Author: Adam Heilmann, MD (EM Resident Physician, Washington University in Saint Louis) // Reviewed by: Jay Khadpe, MD (@resusjay) and Alex Koyfman, MD (@EMHighAK)
Case
A 28-year-old male with no pertinent medical history presents to the emergency department (ED) after a highway-speed motor vehicle collision (MVC). The patient was an unrestrained driver with possible loss of consciousness and is hypotensive in the field. Upon arrival to the ED, the patient is awake but drowsy and complaining of generalized abdominal pain. The abdomen is soft but tender in the suprapubic region with instability. A pelvic binder is placed; BP is 90/40 with a heart rate of 115 and oxygen saturation of 98% on room air.
Hemorrhagic Shock and Volume Resuscitation
Given the initial presentation, there is concern for hemorrhagic shock in this patient and they will require aggressive resuscitation. Interventions must be performed quickly, and monitoring blood products or fluid administration can be difficult while managing a polytrauma patient.
Let’s take a closer look at hemorrhagic shock in the trauma patient. The most overt markers of hemorrhagic shock are hypotension and tachycardia, but signs may be more insidious. According to the ATLS guidelines, hypotension and tachycardia occur after approximately 30% of blood volume is lost however some patients may not have a robust heart rate change (especially if on nodal blocking agents). In fact, the American College of Surgeons report that up to 1500mL of blood can be lost with minimal change in blood pressure and up to 750mL with almost no clinical signs other than anxiety1. Many patients present with lower SBP and even altered mental status without tachycardia or other “classic” signs of shock8.

Regardless of whether overt signs of shock are present, it is imperative to utilize your clinical exam to help identify potential sources of hemorrhage. Does the patient have a tender abdomen or signs of peritonitis? Is the patient diaphoretic? Are there signs of pelvis instability? Is the thigh compartment firm? Early identification of sources of active hemorrhage may be more important than blood product or fluid administration in patients who are in the early stages of hemorrhagic shock. Meanwhile, the Focused Assessment with Sonography in Trauma or FAST exam can identify >100mL of blood in the peritoneal and pericardial spaces, again, directing management to the source injury1.
These polytraumas can be complex with multiple etiologies for their shock. To consolidate the chaos and organize the differential, identifying the most significant source of hemorrhage and obtaining control should be the top priority, even more important than blood product or crystalloid resuscitation. Volume resuscitation may cause additional harm in the setting of continued hemorrhage, causing a positive feedback loop exacerbating the patient’s shock state.

In the trauma patient with hemorrhagic shock, the initial treatment should be blood product administration. Infusion of packed red blood cells (PRBCs) alone has been shown to worsen coagulopathies of trauma, diluting clotting products (platelets, factors, fibrin) and leading to worse outcomes with massive transfusion. Initial resuscitation with uncrossmatched blood may be necessary but large volume resuscitation of these products can lead to increase in mortality2. The advent of 1:1:1 (PRBCs:Plasma:Platelets) in the form of the massive transfusion protocol mobilizes all blood products in anticipation of large volume resuscitation. This technique reduces the total number of products required thereby decreasing the risk of transfusion related complications3.
Often, complications of volume resuscitation are not apparent until the patient is in the Intensive Care Unit (ICU) or Operating Room (OR), however that doesn’t mean it can’t happen in the ED. Many of the warning signs that a patient is over resuscitated are subtle and confounded by their traumatic injuries or concomitant illnesses. Your patient becomes acutely short of breath. Is this from volume overload, pulmonary contusions, pneumothorax, or the patients’ known hemothorax with a chest tube? During a trauma resuscitation, it is important, but also very difficult, to be cognizant of the products and medications administered as well as their potential side effects.
