Author: Christopher J. Nelson, MD (EM Resident Physician, UTSW, Dallas, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 73-year-old male with a history of hypertension presents to the ED with a 2-month history of hiccups. He reports difficulty eating and sleeping secondary to hiccups. He has tried multiple maneuvers from breath holding to biting lemons to drinking water upside-down. His vital signs and exam are normal, including neurologic exam.
What is your diagnosis?
Answer: Intractable Hiccups
Background:
- Hiccups are also known as hiccoughs or singultus
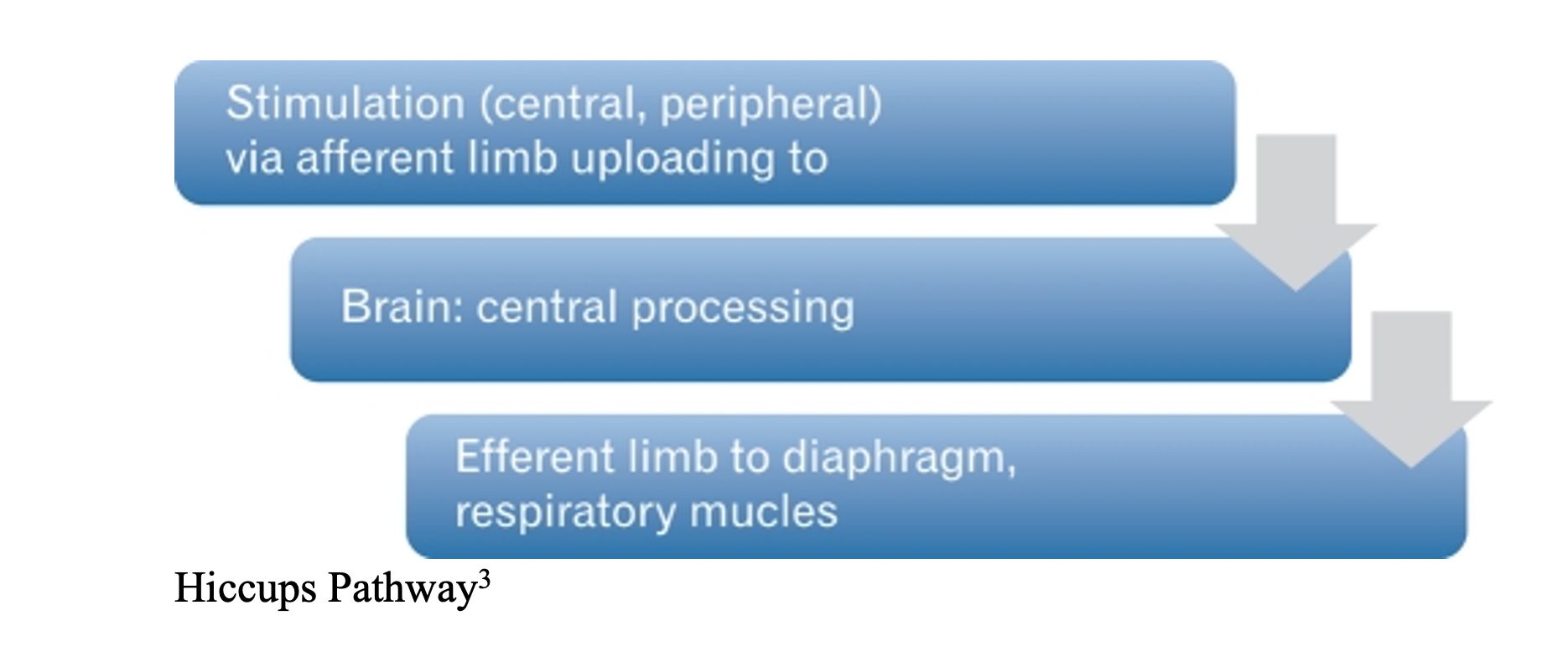
- Hiccups are the involuntary/synchronous spasm of the diaphragm/intercostal muscles resulting in sudden inspiration and glottic closure leading to the well-known “hic” sound1
- Commonly thought to be related to phrenic, vagal, and sympathetic nerve arcs, although other etiologies must be considered2
- Central causes are thought to stem from hypothalamic and medullary respiratory centers2
- May occur as high as 100 times per minute even during sleep leading to significant distress
- Hiccup Bout: Less than 48 hours
- Persistent Hiccups: 48 hours to 1 month
- Intractable Hiccups: Greater than 1 month3
Epidemiology:
- Found in numerous mammalian species4
- Almost all experience hiccups at some point during life
- Intractable hiccups found to be male dominant in non-CNS causes with an odds ratio of 2.425
- Younger ages affected more commonly in females5
- Less likely organic cause in children and full team infants4
- Studies have not shown racial or socioeconomical trends4,5
Assessment:
- Assess time of onset, duration, frequency, relieving/exacerbating factors
- Medical history that increases risk of intractable hiccups – Cancer, AIDS, recent weight loss, dysphagia, GERD, blunt trauma2
- Medications than lead to hiccups – Chemotherapeutic agents, benzodiazepines, corticosteroids6
- Surgical – Recent surgery/procedure (HEENT, chest, abdomen), as well as intubation
- Review of symptoms and exam
- ENT
- Throat/chest burning/GERD symptoms, difficulty swallowing
- Ear canal exam7
- Cardiac – Hiccups can be an atypical symptom of ACS8
- Chest pain, SOB, numbness, tingling, epigastric pain, nausea, vomiting
- Neurologic – Consider infarct
- CN II-XII, cerebellar testing (finger-to-nose, heel-to-shin), ambulation, strength, sensation, reflexes
- ENT
Hiccups Differential Diagnosis:
- Central Nervous System
- Stroke, tumors, injury, seizure
- Cardiac
- ACS
- GI
