Authors: Chance Sullivan, MD (Emergency Medicine Resident, University of Vermont); Muhammad Waseem, MD (Department of Emergency Medicine, Lincoln Medical Center, Bronx NY, Clinical Faculty for St. Georges University); Skyler Lentz (@skylerlentz); and Joe Ravera, MD (@pemuvm1, Director of Pediatric Emergency Medicine, UVM Medical Center, Assistant Professor of Surgery, UVM College of Medicine) // Reviewed by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
Case:
A 2-year-old boy is brought in by his mother after 5 days of fever at home as high as 40.6 0C. She had been managing his fever with appropriate doses of acetaminophen, however the mother noticed a large bump on the left side of his neck while putting on his shirt this morning. He has had a decreased appetite over the past two days, with difficulty holding using his utensils due to pain and swelling in both hands.
Upon further questioning, mother notes that everyone in the house had flu-like symptoms a month ago. None of them sought medical care, as their symptoms quickly resolved, including the patient’s. He otherwise has no pertinent medical history, and immunizations are up to date.
Vital signs are within normal limits except for a temperature of 38.2 C. On physical exam, you note a tired moderately ill appearing boy. He has bilateral non-purulent conjunctivitis, clear TM’s bilaterally, and an unremarkable oropharynx. There is a tender 2 cm posterior cervical lymph node. His heart and lung exam were normal. Abdomen soft, non-tender. He has mild dorsal induration on his bilateral hands, but no erythema.
Introduction
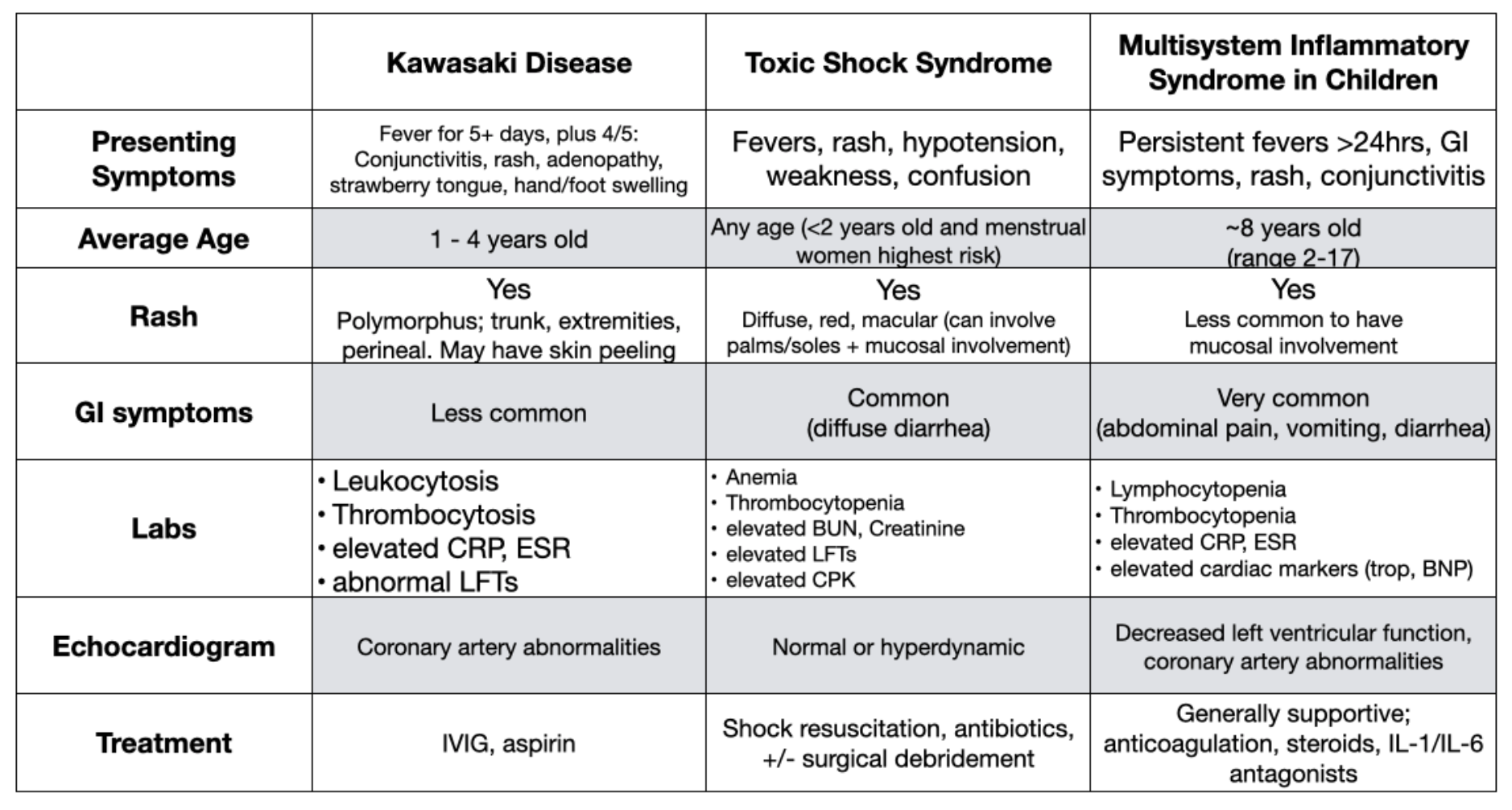
