or undervaccinated individuals.
- HIV: consider HIV as well as more rare infectious causes (including mycobacteria and fungi).
Differential: non-infective encephalopathy, post-infectious encephalomyelitis, medication adverse effects, tumors, toxic ingestion, sepsis, cerebral malaria, subarachnoid hemorrhage, serotonin syndrome, neuroleptic malignant syndrome, malignant hyperthermia, heat stroke, delirium tremens, stroke (hypothalamic), thyroid storm
Diagnostics:
-
- Diagnostic criteria [16, 17]
- Created by the International Encephalitis Consortium in 2013.
- Major criterion (required): altered mental status for >24 hours without alternative cause.
- Minor criteria (2+ for possible; 3+ for probable or confirmed): fever within 72 hours of presentation; seizures; CSF leukocyte count 5mm^3 or greater; neuroimaging suggestive of encephalitis; new-onset focal neurological deficit; EEG suggestive of encephalitis.
- Confirmed cases require either a brain biopsy, evidence of infection with a microorganism known to cause encephalitis, or evidence of an autoimmune condition associated with encephalitis.
- These criteria cannot be applied stringently in pediatric patients due to the incidence of febrile seizures, higher baseline levels of CSF white blood cell counts, and ability of infants to have infectious encephalitis without pleocytosis.
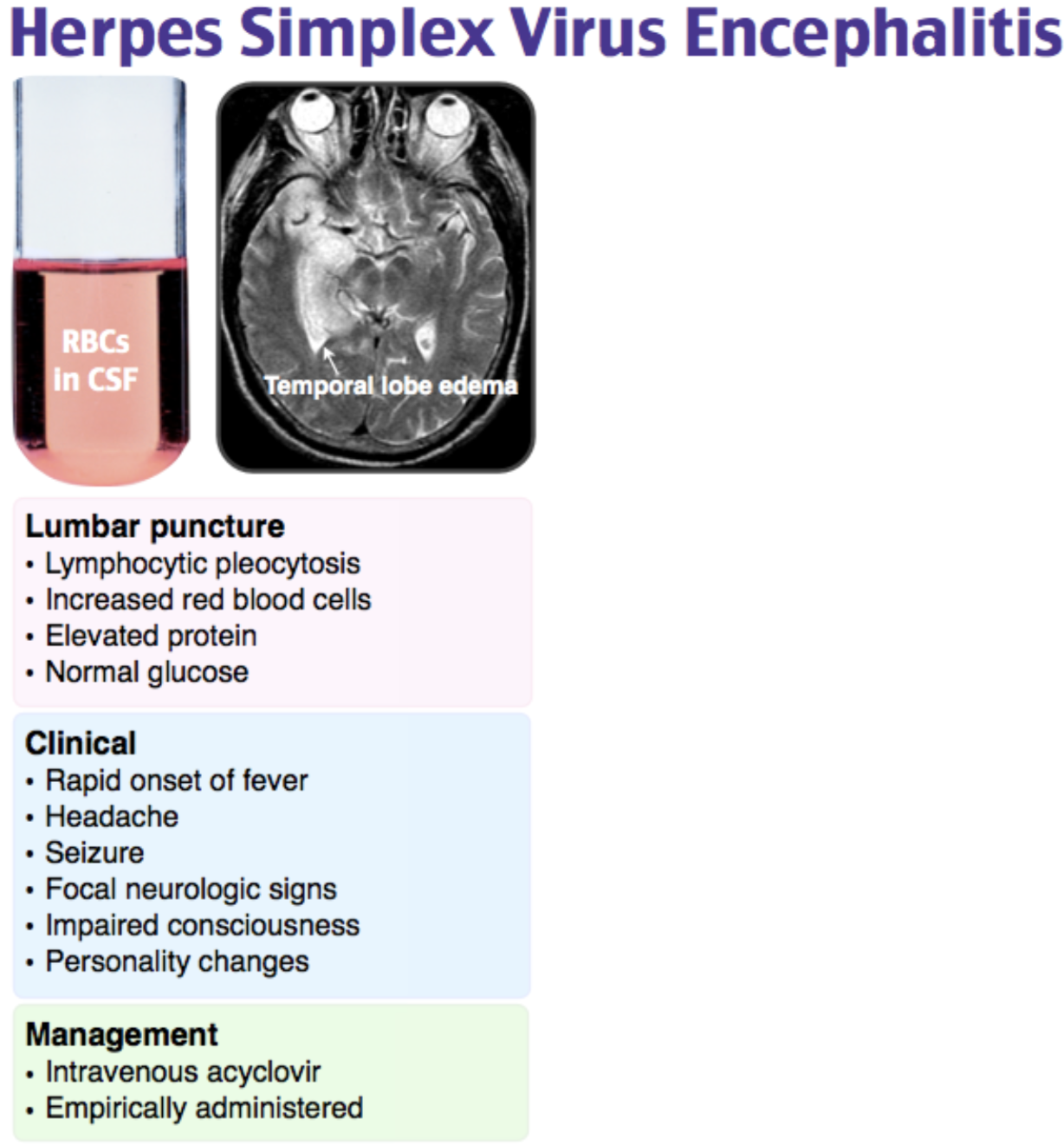
- Lumbar puncture
- Necessary to distinguish encephalopathy from encephalitis.
- Neuroimaging is necessary beforehand if signs of increased intracranial pressure are present (focal neurologic deficits, GCS <12, intractable seizures, or papilledema) [18].
- CSF studies: opening pressure, glucose, protein, cell count, and culture.
- Typical indices are increased cell count (usually less than 250/mm^3) with a lymphocytic predominance (neutrophilic predominance can occur in the earlier stages), elevated protein, and normal glucose[19].
- An increased red blood cell count in the absence of a traumatic tap should raise suspicion for HSV [20].
- At a minimum, additional testing includes HSV-1 and HSV-2 CSF PCRs (repeat if high suspicion and initial PCR is negative), VZV CSF antibodies (more sensitive than PCR), and HIV serum test.
