Originally published at CoreEM.net, dedicated to bringing Emergency Providers all things core content Emergency Medicine available to anyone, anywhere, anytime. Reposted with permission.
Follow CORE EM on twitter at @Core_EM
Written by Bess Storch, MD and Edited by Tim Greene, MD
Definition: Unstable ipsilateral anterior and posterior fractures of the pelvic ring, with resultant superior displacement of one hemipelvis. Also known as the Malgaigne fracture.
Mechanism
- High energy blunt trauma, with significant axial loading
- Most commonly a fall or jump from a height with impact onto the lower extremities
- Pelvic ring is disrupted, with both anterior pelvis injury (pubic rami), and ipsilateral posterior pelvis injury (sacrum, SI joint, iliac wing)
- Ruptures the sacrotuberous and posterior sacroiliac ligaments which provide vertical stability to the pelvis
- As a result, the “lateral fragment”, the fracture component containing the acetabulum, is displaced superiorly
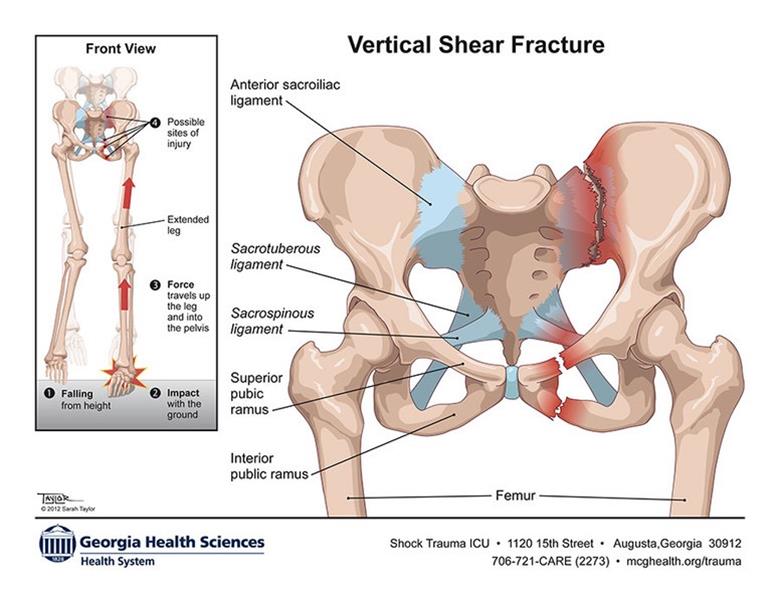
Vertical Shear Fracture Mechanism ( http://www.taylorillustration.com)
Epidemiology
- 5% of all pelvic fractures (Dalal 1989)
- Least common of the three categories of pelvic fractures based on the Young-Burgess Classification System (see “Injury Classification System” below). (Burgess 1990)
- Poor prognosis – overall mortality rate 28% (Dalal 1989)
Physical Exam
- Tenderness on palpation of the pelvis is the most reliable indicator of pelvic ring injury (Durkin 2006)
- Pelvic instability
- Traditional assessment
- Gentle bimanual compression to both iliac wings.
- Should only be performed only once, given risk of disrupting early clot formation and tamponade.
- Poor sensitivity (59%) and specificity (71%) (Scott 2013)
- Vertical instability
- Place one hand on the iliac crest and with the other hand applying traction to the leg
- If there is vertical instability, this maneuver will cause inferior displacement of the leg
- Alternate approach: because of the potential to disrupt clot or worsen bleeding in severely injured trauma patients, it is reasonable to simply place a pelvic binder and obtain imaging instead of applying these maneuvers.
- Traditional assessment
- Assess for limb length discrepancy, with shortening of the lower extremity ipsilateral to the pelvic injury.
- Assess for evidence of surrounding soft tissue injuries:
- Scrotal/labial/perineal/flank hematomarectal /vaginal/perineal lacerationsrectal exam for sphincter tone and sensation to evaluate for lumbosacral plexus injuries
- Gross hematuria for GU injury.