Even before the emergence of novel coronavirus, SARS-CoV-2, the presentation of a moderately to severely ill appearing child with prolonged fever presented a broad differential. The most likely etiology is still a standard of pediatric emergency medicine such as a viral infection,1,2 or common bacterial illness such as pneumonia or urinary tract infection.2 However, with prolonged fever and ill appearance, one should consider immune mediated inflammatory states such as Kawasaki disease or staphylococcal or streptococcal toxic shock syndrome. Further complicating this diagnosis is the emergence of multisystem inflammatory syndrome in children (MIS-C), a diagnosis linked to coronavirus infection.3,4 We present the following review of these three clinical entities.
Kawasaki Disease
This is an acute vasculitis of medium caliber vessels, with the exact etiology being unknown. In general, it is believed to be due to an aberrant response of the immune system to an unidentified pathogen in genetically predisposed children, triggering an immunologic cascade causing the illness.5,6
- Typically self-limited with fever and systemic inflammatory symptoms. However, there are significant complications that may develop, making this an important can’t-miss diagnosis
- Typically affects children 1 – 4 years old, with a higher incidence seen in Japanese descent5,6
- Leading cause of acquired heart disease in patients less than 5 years old.
- Up to 25% of untreated patients develop cardiovascular sequelae, such as coronary artery aneurysms, myocardial ischemia, and myocarditis5-7
- Typically presents with a persistent fever and multiple mucocutaneous findings: diffuse maculopapular rash primarily involving the trunk and extremities, plus dryness and erythema of the lips and tongue5-7
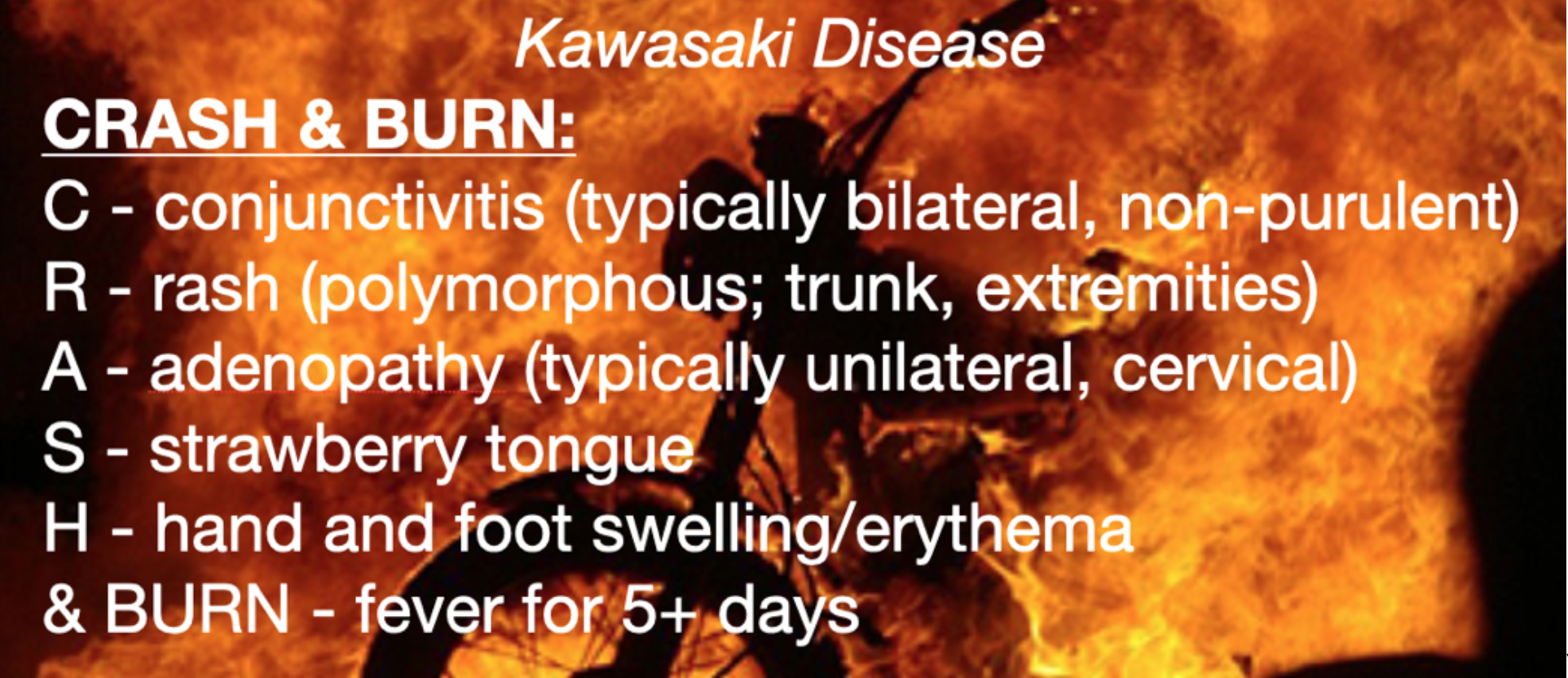
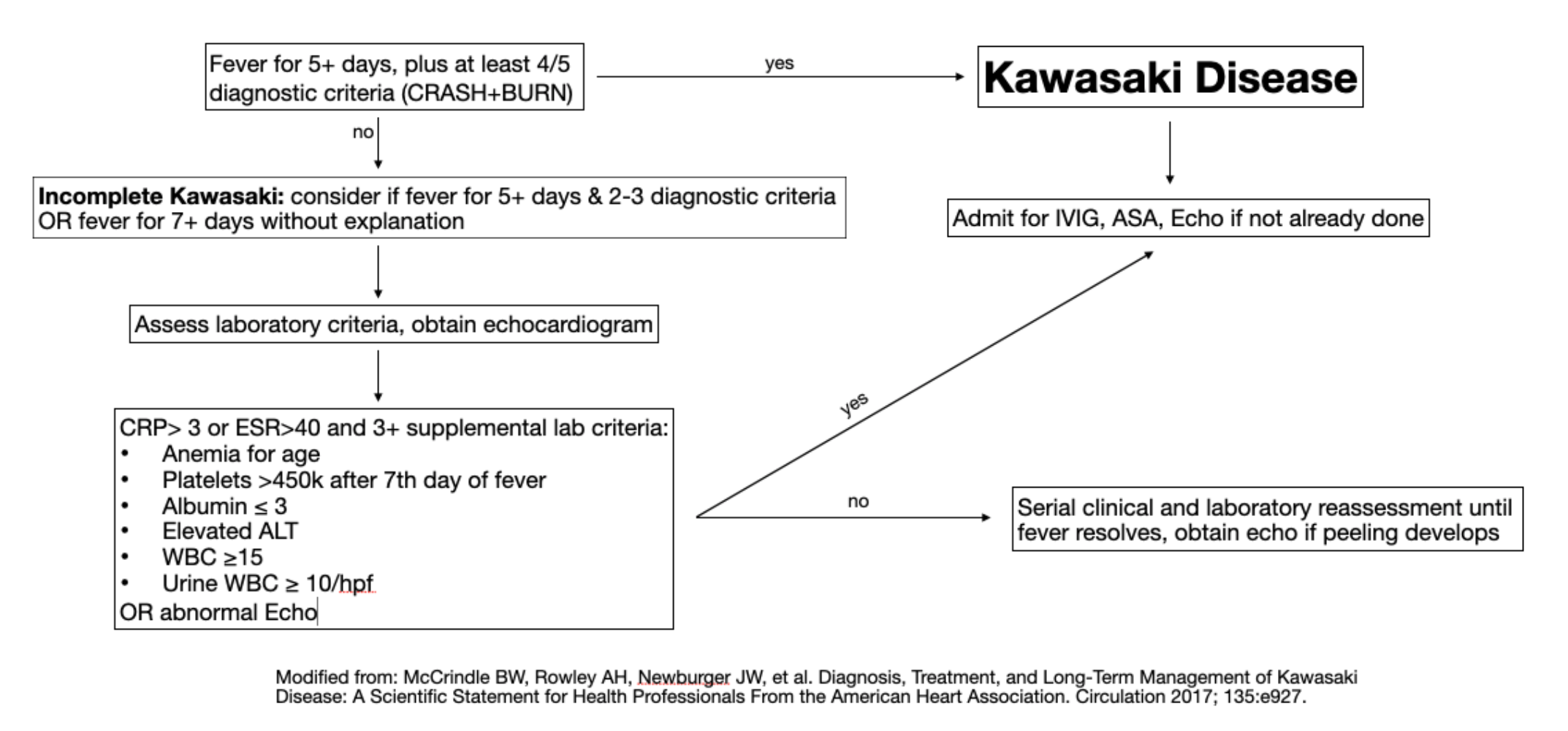
- Diagnostic criteria for complete Kawasaki: fever for 5+ days, plus at least 4 out of the 5 following diagnostic criteria:
