Authors: Matthew Christensen, MD (EM Resident, Naval Medical Center San Diego, CA) and Kristy Schwartz, MD, MPH, FACEP (@kaynani32, Asst Clinical Professor of Pediatrics and Emergency Medicine, University of California San Diego and Rady Children’s Hospital San Diego, CA)// Reviewed by: Jamie Santistevan, MD (@jamie_rae_EMdoc, EM Physician, Presbyterian Hospital, Albuquerque, NM); Manpreet Singh, MD (@MPrizzleER); and Brit Long, MD (@long_brit)

Introduction
Syncope is a relatively common chief complaint in the emergency department, with a broad differential that ranges from reassuringly benign to acutely life-threatening.1 While there is no substitute for a thorough history and physical exam, obtaining an electrocardiogram (ECG) is a key aspect of nearly every syncope workup.1 Prompt recognition of high-risk ECG patterns is a critical skill for emergency medicine attendings, residents, and medical students alike. Here we introduce the mnemonic “ABCDE Left Right”, a memory aid to help EM providers quickly recall seven ECG patterns of high-risk syncope: AV block, Brugada pattern, QTc prolongation, delta waves (Wolff-Parkinson-White), epsilon waves (arrhythmogenic right ventricular cardiomyopathy), left ventricular hypertrophy, and right ventricular strain.
For a refresher on the broader approach to syncope in the emergency department and take a closer look at non-cardiac causes of syncope, see the emDocs article Syncope and Syncope Mimics.
A – Atrioventricular (AV) Block
Learning to recognize the ECG changes of first, second, and third degree AV block is a fundamental skill in emergency medicine. Prolongation of the PR interval (greater than 200 milliseconds) defines first degree AV block.
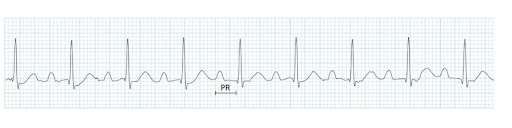
Example of first degree AV block. Image obtained from https://litfl.com/first-degree-heart-block-ecg-library/
Second degree AV block is characterized by a dropped QRS complex following a P wave with normal morphology; second degree Mobitz type I (Wenckebach) can be diagnosed when the dropped QRS is preceded by progressively lengthening PR intervals, while second degree Mobitz type II is diagnosed when the dropped QRS is preceded by beats with a fixed PR interval.
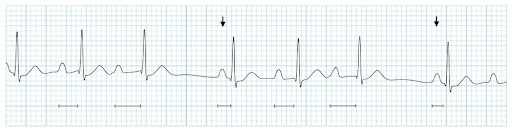
Example of second degree Mobitz type I (Wenckebach) AV block. Image obtained from https://litfl.com/av-block-2nd-degree-mobitz-i-wenckebach-phenomenon/

Example of second degree Mobitz type II AV block. Image obtained from https://litfl.com/av-block-2nd-degree-mobitz-ii-hay-block/
The hallmark of third degree AV block is complete atrial-ventricular dissociation.

Example of third degree AV block. Image obtained from https://litfl.com/av-block-3rd-degree-complete-heart-block/
For a deeper dive, see the emDocs article series ECG Pointers: AV Blocks – Part I and ECG Pointers: AV Blocks – Part II.
B – Brugada Pattern
The Brugada pattern is caused by a genetic mutation in the sodium channel of cardiac myocytes.2 This causes a characteristic “coved” (type I) or “saddleback” (type II) appearance of the ST segment, typically in leads V1 and/or V2.2 Family history of sudden cardiac death should raise suspicion for this diagnosis. For a deeper dive, see the emDocs article ECG Pointers: Syncope and Brugada Syndrome.

ECG changes characteristic of Brugada type I and type II. Image obtained from https://litfl.com/brugada-syndrome-ecg-library/
C – QTc prolongation
The QT interval is measured from the beginning of the QRS complex to the end of the T wave, and is classically measured in lead II or V5/V6.3 The corrected QT (QTc) interval represents the QT interval as adjusted for a heart rate of 60 beats per minute.4 QTc prolongation can be caused by a number of pathologies, including electrolyte derangements (i.e., hypokalemia, hypomagnesemia, hypocalcemia), increased intracranial pressure, medication-induced (antipsychotics, antidepressants, and antiarrhythmics are common culprits), or congenital, as in the case of Long QT syndrome.3 The QT interval is considered prolonged if it measures greater than 440 milliseconds in males or greater than 460 milliseconds in females.3 The QT interval can be grossly estimated as normal if it measures less than half the length of the preceding RR interval.3, 4

Example of QTc prolongation in congenital Long QT syndrome. Image obtained from https://litfl.com/qt-interval-ecg-library/
D – Delta Waves
Delta waves are the pathognomonic shortened PR interval with slurred QRS upstroke characteristic of Wolff-Parkinson-White (WPW).5 These ECG changes are caused by electrical conduction along an accessory pathway between atrial and ventricular myocytes that bypasses the atrioventricular node.5 When present, delta waves can be seen in limb leads and/or precordial leads. For a deeper dive, see the emDocs article ECG Pointers: Syncope and Wolff-Parkinson-White.