- Further testing for other infectious or autoimmune etiologies should be based on suspicion (for instance, arbovirus or enterovirus testing depending on season and exposure, or autoantibody testing depending on suspicion for an autoimmune cause) [21] [22].
- Repeat lumbar puncture as needed if initial studies are negative and suspicion persists.
- Neuroimaging
- Conventionally, most clinicians will start with a CT head and proceed to an MRI head as indicated.
- Brain imaging is needed to exclude alternative diagnoses (for instance, intracranial mass), assess for mass effect, and to evaluate for brain changes consistent with encephalitis (for instance, temporal lobe changes with HSV-1 encephalitis) [23].
- The preferred MRI study is with and without contrast with FLAIR sequences to best evaluate for inflammation [24].
- Specific changes seen on MRI with HSV encephalitis include inflammation in the temporal and frontal lobes [24].
- EEG: Non-specific, but is used to identify seizure or encephalopathic activity.
- Brain biopsy: Typically, a last resort option in the setting of clinical deterioration or diagnostic uncertainty. However, it is important to note that if the biopsy findings reveal encephalitis, the exact cause is typically not found [25].
- Diagnostic criteria [16, 17]
Management:
- Supportive care [14, 26-28]:
- Persistent re-evaluation of airway, breathing, and circulation. Consider intubation if the patient is not able to protect their airway.
- Increased intracranial pressure: elevate the head of the bed to 30 degrees or more, and consider hypertonic saline (0.1-1 cc/kg/hr with sodium goal of 145-155), mannitol (0.25-1 mg/hr every 4-6 hours), diuretics, or hyperventilation. In general, hypertonic saline is preferred over mannitol. An important caveat is, in the presence of hyponatremia, mannitol tends to be preferred in order to avoid demyelinating phenomena. Avoid hypoxia, hypotension, and elevated temperature. Fevers have been associated with increased intracranial pressure and subsequent neurological insult.
- Seizures: prophylactic management with anticonvulsants, such as levetiracetam, valproic acid, or phenytoin. Levetiracetam is sometimes not preferred in this situation due to its associated drowsiness.
- Steroids: not routinely recommended.