- Gastroesophageal reflux disease, esophageal tumors
- Drugs
- Chemotherapeutic agents, steroids, psychiatric medications
- Electrolyte abnormality
- Hyponatremia, hypokalemia
- Procedures
- Intubation, bronchoscopy, esophagogastroduodenoscopy, central venous catheter
- Miscellaneous
- Cancer, EtOH use
- Toxin mediated
Clinical Presentation:
- This is a clinical diagnosis
- Sudden feeling of involuntary diaphragm contractions and inspiration followed by pause in breath and classic “hic” sound
- Typically ranging from 30-100 hiccups per minute
- Normally self-resolving by 48 hours of onset without intervention
- Considered persistent if greater than 48 hours and intractable if greater than 1 month3
- Persistence during sleep may suggest organic cause9
Evaluation:
- Generally conservative unless history or physical suggest otherwise
- External auditory canal exam for foreign body or hair against tympanic membrane7
- CMP – Sodium most common electrolyte culprit10
- CBC – If infection suspected
- Less common labs but considered in the right clinical context
- EtOH, Lipase, UA, CSF studies
- Consider CXR for mass vs. structural abnormality
- Consider evaluation for cardiac cause with ECG, CXR, troponin, BNP
- CNS imaging as directed by history and exam – CT head vs. CTA head/neck vs. MR brain
Treatment:
- Conservative treatment typically involves glottic stimulation/manipulation
- Breath holding
- Large gulps of water
- Drinking water upside-down
- Vagal maneuvers
- Pharyngeal vs. nasopharyngeal stimulation with nasopharyngeal tube or foley11
- Pharmacologic – Reserved for symptoms greater than 48 hours
- PPI – Often first line, GERD treatment
- Omeprazole 20 mg daily12
- Pantoprazole 40 mg daily12
- Other medications – similar in efficacy with varying side effect profiles
- Metoclopramide: 10 mg IV/IM; 10–20 mg PO TID x 10 days13
- Chlorpromazine: 25-50 mg IV in 500-1000 mL NS over at least 1 hour, 25 mg QID, increase to 50 mg if needed4
- Only medication FDA approved for hiccups7
- Gabapentin: 300 mg TID14
- Baclofen: 5 mg BID to 20 mg TID15,16
- Less commonly cited treatment
- Haloperidol: 2-5 mg IM vs. PO, can continue 1-4 mg TID PO4
- PPI – Often first line, GERD treatment
Disposition:
- Discharge uncomplicated cases, able to tolerate PO
- If complex secondary cause is identified such as stroke, mass, etc., admission may be required
Pearls:
- Hiccups are common
- Defined as intractable when persistent for greater than 48 hours
