Originally published on Ultrasound G.E.L. on 2/28/18 – Visit HERE to listen to accompanying PODCAST! Reposted with permission.
Follow Dr. Michael Prats, MD (@PratsEM), Dr. Creagh Bougler, MD (@CreaghB), and Dr. Jacob Avila, MD (@UltrasoundMD) from Ultrasound G.E.L. team!
Point-of-Care Ultrasound Could Streamline the Emergency Department Workflow of Clinically Nonspecific Intussusception
Pediatric Emergency Care September 2017 – Pubmed Link
Take Home Points
1. This study provides some weak evidence that POCUS can potentially decrease length of stay and radiology referrals in pediatric ED patients with suspected intussusception.
2. This strategy may not be effective unless you discharge after negative POCUS study. This practice is of unclear safety as the sensitivity of POCUS for intussusception is not well established.
Background
Intussusception is the most common cause of intestinal obstruction in toddlers. Less than 30% have the (complete) classic triad of colicky abdominal pain, currant-jelly stool, vomiting/”sausage-like mass”. Ultrasound is the diagnostic modality of choice. Case reports and single site studies support the use of POCUS to evaluate for intussusception (no rigorous studies at this time). There is some concern that there may be unnecessary referrals for radiologist performed ultrasounds – they cite 85.9% negative US in one study. Although negative studies don’t mean that it wasn’t the right thing to do, perhaps the yield can be improved if there was a screening exam with POCUS. The point of this study is to see if implementing a POCUS protocol helps improve the work flow in the emergency department.
Questions
Does the implementation of a POCUS protocol in patients with clinically nonspecific intussusception (CNI) affect:
- ED length of stay (EDLOS)
- Percentage of negative referrals to radiology for intussusception ultrasounds
Population
- Single institution in Seoul, Korea
- Tertiary-care, university hospital
- ED patients only → see approx. 35K children annually
- Three teaching hospitals affiliated with this university → the largest of these has 2700 beds!
Inclusion:
- age 6 and younger, diagnosed between may 2012 and April 2016
- Must have had Clinically Nonspecific Intussusception (CNI)* + positive US, treated by pneumatic reduction
This is an important point. To backtrack a little, classic presentation of intussusception is the triad of abdominal pain, currant-jelly stool, and vomiting or a ”sausage-like mass”. There is discrepancy which symptom is actually the third part of the triad – vomiting or the mass. I looked at multiple sources, and it seems that most favor vomiting as the third symptom; however, this study used the mass as the third aspect of the triad. With that said, this study included both as one of the symptoms they look at so it all comes out in the wash. So they defined Clinically Non-specific Intussusception (which it seems they made up) as a patient presenting with only one manifestation out of these three symptoms: pain/irritability, mass, bloody stool, AND/OR vomiting. This means that patients with both pain and vomiting, for example, could be included, but if they had pain and bloody stool, they were excluded from the study. They were trying to rule out the disease in a lower prevalence population.
Exclusion:
- Not non-specific intussusception (more than 1 symptom of triad)
- Transfers with the diagnosis already
- Hx of intussusception (second visits were not counted twice)
- Surgery treatment
- CT performed
- Left against medical advice
Design
Retrospective cohort study. Before and after design.
Reviewed all cases of children 6yo and younger given dx of intussusception from May 2012 through April 2016
Setting:
- Since 2000, 24-hour availability of radiology performed ultrasound with air enema reduction has been standard of care
- If procedure successful, patients are monitored in ED for 6-12 hours then discharged if well-appearing and tolerating PO
- Patients go to surgery if had symptoms > 48 hours, evidence of bowel perforation, 2+ failed attempts at reduction by air enema
- May 2012-April 2014 (POCUS only occasionally performed) – PRE group
- May 2014-April 2016 (POCUS protocol initiated)
Data Collection:
All children with CNI confirmed by radiology US and treated by air enema over study period were included. Lots of data collected → all of these data were reasonable, although unclear utility of labs as these labs are not routinely performed for the evaluation of intussusception.
Regarding ultrasound findings, they noted:
o Location of lesion
o Lead points (<10% in kids have this)
o Thickness of involved bowel >10mm
o Number of involved lymph nodes ≥ 2
o Trapped fluid
Some of these (thickness ≥ 10 mm, ≥2 involved lymph nodes, and trapped fluid) are thought to predict irreducibility.
Also looked at variables regarding disease severity, recurrence within 48 hours, admission, surgery, death.
Recorded frequency of POCUS performance and positive US results.
Time intervals: measured by time stamps and compared between PRE- and POST- groups. EDLOS = sum of door-to-reduction and observation times. Door-to-reduction = door-to-US time (time from ED arrival to US dx) + US-to-reduction time (time from US to successful air enema). Observation time = time from successful reduction to discharge.
Intervention
Pre-intervention group (PRE) = May 2012 through April 2014. One pediatric emegency medicine (PEM) attending and multiple pediatricians. The PEM attending in the group occasionally did POCUS for intussusception.
Post-intervention group (POST) = May 2014 through April 2016. Now 5 PEM attendings. POCUS protocol implemented.
Study POCUS Protocol:
- Performed POCUS within 1 hour of presentation
- Positive study defined as target sign or pseudo-kidney sign
- If positive, they were sent to radiology for confirmation and treatment with air enema
- If negative, they were discharged unless there was high suspicion
- If POCUS not performed, they received comprehensive radiologist US
Who did the ultrasounds?