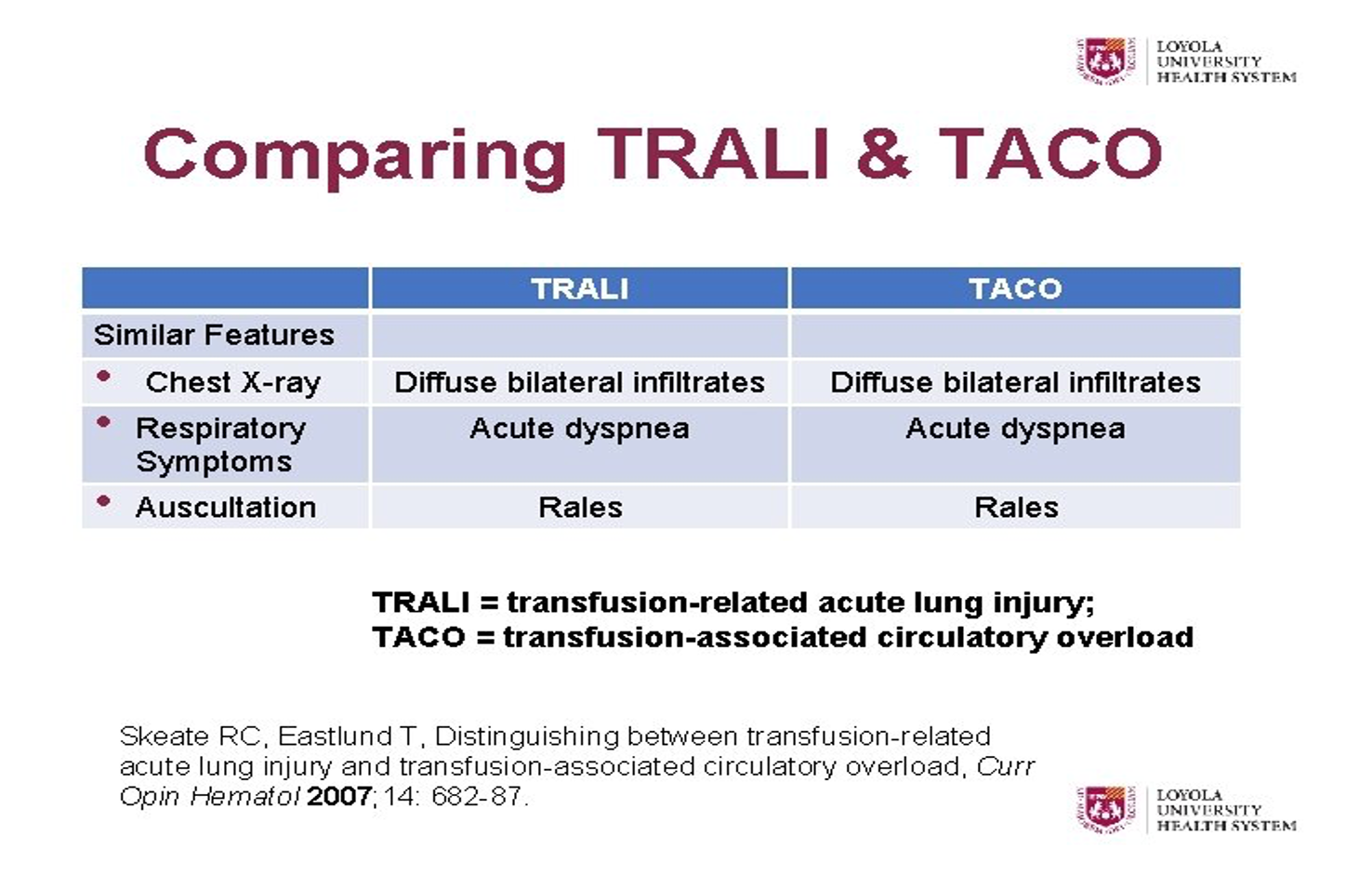
Despite utilization of balanced blood products, source control, and volume resuscitation, patients can still experience complications when receiving large volumes. Two of the more recognized reactions are the Transfusion Related Acute Lung Injury (TRALI) and Transfusion Associated Circulatory Overload (TACO).
