Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. Today we look at the CENSER trial.

Authors: Mackenzie Prendergast, DO (EM Resident Physician, San Antonio, TX); Brannon L Inman, MD (Critical Care Fellow, Orlando, FL) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Early Use of Norepinephrine in Septic Shock Resuscitation: A Randomized Trial
AKA the CENSER Trial
Clinical question:
In patients with suspected infection and hypotension (MAP < 65 mm Hg), does early use of norepinephrine in septic shock resuscitation improve the efficacy of shock control?
Study design
- Single center, randomized, double-blinded, placebo-controlled clinical trial
- Phase II RCT
- Outcome evaluation, data management, and analysis were performed by PI and statistician, both of whom were blinded to the patient enrollment and treatment process
PICO
Population
- Patients recruited from the Department of Medicine, Faculty of Medicine, Siriraj Hospital in Bangkok, Thailand from October 2013 to March 2017
- This is the largest university-based national tertiary referral center in Thailand

- 310 adults with sepsis with hypotension in final count
- 320 initially met criteria and underwent randomization, 10 withdrew consent
- Inclusion criteria:
- Adults 18 and older presenting to the ED with hypotension and suspected infection
- Hypotension defined as MAP <65mmHg
- Were required to meet the diagnostic criteria for sepsis according to the 2012 Surviving Sepsis Campaign
- Must meet criteria for less than 1 hour prior to randomization
- Adults 18 and older presenting to the ED with hypotension and suspected infection
- Exclusion criteria:
- Patients who:
- Met septic shock criteria >1 hour prior to randomization
- Acute CVA
- ACS
- Acute Pulmonary Edema
- Status asthmaticus
- Active GI hemorrhage
- Pregnancy
- Seizure
- Drug overdose
- Burn injury
- Trauma
- Need for immediate surgery
- Advanced stage cancer
- Signed to refuse medical treatment, including intubation, fluid resuscitation, vasopressor use
- Patients were randomly assigned 1:1 based on sequential number of enrollment
- Patients who:
- Groups were even in terms of division for age/gender/comorbidities/source of infection
- Treatment group did have more patients with culture + Gram neg bacilli
Intervention
- 4 mg NE mixed with 250 mL 5% dextrose in water (D5W) for a final concentration of 16mcg/mL infused at a constant non-titrated rate of 0.05 mcg/kg/min for 24 hours
Comparison
- Placebo = 250 mL D5W infused at an equal, constant non-titrated rate of 0.05mcg/kg/min for 24 hours
Outcome
- Measured primary outcome: shock control rate by 6 hours after diagnosis of sepsis with hypotension
- Shock control rate defined as: sustained MAP > 65 mmHg + evidence of adequate tissue perfusion
- Sustained MAP defined as: MAP > 65mmHg for two consecutive measurements 15 minutes apart
- Adequate tissue perfusion defined as:
- Continuation of UOP > 0.5 mL/kg/hr for 2 consecutive hours OR
- Decrease in serum lactate by more than 10% from initial level
- Shock control rate defined as: sustained MAP > 65 mmHg + evidence of adequate tissue perfusion
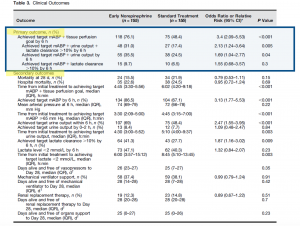
- Primary outcome – Early norepinephrine group vs. the control group demonstrated higher rates of shock control at 6 hours: 76.1% vs 48.4% (OR 3.4, 95% CI 2.09-5.53)
Takeaways:
- Positive trial => there was a statistically significant rate of shock control attained with the treatment arm.
- They used a fixed dose of NE rather than titratable amount, which is not how we would typically utilize this treatment.
- There was no significant difference in median time to initiation of use of open label NE between groups. Additionally, 80% of patients in the control group required open label NE use indicating that NE was going to be needed in most of these patients regardless of initial resuscitation method.
- 55.5% of the patients received vasopressors through a peripheral IV. There was no difference in skin necrosis or limb ischemia between groups.
- The median amount of fluids administered between the groups before initiation of NE was not statistically significant (2080 mL vs. 1900 mL).
- The study was performed when Surviving Sepsis Campaign Guidelines were used, so it was more common to see large volume fluid administration in the setting of sepsis. Authors also did not control for volume of fluid administered.
- External validation is limited as the primary study occurred in a resource-limited country as a single center only trial, would like to see this in a multicenter setting.
- Unfortunately, a surrogate endpoint was used as the primary outcome (shock control), and patient centered outcomes like mortality were secondary outcomes.
My Take:
- This is the first RCT for this type of intervention. It certainly opens the door for other, larger/more widespread trials to take place and is a good stepping stone for improving on previous doctrine of fluids, fluids, fluids in the setting of septic shock.
- I will continue to reach for pressors early in resuscitation of the septic shock patient.
Reference:
- Permpikul C, Tongyoo S, Viarasilpa T, Trainarongsakul T, Chakorn T, Udompanturak S. Early Use of Norepinephrine in Septic Shock Resuscitation (CENSER). A Randomized Trial. Am J Respir Crit Care Med. 2019;199(9):1097-1105. doi:10.1164/rccm.201806-1034OC