- It is important to remember that symptoms can be transient and do not have to all be present at the same time for diagnosis. Therefore, thorough and direct questioning as well as repeated examinations may be necessary to make a timely diagnosis
- Treatment/Disposition: Aspirin, admission for IVIG and echocardiogram7 +/- adjuvant therapy with high dose steroids7,8 or cyclosporin9 particularly in refractory cases or high risk populations
Incomplete presentations of Kawasaki Disease (KD)
- If full diagnostic criteria are not met, then incomplete KD should be considered, as these children are still at risk for cardiovascular sequelae10,11
- High index of suspicion is required, particularly in young children under 6 months, who may present only with fever for 5+ days10,11
- Evaluate with the following laboratory tests:
- CBC with differential
- Serum albumin and ALT
- CRP and/or ESR
- UA
- Elevation of CRP/ESR and 3+ supplemental lab findings indicate treatment with IVIG
- If less than three supplemental laboratory tests are abnormal, echocardiogram is warranted for further evaluation
It is important with KD to maintain a high index of suspicion, as picking out KD from a sea of viral illness is a difficult task. Lack of consideration of the disease is the most common reason for failure to diagnose KD and failure to initiate prompt treatment. If you’re seeing a child with four or five days of constant unrelenting fever, take an extra second and think “Could this be Kawasaki disease?”
Staphylococcal or Streptococcal Toxic Shock Syndrome