TRALI
Coined in the 1980’s, TRALI was described as a phenomenon of lung injury related to leukoagglutinins in blood products. In 2004, the National Heart, Lung and Blood Institute (NHLBI) redefined criteria for TRALI:

The majority of cases are in relation to plasma-containing products. Early studies report 1:432 plasma transfusions10result in TRALI compared to 1:557,000 PRBC9 transfusions though this incidence is likely underreported in part due to nonspecific symptoms. Symptoms can occur as early as minutes to 1-hour post-transfusion with as little as 4 units of transfused blood4,9-10. Again, the signs and symptoms can be insidious especially in a critically ill patient. The main clinical findings are tachycardia, tachypnea, and hypoxia – all which can be seen in severe traumatic injury as well. The pathophysiology is primarily thought to be due to antibodies causing agglutination of leukocytes which get stuck in lung capillaries leading to cytokine release and autoinflammatory reactions5, 9-10.

Treatment for TRALI is, as you can expect, supportive care. It can be viewed similarly to a transfusion reaction with initial steps of terminating blood/blood product administration. Unlike TACO, described below, the patient with TRALI is often under-resuscitated and diuresis can precipitate worsening hypovolemia and hypotension. Mortality is reported as 6-14%, however, this is difficult to assess in patients with multiple comorbidities5. Many of these patients require mechanical ventilation and their polytrauma poses another layer of risk. Limited data is available regarding the use of steroids, so their role remains unclear. Treatment is similar to ARDS with diffuse pulmonary infiltrates, which makes sense considering TRALI fits the clinical criteria for ARDS11. While this is more often encountered in secondary hospital, clinicians should be aware and it should be considered in patients receiving massive transfusion.
 TACO
TACO
Transfusion associated circulatory overload is the second transfusion complication we will discuss. Similar to volume overload in a patient with congestive heart failure, volume resuscitation and transfusion can lead to circulatory overload. However, there is also evidence for a cytokine mediate response that contributes to the volume and circulatory overload. Studies evaluating leukoreduced blood products showed a 50% reduction in incidence of TACO. Both TRALI and TACO can occur with as little as 4 units of blood products . However, TACO usually takes longer to take effect. Unlike TRALI, TACO typically takes up to 6 hours post transfusion to manifest12. TACO also differs from TRALI in that TACO has evidence of heart strain and volume overload. Patients initially present with shortness of breath or increasing oxygen requirement but unlike TRALI, these patients may show hypertension, distended neck veins, S3 gallop, or lower extremity edema on physical exam6. You can also differentiate the two with echo or ultrasonographic findings. TACO may reveal new or worsening signs of systolic heart failure such as reduced ejection fraction and elevated PA pressure.
Much like TRALI, the main treatment is supportive care including oxygen support and mechanical ventilation if necessary and of course discontinuing the transfusion6. Because TACO is more of a problem with volume overload, non-invasive ventilation and diuresis may be beneficial. The most effective strategy against these transfusion reactions is prevention and being mindful of these complications.
So, what have we learned? Unfortunately, these complications are easy to miss, hard to differentiate, and don’t have good treatment options. The best treatment may be prevention. But is it safe to show restraint in the volume resuscitation of our hemorrhagic shock trauma patients?
Multiple studies have evaluated the role of permissive hypotension in trauma7. One meta-analysis in 2018 reviewed 5 randomized control trials comparing permissive hypotension, defined as MAP of 50, to conventional resuscitation, MAP of 60-100mmHg13. This study showed clinically significant reduction in 30-day mortality with permissive hypotension in the trauma patient with hypovolemic shock compared to those resuscitated with greater than 4 units of blood or blood product7,13. Four of the trials reviewed in this analysis showed an overall survival benefit at 30 days and in hospital mortality7,13-15. These data are not definitive and come with many confounders, but the authors did show a reduction in hypothermia, coagulopathies, and transfusion reactions in secondary analyses. Titrating MAP to signs of perfusion such as mental status or urine output may be a reasonable strategy in this patient population to prevent the potential life-threatening complications associated with large volume resuscitation.
Key Points
- TRALI is a fatal transfusion complication presenting similar to ARDS.
- It can occur with as little as 4 units of blood products, more likely plasma.
- It can occur as early as minutes to one hour and up to 6 hours post-transfusion.
- Tachycardia, tachypnea, and hypoxia have several possible causes in a critically ill trauma patient, TRALI can be easily missed.
- Treatment is largely supportive care; diuresis and steroids do not show benefit.
- TACO leads to volume overload and heart strain.
- Hypertension, reduced EF, elevated PA pressures, JVD, and lower extremity edema help to differentiate from TRALI.