- Empiric acyclovir (10 mg/kg intravenously every 8 hours) is usually started in all cases of suspected encephalitis because of a decrease in morbidity and mortality and the prevalence of HSV encephalitis relative to other causes of encephalitis [29, 30].
- Antibiotics are typically recommended as well until bacterial etiologies are excluded.
- Treatment for other etiologies of encephalitis depending on clinical presentation (for instance, if considering anti-NMDA receptor encephalitis, steroids and intravenous immunoglobulin or plasma exchange are indicated. For tick-borne encephalitis, there is no specific treatment but vaccination can be largely preventative).
Complications:
-
- Cerebral edema: this can be further complicated by mass effect and increased intracranial pressure. If concerned for sudden increase in intracranial pressure, obtain CT head. Additionally, suspect herniation if patient develops either unilateral or bilateral pupils that are dilated and unresponsive to light [31].
- Seizures: this can occur in up to 15% of patients with encephalitis. If this occurs, an emergent electroencephalogram (EEG) should be performed.
- In light of active seizure activity, assess the patient’s airway, breathing, and circulation. Place the patient on supplemental oxygen and turn them on their side if feasible.
- First-line medicinal management with benzodiazepines: lorazepam IV (0.1 mg/kg–usual loading dose is 4 mg), midazolam IM (0.2 mg/kg–max dose 10 mg), or diazepam rectally (0.1-0.15 mg/kg–max dose 10 mg per dose) [32].
- Patients with seizures refractory to first-line medications should be started on second-line medications, including valproic acid (30 mg/kg), fosphenytoin or phenytoin (20 mg/kg), or levetiracetam (60 mg/kg) [33]
- Status epilepticus, which is defined as 5 or more minutes of seizing or 2 or more seizures without return to baseline, has a mortality rate of up to 50% in the general population and may exceed 75% in the elderly [34].
- Recurrence: HSV encephalitis has been associated with relapse, which is thought to occur by an immune-mediated pathway as opposed to cytotoxic destruction of cells [35].
Disposition:
- Admission for empiric acyclovir (since HSV is the most common cause of encephalitis in the United States) and supportive care.
- Around 25% of patients may require intensive care unit admission [36].
- Consider admission to a neurological service, and if not, ensure neurologists are working closely with your team.
- Since criteria for encephalitis includes altered mental status of unknown origin, these patients are not appropriate for discharge.
- If cause is noted to be HSV, duration of treatment is between 14-21 days [37].
Take-Home Points:
- Encephalitis is defined as brain parenchymal inflammation with associated neurologic dysfunction.
- It’s often coupled with signs of infection, such as a fever and abnormal CSF studies.
- The most common cause of encephalitis in the United States is HSV.
- All patients with suspected encephalitis should be started on empiric acyclovir early, as this has been shown to decrease morbidity and mortality.

A 53-year-old woman with a history of bipolar disorder, depression, substance abuse, and hypertension presents to the emergency department from her group home with altered mental status. Her caseworker reports that two days ago, she started to become more agitated. Her psychiatric medications were then increased due to this agitation, but the medication list was not brought from the group home. Today, she spiked a fever and had more difficulty speaking. Upon arrival, her vital signs include a temperature of 38.6°C, pulse 108 bpm, blood pressure 144/78 mm Hg, respiratory rate 14 breaths per minute, and oxygen saturation 98% on room air. Her physical exam reveals confusion and dysphasia without focal neurologic deficits. A CT scan of her head without contrast is normal. The most appropriate next step is administration of which of the following?
A) Acyclovir, ceftriaxone, and vancomycin
B) Cyproheptadine
C) Dantrolene
D) Haloperidol and lorazepam
Answer: A
This patient has signs of acute encephalitis, possibly due to herpes simplex virus (HSV). HSV-1 is the most common cause of encephalitis. HSV encephalitis occurs most commonly in patients under 20 years old and patients over 50 years old. The gold standard for diagnosis is PCR of the cerebrospinal fluid for HSV. Computed tomography of the brain may show asymmetric enhancement across the temporal lobes, however, abnormal radiographic findings are not required for the diagnosis. HSV encephalitis is thought to be due to a latent infection spreading to the brain via the olfactory or trigeminal nerve. The rate of mortality is 30% with treatment, compared to a 70% mortality if left untreated. Patients present with acute onset of fever and altered mental status. Common findings include agitation, dysphasia, seizures, and personality changes. The mainstay of treatment is acyclovir. It is recommended to also empirically treat for bacterial meningitis with ceftriaxone and vancomycin due to the difficulty in differentiating between the two without CSF test results.
