Author: Summer Chavez, DO, MPH, MPM (Health Policy Fellow, Georgetown University/Medstar) // Reviewed by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
The Policy Playbook series from Dr. Summer Chavez is back! This post looks at COVID-19.
What is the issue?
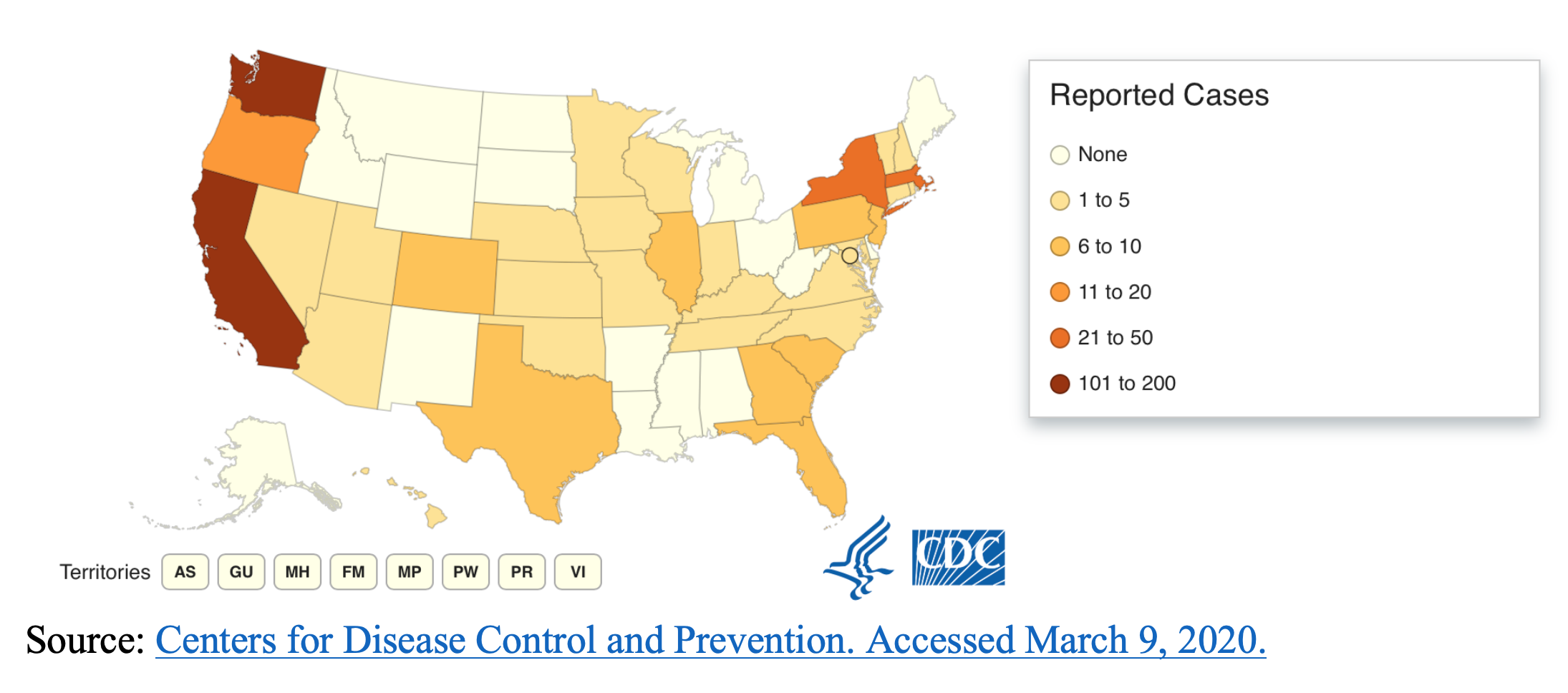
Coronavirus disease (COVID-19) is caused by the SARS-CoV-2 virus, a novel coronavirus first reported in China late December 2019.1 COVID-19 typically presents as a mild viral lower respiratory illness although the elderly and those with comorbidities may be more likely to have poorer outcomes, including death and respiratory failure. 1,2 As of January 31, 2020, the Secretary of Health and Human services declared a public health emergency in response to the COVID-19 outbreak.1 More than 105,000 cases have been reported globally, with approximately 80,000 of these cases in China.3 The number of cases outside of China has been growing, with nearly 25,000 confirmed cases in 101 countries and territories.3 As of March 9, 2020, 423 cases and 19 deaths have been reported in the US amongst 35 states.4 The following figure depicts states with at least 1 COVID-19 case reported to the Centers for Disease Control & Prevention:
Why does this matter?