Although less common than Kawasaki disease, either staphylococcal or streptococcal toxic shock syndrome can present with findings similar to both KD and MIS-C. The incidence is much lower, as indicated by a review from Victoria, Australia which described only 62 cases over 11 years.12 The etiology is typically immune mediated and associated with an antibody antigen complex from a streptococcal or staphylococcal disease. Similar to KD and MIS-C the diagnosis of toxic shock syndrome based clinical and laboratory studies and the exclusion of other alternative diagnosis like bacterial sepsis.
To meet the criteria of a probable toxic shock syndrome, the following conditions are needed:13
- Fever: temperature greater than or equal to 102.0°F (greater than or equal to 38.9°C)
- Rash: diffuse macular erythroderma
- Hypotension: systolic blood pressure less than or equal to 90 mm Hg for adults or less than fifth percentile by age for children aged less than 16 years
And multisystem involvement from 3 organ systems defined as:
- Gastrointestinal: vomiting or diarrhea at onset of illness
- Muscular: severe myalgia or creatine phosphokinase level at least twice the upper limit of normal
- Mucous membrane: vaginal, oropharyngeal, or conjunctival hyperemia
- Renal: blood urea nitrogen or creatinine at least twice the upper limit of normal for laboratory or urinary sediment with pyuria (greater than or equal to 5 leukocytes per high-power field) in the absence of urinary tract infection
- Hepatic: total bilirubin, alanine aminotransferase enzyme, or aspartate aminotransferase enzyme levels at least twice the upper limit of normal for laboratory
- Hematologic: platelets less than 100,000/mm3
- Central nervous system: disorientation or alterations in consciousness without focal neurologic signs when fever and hypotension are absent
These criteria plus desquamation of the rash after 1 to 2 weeks changes the classification from probable to confirmed.