Cyproheptadine (B) is the recommended treatment for serotonin syndrome. While it may also present with fever and altered mental status, this patient lacks the classic findings of hyperreflexia, clonus, diaphoresis, and mydriasis. Dantrolene (C) is the treatment for neuroleptic malignant syndrome. This also may present with fever and altered mental status, but this patient lacks the classic finding of “lead pipe” muscle rigidity. In addition, dysphasia is not a common finding in serotonin syndrome or neuroleptic malignant syndrome. Haloperidol and lorazepam (D) are not appropriate as the primary treatment in HSV encephalitis. While patients with encephalitis may present with severe agitation requiring chemical sedation, this scenario does not indicate an immediate safety risk to the patient or staff. Additionally, the patient presented with a fever, and should first be empirically treated for meningoencephalitis with HSV coverage.
Further Reading:
FOAMed:
- https://emcrit.org/ibcc/meningitis/#antibiotic_selection
- https://www.aliem.com/anti-nmda-receptor-encephalitis/
- http://www.emdocs.net/hsv-encephalitis/
- http://www.emdocs.net/medical-malpractice-insights-delayed-diagnosis-viral-encephalitis/
- https://emcrit.org/wp-content/uploads/2017/01/meningitis.pdf
- https://www.racp.edu.au/docs/default-source/default-document-library/imj-consensur-guidelines-may-2015.pdf?sfvrsn=2
- https://n.neurology.org/content/neurology/early/2020/0123/WNL.0000000000008934.full.pdf
References:
- Bradshaw MJ and Venkatesan A. “Herpes Simplex Virus-1 Encephalitis in Adults: Pathophysiology, Diagnosis, and Management.” Neurotherapeutics. 2016 Jul; 13(3): 493–508.
- Venkatesan A, Tunkel AR, Bloch KC, et al. “Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium.” Clin Infect Dis 2013; 57:1114-1128.
- George BP, Schneider EB, Venkatesan A. “Encephalitis hospitalization rates and inpatient mortality in the United States, 2000-2010.” PLoS One 2014; 9:e104169.
- Venkatesan A. “Epidemiology and outcomes of acute encephalitis.” Neurology. 2015 June; 28(3): 277-82.
- Michaeli O, Kassis I, Shachor-Meyouhas Y, et al. “Long-term motor and cognitive outcome of acute encephalitis.” Pediatrics 2014; 133:e546-e552.
- Mailles A, Stahl JP. “Infectious encephalitis in France in 2007: a national prospective study.” Clin Infect Dis 2009; 49:1838-1847.
- Thakur KT, Motta M, Asemota AO, et al. “Predictors of outcome in acute encephalitis.” Neurology 2013; 81:793-800.
- Venkatesan A, et al. “International Encephalitis Consortium.” Clin Infect Dis. 2013 Oct; 57(8):1114-28.
- Venkatesan A. “Epidemiology and outcomes of acute encephalitis.” Curr Opin Neurol. 2015 Jun; 28(3):277-82.
- Corey L, et al. “Difference between herpes simplex virus type 1 and type 2 neonatal encephalitis in neurological outcome.” Lancet. 1988; 1(8575-6):1.
- Thakur KT, Motta M, Asemota AO, et al. Predictors of outcome in acute encephalitis. Neurology 2013; 81:793-800.
- Liu C et al. “Anti-N-Methyl-D-aspartate receptor encephalitis: A severe, potentially reversible autoimmune encephalitis.” Mediators Inflamm. 2017; 2017: 6361479.