Delta waves characteristic of WPW. Image obtained from https://litfl.com/delta-wave-ecg-library/
E – Epsilon Waves
Epsilon waves are the characteristic inflection point seen between the QRS and the ST segment that classically represents arrhythmogenic right ventricular cardiomyopathy (ARVC), also called arrhythmogenic right ventricular dysplasia (ARVD).6 When present, the epsilon wave is typically most prominent in precordial leads V1 and/or V2. In patients with ARVC, cardiac myocytes become replaced with fat and fibrous tissue, causing conduction impairment that manifests as the epsilon wave.6 For a deeper dive, see the emDocs article ECG Pointers: Syncope and Arrhythmogenic Right Ventricular Cardiomyopathy.
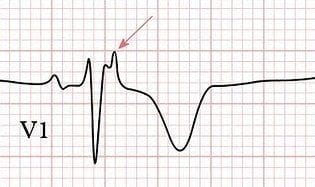
Epsilon wave. Image obtained from https://litfl.com/epsilon-wave-ecg-library/
Left – Left Ventricular Hypertrophy
ECG evidence of left ventricular hypertrophy (LVH) after a syncopal episode raises concern for impaired cardiac outflow, which may represent underlying hypertrophic cardiomyopathy (HCM), aortic stenosis, aortic coarctation, aortic regurgitation, or mitral regurgitation in the appropriate clinical context.7 Many different voltage criteria can be used to diagnose LVH, however the Sokolov-Lyon criteria (the sum of the deepest S wave depth in lead V1 or V2 plus the tallest R wave in either V5 or V6 is greater than 35 mm) is one of the most widely accepted.7 For a deeper dive on HCM, see the emDocs article ECG Pointers: Syncope and HCM.

LVH by the Sokolov-Lyon criteria. Image obtained from https://litfl.com/left-ventricular-hypertrophy-lvh-ecg-library/ .
Right – Right Ventricular Strain
Key ECG findings of right heart strain are ST segment depressions and T wave inversions in the right-sided precordial leads V1-V4 and/or inferior limb leads II, III, aVF, typically accompanied by right axis deviation and/or a dominant R wave in V1.8, 9 ECG evidence of right ventricular strain after a syncopal episode raises concern for pulmonary embolism.8 The classic SIQIIITIII pattern often tested on license exams is unfortunately neither sensitive nor specific for pulmonary embolism8, and EM providers must be on the lookout for evidence of right heart strain in the right clinical context as well. For a deeper dive on pulmonary embolism including its potential ECG changes, see the emDocs article Pulmonary embolism: Why do we miss it, and how do we get better?.

Example of right ventricular strain on ECG. Image obtained from https://litfl.com/right-ventricular-strain-ecg-library/
Main ECG Pointers:
- Learning to recognize key ECG patterns of high-risk syncope is a critical skill in emergency medicine. Memory aids are a valuable tool to recall important information under otherwise tense or stressful circumstances.
- The “ABCDE Left Right” mnemonic can be used to highlight seven can’t-miss patterns of high-risk syncope that emergency medicine providers of any training level must be able to promptly recognize and manage.
- AV block
- Brugada pattern
- QTc prolongation
- Delta waves (Wolff-Parkinson-White)
- Epsilon waves (arrhythmogenic right ventricular cardiomyopathy)
- Left ventricular hypertrophy
- Right ventricular strain.
- For a refresher on the broader approach to syncope in the emergency department and take a closer look at non-cardiac causes of syncope, see the emDocs article Syncope and Syncope Mimics.
References
- Quinn J, D’Souza P. Approach to Syncope. EM:RAP CorePendium. Published July 15, 2021. Accessed August 06, 2022. https://www.emrap.org/corependium/chapter/recn9iTEoblED2hWk/Syncope
- Brugada J, Brugada R, Brugada P. Right bundle branch block and ST segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998; 97:457–460.
- Burns E, Buttner R. QT Interval. Life in the Fast Lane ECG Library. Published online May 14, 2022. Accessed August 07, 2022. https://litfl.com/qt-interval-ecg-library/
- Grohmann A, Eggeman D, et al. QT Prolongation. WikEM. Page last updated May 2022. Accessed August 07, 2022. https://wikem.org/wiki/QT_prolongation
- Cadogan M, Buttner R. Delta Wave. Life in the Fast Lane ECG Library. Published online February 10, 2022. Accessed August 07, 2022. https://litfl.com/delta-wave-ecg-library/
- Cadogan M, Buttner R. Epsilon Wave. Life in the Fast Lane ECG Library. Published online February 04, 2022. Accessed August 07, 2022. https://litfl.com/epsilon-wave-ecg-library/
- Burns E, Buttner R. Left Ventricular Hypertrophy. Life in the Fast Lane ECG Library. Published online April 02, 2021. Accessed August 07, 2022. https://litfl.com/left-ventricular-hypertrophy-lvh-ecg-library/
- Burns E, Buttner R. ECG changes in Pulmonary Embolism. Life in the Fast Lane ECG Library. Published online November 30, 2021. Accessed August 06, 2022. https://litfl.com/ecg-changes-in-pulmonary-embolism/
- Burns E, Buttner R. Right Ventricular Strain. Life in the Fast Lane ECG Library. Published online March 09, 2021. Accessed August 07, 2022. https://litfl.com/right-ventricular-strain-ecg-library/