PEM attendings who received a 4-hour training course (hands-on and didactics)
The Scan
Small curvilinear and linear probes used

Positive scan = “target sign” or “pseudo-kidney” sign.
No detail provided regarding scanning protocol.
Short video describing ultrasound intussusception findings
Intussusception on Ultrasound Podcast Part 1 and Part 2
Here is one more video about POCUS for intussusception by Society of Academic Emergency Medicine]
Results
The Patients
With 114 exclusions, study population down to 160. N = 160. PRE group = 67, POST group = 93.
- No significant age, clinical, vital signs, or lab abnormalities between Pre and Post groups
- Thickness of bowel > 10 mm was more common in PRE- vs. POST- group
- median age 19 months
- median symptoms 8 hrs
- pain/irritability in 81%, vomiting in 45%, 0 with mass, 6% with blood stool
Exclusions:
- ≥ 2 classic symptoms: n=50
- Transfer with diagnosis: n=25
- History of intussusception: n=13
- Treated by surgery: n=13 (11 surgical reductions, 1 surgical reduction with transverse colon wedge resection, 1 right hemicolectomy)
- Confirmation by CT: n=10
- Discharge AMA: n=3
Primary Outcomes
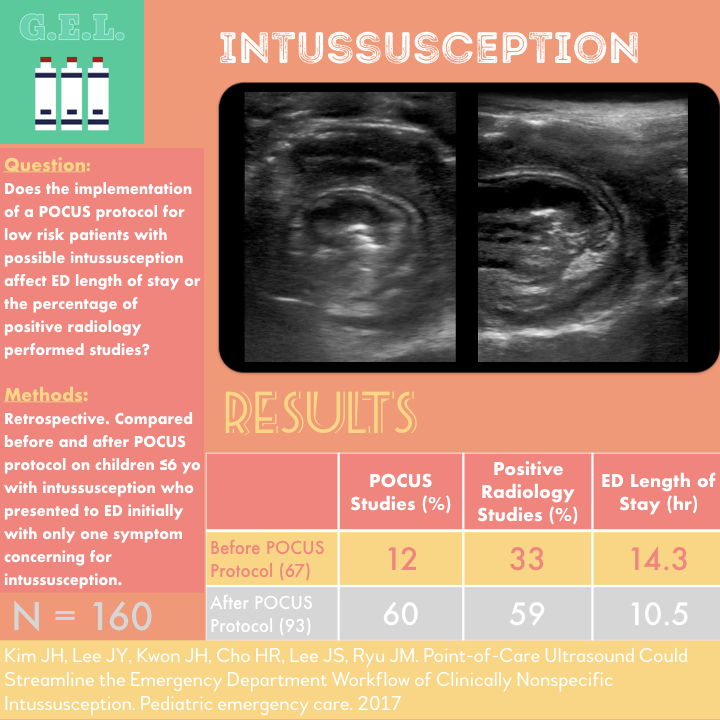
1 More POCUS performed in POST group
PRE 12%
POST 60%
Makes sense, this is after the POCUS protocol was instituted.
2 Much higher rate of radiology US positive for intussusception in POST group
PRE 33%
POST 59%
This is what they expected, more radiologist US are positive because the screening POCUS has taken out those unlikely to have disease.
3 POST group had shorter median ED LOS
PRE 14.26 hrs
POST 10.5 hrs
Door to reduction time (137 min vs 111 min), and observation times (11.66 hours vs 8.86 hours) also improved. Note – on all of these time comparisons the confidence intervals between groups overlapped.
Other Findings
100% specificity – all positive POCUS studies were confirmed on radiologist ultrasound.
No difference between groups with regard to recurrence, admission, or surgery.
Of the 56 children that had POCUS scans, 55 were positive with radiology confirmed US and air enema.
There was 1 false negative study that is mentioned. After having a negative study, she developed further symptoms during observation and underwent subsequent radiology performed study which was positive.
They did not find any follow visits or returns on patients discharged with negative POCUS study.
Limitations and Discussion
External validity limited as this was a single center, outside of the US.
Are these changes/improvements really due to POCUS? That’s the problem with PRE and POST studies in general. There were significant differences in rates of intussusception between the two groups that could affect outcomes. Another variable is that they went from 1 to 5 attendings! Also,can the improvements seen really due to POCUS when only 60% of patients in POST- group got a POCUS scan?
Most of the improvement in LOS time seemed to come from the decrease in observation time. They do not mention why this was but state that it could have been due to recent studies suggesting a shorter observation time might be safe.
Did they miss any with POCUS? At least 1. Because this was retrospective, they could not follow up on the patients that were discharged after negative POCUS. There were no return visits noted but that only goes so far. They quote a prior study with sensitivity of 85% → their recommendation is for observation after a negative POCUS.
Overlapping confidence intervals in the comparison of time intervals results cast doubt on the significance of the difference.
The fact that the PRE group had more patients with thickened bowel wall brings up the possibility that the PRE group could have been sicker. If this is true but but there were no difference in outcomes, would pre-group have better outcomes if patients were equally ill? Alternately, this could be explained by longer times to time to US in the PRE group.
Despite better times to diagnostics – no difference in mortality, recurrence, or the need for surgery. So it seems it may help the emergency department more than it helps the patient (although certainly length of stay time may be important to patients).
Take Home Points
1. This study provides some weak evidence that POCUS can potentially decrease length of stay and radiology referrals in pediatric ED patients with suspected intussusception.
2. This strategy may not be effective unless you discharge after negative POCUS study. This practice is of unclear safety as the sensitivity of POCUS for intussusception is not well established.
Our score