- Bogovic P and Strle F. “Tick-borne encephalitis: A review of epidemiology, clinical characteristics, and management.” World J Cli Cases. 2015 May 16; 3(5): 430-41.
- Kumar R. “Understanding and managing acute encephalitis.” Version 1. F1000Res. 2020; 9: F1000 Faculty Rev-60.
- Messascar K, et al. Infect Dis Clin North Am. “Encephalitis in US Children.” Author manuscript; available in PMC 2019 March 01.
- Venkatesan A and Geocadin R. “Diagnosis and management of acute encephalitis.” Neurol Clin Pract. 2014 Jun; 4(3): 206–215.
- Aryee A and Thwaites G. “Viral encephalitis in travellers.” Clin Med (Lond). 2015 Feb; 15(1): 86–90.
- Ellul M and Solomon T. “Acute encephalitis-diagnosis and management.” Clin Med (Lond). 2018 Apr; 18(2): 155–159.
- Negrini B, Kelleher KJ, and Wald ER. “Cerebrospinal fluid findings in aseptic versus bacterial meningitis.” Pediatrics. 2000 Feb; 105(2):316-9.
- Feigin R and Shackelford P. “Value of repeat lumbar puncture in the differential diagnosis of meningitis.” N Engl J Med. 1973; 289(11):571.
- Cinque P, et al. “The role of laboratory investigation in the diagnosis and management of patients with suspected herpes simplex encephalitis: a consensus report. The EU Concerted Action on Virus Meningitis and Encephalitis.” J Neurol Neurosurg Psychiatry. 1996 Oct; 61(4):339-45.
- Kennedy PGE. “Viral encephalitis: causes, differential diagnosis, and management.” J Neurol Neurosurg Psychiatry 2004; 75(Suppl I):i10–i15.
- Saraya AW, et al. “Normocellular CSF in herpes simplex encephalitis.” BMC Res Notes. 2016; 9:95.
- Chow FC, Glaser CA, Sheriff H, et al. “Use of clinical and neuroimaging characteristics to distinguish temporal lobe herpes simplex encephalitis from its mimics.” Clin Infect Dis. 2015; 60(9):1377–83.
- Gelfand J, et al. “Encephalitis of unclear origin diagnosed by brain biopsy.” JAMA Neurol. 2015; 72(1):66-72.
- Ragland J and Lee K. “Critical Care Management and Monitoring of Intracranial Pressure.” J Neurocrit Care. 2016; 9(2):105–12.
- Hoke C, et al. “Effect of high-dose dexamethasone on the outcome of acute encephalitis due to Japanese encephalitis virus.” J Infect Dis. 1992 Apr; 165(4):631-7.
- Roos KL. Lumbar puncture. Semin Neurol 2003; 23:105–114.
- Whitley R. “Viral encephalitis.” N Engl J Med. 1990; 323(4):242.
- Benson P and Swadron S. “Empiric acyclovir is infrequently initiated in the emergency department to patients ultimately diagnosed with encephalitis.” Ann Emerg Med. 2006;47(1):100.
- Tan IL, Mowry EM, Steele SU, et al. Brainstem encephalitis: etiologies, treatment, and predictors of outcome. J Neurol 2013; 260:2312–2319.
- Alldredge BK, et al. “A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus.” N Engl J Med. 2001; 345(9):631.
- Kapur J, et al. “Randomized Trial of Three Anticonvulsant Medications for Status Epilepticus.” N Engl J Med. 2019; 381(22):2103.
- Logroscino G, et al. “Long-term mortality after a first episode of status epilepticus.” Neurology. 2002 Feb 26; 58(4):537-41.
- Skoldenberg B, et al. “Incidence and pathogenesis of clinical relapse after herpes simplex encephalitis in adults.” J Neurol. 2006 Feb; 253(2):163-70.
- Venkatesan A, Tunkel AR, Bloch KC, et al. “Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium.” Clin Infect Dis 2013; 57:1114–1128.
- Valencia I, et al. “Relapse of herpes encephalitis after acyclovir therapy: report of two new cases and review of the literature.” Neuropediatrics. 2004; 35(6):371.