- In addition to supportive care, diuretics and BiPAP may be beneficial.
- Permissive hypotension may be a beneficial strategy in trauma patients with hemorrhagic shock.
- It’s reasonable to be judicious with volume resuscitation even in critically ill patients.
References
- Young, Andrew J., and Jeremy W. Cannon. “Hemorrhagic Shock.” Evidence-Based Critical Care, 2020; 711–718., https://doi.org/10.1007/978-3-030-26710-0_95
- Black, Jonathan A., et al. “The Evolution of Blood Transfusion in the Trauma Patient: Whole Blood Has Come Full Circle.” Seminars in Thrombosis and Hemostasis, 2019;46(2): 215–220., https://doi.org/10.1055/s-0039-3402426
- Cotton, Bryan, et al. “A Randomized Controlled Pilot Trial of Modified Whole Blood versus Component Therapy in Severely Injured Patients Requiring Large Volume Transfusions.” Annals of Surgery, 2014;260(1): 178. https://doi.org/10.1097/sla.0000000000000820
- Triulzi, Darrell J. “Transfusion-Related Acute Lung Injury: Current Concepts for the Clinician.” Anesthesia & Analgesia, 2009;108(3): 770–776., https://doi.org/10.1213/ane.0b013e31819029b2
- Webert, Kathryn, and Morris Blajchman. “Transfusion-Related Acute Lung Injury.” Current Opinion in Hematology, 2005;12(6): 480–487., https://doi.org/10.1097/01.moh.0000177829.85904.39
- Semple, John W., et al. “Transfusion-Associated Circulatory Overload and Transfusion-Related Acute Lung Injury.” Blood, 2019;133(17):1840–1853., https://doi.org/10.1182/blood-2018-10-860809
- Tran, Alexandre, et al. “Permissive Hypotension versus Conventional Resuscitation Strategies in Adult Trauma Patients with HEMORRHAGIC SHOCK: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Journal of Trauma and Acute Care Surgery, 2018;84(5): 802–808., https://doi.org/10.1097/ta.0000000000001816
- Mutschler M, Nienaber U, Brockamp T, et al. “A critical reappraisal of the ATLS classification of hypovolaemic shock: does it really reflect clinical reality?” Resuscitation. 2013;84(3):309-13. doi: 10.1016/j.resuscitation.2012.07.012.
- Popovsky MA, Moore SB. “Diagnostic and pathogenetic considerations in transfusion-related acute lung injury.” Transfusion. 1985;25(6):573-7. doi: 10.1046/j.1537-2995.1985.25686071434.x
- Goldman M, Webert KE, Arnold DM, Freedman J, Hannon J, Blajchman MA. “TRALI Consensus Panel. Proceedings of a consensus conference: towards an understanding of TRALI.” Transfus Med Rev. 2005;19(1):2-31. doi: 10.1016/j.tmrv.2004.10.001
- Engelfriet, C.P. and Reesink, H.W. “ Transfusion-related acute lung injury (TRALI).” Vox Sanguinis, 2009;81: 269-270. https://doi.org/10.1046/j.0042-9007.2001.00115_1.x
- Adapted from Division of Healthcare Quality Promotion; Centers for Disease Control and Prevention. The National Healthcare Safety Network Manual: Biovigilance Component 2016. cdc.gov/nhsn/pdfs/biovigilance/bv-hv-protocol-current.pdf.
- Wang CH, Hsieh WH, et al. “Liberal versus restricted fluid resuscitation strategies in trauma patients: a systematic review and meta-analysis of randomized controlled trials and observational studies.” Crit Care Med. 2014;42(4):954–961.
- Carrick MM, Morrison CA, et al. “Intraoperative hypotensive resuscitation for patients undergoing laparotomy or thoracotomy for trauma: Early termination of a randomized prospective clinical trial.” J Trauma Acute Care Surg. 2016;80(6):886–896.
- Morrison CA, Carrick MM, et al. “Hypotensive resuscitation strategy reduces transfusion requirements and severe postoperative coagulopathy in trauma patients with hemorrhagic shock: preliminary results of a randomized controlled trial.” J Trauma. 2011;70(3):652–663.