- Do not miss organic causes: cardiac, neurologic, electrolyte, toxic ingestion/exposure, structural, cancer
- Conservative treatment first, pharmacologic second line
- No clear first-line drug choice
- Consider case-by-case and side-effect profiles
References:
- Calsina-Berna A, Garcia-Gomez G, Gonzalez-Barboteo J, et al. Treatment of Chronic Hiccups in Cancer Patients: A systemic Review. Journal of Palliative Medicine. 2012;12(15):10. DOI: 10.1089/jpm.2021.0087.
- Samuels L. Hiccup; a ten-year review of anatomy, etiology, and treatment. Can Med Assoc J. 1952;67(4):315-322.
- Chang FY, Lu CL. J Neurogastroenterol Motil. 2012;18(2):123–130. DOI: 10.5056/jnm.2012.18.2.123.
- Kolodzik PW, Eilers MA. Hiccups (singultus): review and approach to management. Ann Emerg Med. 1991;20:565-573.
- Lee GW, Kim RB, Go SI, et al. Gender Differences in Hiccup Patients: Analysis of Published Case Reports and Case-Control Studies. J Pain Symptom Manage. 2016; 51:278.
- Thompson DF, Landry JP. Drug-induced hiccups. Ann Pharmacother. 1997 Mar;31(3):367-9. doi: 10.1177/106002809703100318. PMID: 9066948.
- Cardi E. Hiccups associated with hair in the external auditory canal – Successful treatment by manipulation. N Engl J Med. 1961;265:286.
- Hovey J, Perwez T, Regula P, Chaucer B, et al. Acute Coronary Syndrome Presenting With Hiccups. Cureus. 2021;13(7):e16244. DOI:10.7759/cureus.16244
- Sonadjian J, Cain J. Intractable hiccups: Etiological factors in 220 cases. Postgrad Med. 1968;43:72-77.
- Jones JS, Lloyd T, Cannon L. Persistent hiccups as an unusual manifestation of hyponatremia. J Emerg Med. 1987;5(4):283-7. DOI: 10.1016/0736-4679(87)90256-3. PMID: 3624834.
- Salem MR, Baraka A, Rattenborg CC, et al. Treatment of Hiccups by Pharyngeal Stimulation in Anesthetized and Conscious Subjects. JAMA. 1967;202(1):32–36. doi:10.1001/jama.1967.03130140090014.
- Heidelbaugh JJ, Nostrant TT, Kim C, et al. Management of gastroesophageal reflux disease. Am Fam Physician. 2003;68(7):1311-1318.
- Wang T, Wang D. Metoclopramide for patients with intractable hiccups: a multicentre, randomized, controlled pilot study. Intern Med J. 2014;44(12a):1205-9. doi: 10.1111/imj.12542. PMID: 25069531.
- Hernandez JL, et al. Gabapentin for intractable hiccup. Am J Med. 2004;117:279-281.
- Woelk CJ, Managing hiccups. Can Fam Physician. 2011;57(6):672-e201.
- Ramirez FC, Graham DY. Treatment of intractable hiccup with baclofen: results of a double-blind, randomized, controlled, cross-over study. A J Gastro. 1992;87:1789-91.