If you suspect toxic shock, one of the first steps is an exhaustive evaluation for an underlying staphylococcal or streptococcal infection. It is important to consider sources such as the mucous membranes, perineal area, GYN source associated with tampon use or another skin or soft tissue source. In some cases, source control with tampon removal or surgical debridement may be necessary.14
These children will typically present critically ill and require aggressive resuscitation with IV fluids and a large percentage will require vasoactive support with either epinephrine or norepinephrine.14 Early consideration of intubation should also be considered to decrease metabolic demand even in the absence of severe pulmonary pathology.
For targeted antibiotic treatment the patient should receive broad-spectrum antibiotics typically a later generation cephalosporin or penicillin such as cefepime or piperacillin-tazobactam. Vancomycin should also be added for MRSA coverage. Additionally clindamycin is recommended for decreased bacterial toxin production as its mechanism of action is a ribosomal inhibitor.14
Adjuvant therapy with IVIG is controversial and should be discussed with the pediatric critical care and pediatric infectious disease specialist.14
In summary, staphylococcal and streptococcal toxic shock syndromes are rare and in the emergency department we can make a difference with early recognition (particularly those who have a surgical or GYN source), prompt resuscitation and broad-spectrum antibiotic, and transfer to a tertiary care facility.
COVID-19 and MIS-C
Most children and adolescents infected with SARS-CoV-2 (COVID-19) are asymptomatic or develop mild symptoms such as fever and cough.15 Recently, a small number of children, primarily in the UK and New York City, have been identified as developing a significant systemic response termed Multi-system Inflammatory Syndrome in Children (MIS-C).3,4 Limited case reports suggest an older demographic as compared to KD, with an average age around 8 years old and an increased prevalence seen in African descent.16-18
The clinical manifestations of this process are common with other systemic inflammatory conditions, including Kawasaki disease and Toxic Shock Syndrome. Presenting symptoms often include persistent fever, rash, extremity edema, and conjunctivitis. Distinguishing features from KD and TSS include cardiac dysfunction, severe abdominal pain, and relative thrombocytopenia.16-19 The disease can slowly progress over days to weeks after initial recovery from COVID-19 illness, with some patients developing cardiogenic or vasogenic shock requiring ICU admission.
This is an evolving diagnosis and even categorization has been difficult however this is the most recent consensus definition includes a patient less than 21 years old presenting with fever (≥ 100.4° F/38° C); AND all of the following (CDC 2020):
- Laboratory evidence of inflammation
- Elevated CRP, ESR, fibrinogen, procalcitonin, d-dimer, ferritin, LDH, or IL-6
- Elevated neutrophils, reduced lymphocytes, and low albumin
- Multisystem organ involvement
- Cardiac: hypotension, shock, myocarditis/pericarditis
- Rash, however mucosal involvement is less common
- Gastrointestinal symptoms such as diarrhea, vomiting, or abdominal pain
- Renal injury, respiratory failure, or neurologic involvement
- Positive for current or recent SARS-CoV2 infection (PCR or antibody), or COVID-19 exposure within 4 weeks of symptom onset
- Exclusion of other common diagnoses such as sepsis (either bacterial or viral), toxic shock syndrome, etc.