COVID-19 may become a pandemic with the CDC reporting, “It’s likely that at some point, widespread transmission of COVID-19 in the United States will occur.”1 No vaccine or curative treatment is currently available and confirmatory testing has been limited to date.1,2 In order to meet the increased demand for personal protective equipment (PPE) for healthcare personnel caused by SARS-CoV-2, the World Health Organization recommends a 40% increase in manufacturing to avoid shortages.5 Emergency medicine physicians play integral roles in emergency preparedness and act as safety nets within the healthcare system. Whether it’s seasonal influenza, a mass casualty event, Ebola or resuscitating a septic patient, emergency medicine providers must be able to rise to the occasion.
On March 6, 2020, President Trump signed an $8.3 billion emergency spending bill (H.R. 6074 – Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020) into law.6,7 The bill will allocate funding for public health agencies, vaccine research, medical supplies, testing, small business loan subsidies, emergency preparedness and international humanitarian aid.6 The US government has also instituted an unparalleled travel ban, barring entry for foreign nationals with travel to China or Iran within 14 days and calling for strict monitoring with potential for quarantine for US residents or citizens in contact with certain parts of China.1 Other physicians argue that lifting restrictions on utilizing telehealth for Medicare beneficiaries could be instrumental in public health emergencies by limiting exposure to the community, shifting in-hospital resources to the sickest patients, continuing surveillance and increasing the number of infectious disease specialists.8 While the endpoint is not in sight, a cautious but well-thought out approach is imperative for mitigating the effects of this outbreak and the ones to come in the future.
What can I do about it?
- Practice good hand hygiene. Know how to don and doff PPE.
- Understand your institution’s protocol for identifying patients with potential COVID-19 and preserving or reusing PPE.
- Stay informed about the latest developments as the course of the outbreak progresses.
- Provide education and dispel misinformation about SARS-CoV-2 to your patient population and within your community.
- Consider joining emergency response teams or committees within your organization.
Helpful Resources & Links:
- CDC Coronavirus Disease 2019 (COVID-19) Information for Healthcare Professionals
- World Health Organization Rolling Updates on Coronavirus Disease (COVID-19)
- ACEP COVID-19 (Coronavirus) Clinical Alert
- American Medical Association COVID-19 Resource Center for Physicians
- Novel coronavirus 2019 (COVID-19): Emergence and implications for emergency care (JACEP Article)
References:
- CDC. 2019 Novel Coronavirus (2019-nCoV) Situation Summary. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/summary.html. Published February 11, 2020. Accessed February 18, 2020.
- CDC. Coronavirus Disease 2019 (COVID-19) Evaluating and Reporting Persons Under Investigation (PUI). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html. Published February 11, 2020. Accessed March 4, 2020.
- WHO. Coronavirus disease 2019 (COVID-19) Situation Report – 48. World Health Organization. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200308-sitrep-48-covid-19.pdf?sfvrsn=16f7ccef_4. Published March 8, 2020. Accessed March 9, 2020.
- CDC. Coronavirus Disease 2019 (COVID-19) in the U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html. Published February 11, 2020. Accessed March 4, 2020.
- Shortage of personal protective equipment endangering health workers worldwide. https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide. Accessed March 4, 2020.
- Congressional negotiators reach deal on roughly $8 billion emergency coronavirus spending – The Washington Post. https://www.washingtonpost.com/us-policy/2020/03/04/congress-coronavirus-emergency-spending/. Accessed March 4, 2020.
- Lowey NM. Text – H.R.6074 – 116th Congress (2019-2020): Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020. https://www.congress.gov/bill/116th-congress/house-bill/6074/text. Published March 6, 2020. Accessed March 9, 2020.
- Congress must act to ensure telehealth can be used to combat the coronavirus. Modern Healthcare. https://www.modernhealthcare.com/opinion-editorial/congress-must-act-ensure-telehealth-can-be-used-combat-coronavirus. Published March 2, 2020. Accessed March 4, 2020.