Although the full range of presentations is not fully understood at this time, there is limited data from recent reviews of patients in the United Kingdom and the New York Area. About 90% of these patients presented GI symptoms such as abdominal pain, nausea, vomiting, or diarrhea.18,19
Some of these children but not all had a history of confirmed coronavirus infection via PCR however at time of presentation the viral PCR was typically negative. If available, antibody testing was almost always positive in these patients.18,19
Patients presenting critically ill typically had cardiovascular collapse and shock. Interestingly, despite the patient’s association with coronavirus infection, almost none of the patients had pulmonary disease that was severe enough to require mechanical ventilation, and the common indication for intubation was cardiovascular collapse and circulatory support.18,19
If you do suspect MIS-C, we recommend the following work-up:
Inflammatory Markers
- CBC (neutrophilia, lymphopenia, thrombocytopenia)
- CRP (typically extremely elevated)
- ESR
- Procalcitonin
- Ferritin
- IL-6 (if available)
Coagulation Profile
- Fibrinogen
- PT/PTT
- D-Dimer
Microbiology/Immunology
- SARS-CoV-2 PCR
- COVID antibodies
- Blood culture
Cardiac Function
- Troponin
- BNP
- EKG
- Echocardiogram to evaluate for coronary artery abnormalities
What complications are associated with MIS-C?
The main complications of MISC are cardiovascular. As discussed, a subset of patients present with cardiovascular collapse and a shock-like syndrome requiring vasopressor support. Another complication is cardiac involvement defined by an abnormal echocardiogram with coronary aneurysm, reduced ejection fraction, mitral valve regurgitation or a pericardial effusion.17 Perhaps the most alarming feature of MIS-C was a high prevalence of cardiac involvement at time of presentation. An observational study in Italy demonstrated an increase in the rate of cardiac involvement from a Kawasaki-like disease after the outbreak of the COVID-19 pandemic; the rate was 6/10 cases post-pandemic compared to 2/19 cases pre-pandemic.16 A subsequent review from the UK found that 15% of children presenting with MIS-C already have evidence of coronary artery aneurysms despite a short duration of illness.18 It is not known if the severity of disease correlates with the presence of coronary artery aneurysms, nor if treatment mitigates these complications.
What are the treatment options?
While in the emergency department, supportive care and monitoring are essential. Once the diagnosis is established, work closely with consultants regarding directed therapies. As this illness is still evolving, many treatment options may be experimental. Evidence is limited, especially regarding the benefit in children. Treatments have included anticoagulation, IV immunoglobulin, corticosteroids, and IL-1 or IL-6 blockade.18,20,21
Consider the following:
- Enoxaparin
- All hospitalized cases should receive prophylaxis dosing
- If elevated D-Dimer, consider therapeutic dosing
- Consider heparin if child has renal failure or receiving ECMO
- IVIG and aspirin: If patient meets criteria of Kawasaki disease (complete or incomplete)
- Steroids: in patients with shock; avoid if PCR is positive
- Remdesivir: anti-viral agent for patients with positive SARS-CoV-2 PCR
- Antibiotics: empirically, if unable to rule out serious bacterial infection
- Anakinra: IL-1 receptor antagonist; considered if there is a significantly elevated IL-1
- Tocilizumab: IL-6 receptor antagonist; currently experimental for treating severe COVID-19 pneumonia
Case Conclusion:
The child did not appear critically ill, so toxic shock was considered unlikely. The child had full laboratory studies for evaluation of KD and MIS-C. The only severe abnormality was a highly elevated CRP at 180 mg/L, but all other labs were unremarkable. The child was admitted to the hospital for a full work-up and evaluation of KD and MIS-C. The child’s echocardiogram and cardiac biomarkers were normal. The pediatrics team felt this was more consistent with a prolonged viral illness and not KD or MIS-C. Unfortunately, antibody studies for coronavirus were not available at the time of this child’s admission.
This case highlights that a prolonged viral illness is still the most common reason to see a child with prolonged fever; however, these serious immune mediated complications must be considered, as they are can’t miss diagnoses.
Take-Home Points:
- Children with prolonged fever and multi-system symptoms should be approached with caution, as timely recognition and prompt management can significantly reduce the risk of poor outcomes.
- Kawasaki Disease
- Consider Kawasaki Disease in any child with prolonged fever (5+) days.
- Incomplete Kawasaki Disease represents 15-20% of cases but may still have dangerous sequelae.
- Transthoracic echocardiogram is essential for identification cardiovascular sequelae such as coronary artery aneurysm.
- Treatment with IVIG reduces the likelihood of coronary artery lesions from 25% to 5%.
- Toxic Shock Syndrome
- Maintain a high index of suspicion particularly in a critically ill child.
- In addition to antibiotics, consider source control with either tampon removal or surgical debridement.
- Multi-system Inflammation Syndrome in Children
- MIS-C may occur in children previously infected with COVID-19, and results in persistent fevers and a pronounced systemic inflammatory response.
- Early recognition and specialty consultations are important, including critical care if warranted.
- Treatment is generally supportive and echocardiogram is often warranted.
References/Further Reading:
- Hara M, Takao S. Five-year Study of Viral Etiology and Features of Febrile Respiratory Tract Infections With Prolonged Fever in Japanese Pediatric Outpatients. Pediatr Infect Dis J. 2017;36(12):e358-e360.
- Cho CY, Lai CC, Lee ML, et al. Clinical analysis of fever of unknown origin in children: A 10-year experience in a northern Taiwan medical center. J Microbiol Immunol Infect. 2017;50(1):40-45.
- Royal College of Paediatrics and Child Health. Guidance: Paediatric multi-systemic inflammatory syndrome temporally associated with COVID-19”. 2020
- CDC Health Alert Network. Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). 2020
- Burns JC, Kushner HI, Bastian JF, et al. Kawasaki disease: A brief history. Pediatrics. 2000;106(2):E27.
- Burns, J. C. and M. P. Glodé. Kawasaki syndrome. Lancet. 2004;364(9433): 533-544.
- McCrindle, B. W., et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. Circulation. 2017;135(17): e927-e999.
- Kobayashi T, Saji T, Otani T, et al. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet. 2012;379(9826):1613-1620.
- Aoyagi R, Hamada H, Sato Y, et al. Study protocol for a phase III multicentre, randomised, open-label, blinded-end point trial to evaluate the efficacy and safety of immunoglobulin plus cyclosporin A in patients with severe Kawasaki disease (KAICA Trial). BMJ Open. 2015;5(12):e009562
- Minich LL, Sleeper LA, Atz AM, et al. Delayed diagnosis of Kawasaki disease: what are the risk factors?. Pediatrics. 2007;120(6):e1434-e1440.
- Cimaz, R. and R. Sundel. Atypical and incomplete Kawasaki disease. Best Practice & Research Clinical Rheumatology 2009;23(5): 689-697.
- Chen KY, Cheung M, Burgner DP, Curtis. Toxic shock syndrome in Australian children. N.Arch Dis Child. 2016;101(8):736-40.
- CDC guidelines on the diagnosis of toxic shock. 2010
- Wilkins AL, Steer AC, Smeesters PR, Curtis N. Toxic shock syndrome – the seven Rs of management and treatment. J Infect. 2017;74 Suppl 1:S147-S152
- Zimmermann, P. and N. Curtis. Coronavirus Infections in Children Including COVID-19: An Overview of the Epidemiology, Clinical Features, Diagnosis, Treatment and Prevention Options in Children. The Pediatric infectious disease journal. 2020;39(5): 355-368.
- Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395(10239):1771-1778.
- Toubiana J, Poirault C, Corsia A, et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. 2020;369:m2094.
- Whittaker E, Bamford A, Kenny J, et al. Clinical Characteristics of 58 Children With a Pediatric Inflammatory Multisystem Syndrome Temporally Associated With SARS-CoV-2. JAMA. 2020;e2010369.
- Cheung EW, Zachariah P, Gorelik M, et al. Multisystem Inflammatory Syndrome Related to COVID-19 in Previously Healthy Children and Adolescents in New York City.JAMA. 2020;e2010374.
- Chiotos K, Bassiri H, Behrens EM, et al. Multisystem Inflammatory Syndrome in Children during the COVID-19 pandemic: a case series. J Pediatric Infect Dis Soc. 2020;piaa069
- Balasubramanian S, Rao NM, Goenka A, Roderick M, Ramanan AV. Coronavirus Disease 2019 (COVID-19) in Children – What We Know So Far and What We Do Not. Indian Pediatr. 2020;57(5):435-442.









1 thought on “Prolonged Pediatric Fever and Evaluating Patients for Kawasaki Disease, Toxic Shock Syndrome, and Multi-inflammatory Syndrome of Children”
Pingback: Multisystem Inflammatory Syndrome (MIS-C) & Kawasaki Disease – similarities and differences | Pediatric Focus