- Thoroughly evaluate for other injuries given the high energy mechanism needed to sustain this type of fracture
Injury Classification System
- Tile System: Divided into three categories based on the stability of the posterior sacroiliac complex
| Type | Stability | Examples |
| A | Stable | Isolated iliac wing fractures, avulsion fractures of the iliac spines or ischial tuberosity, nondisplaced pelvic ring fractures. |
| B | Rotationally unstable; vertically stable | Open book fractures, lateral compression fractures, and bucket-handle fractures. |
| C | Rotationally and vertically unstable | Vertical shear injuries |
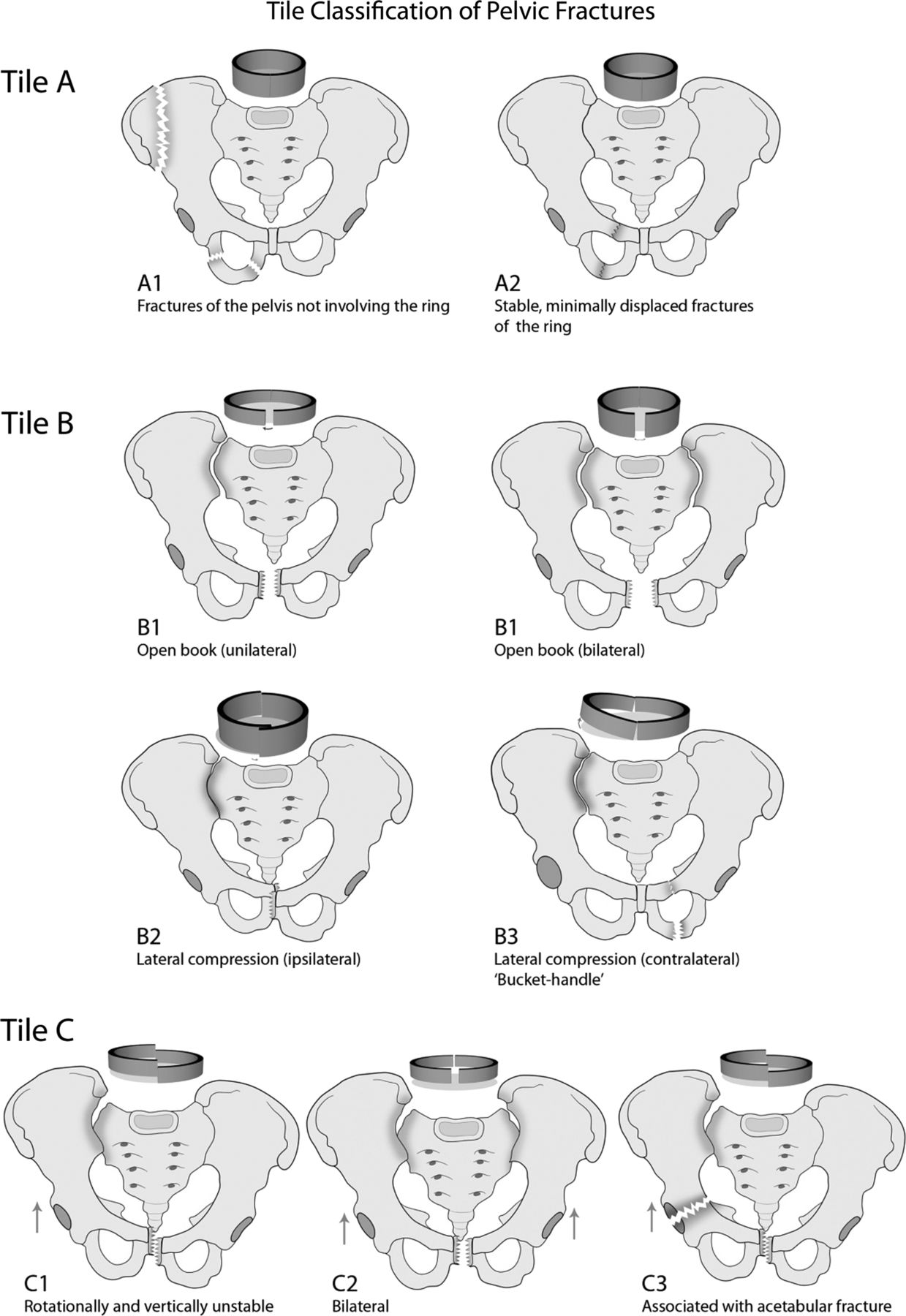
Tile Classification (jramc.bmj.com)
- Young-Burgess system: Based on the direction of force applied to the pelvic ring
| Pattern | Characteristics | Incidence | |
| Lateral compression (LC) | I. Rami fracture and ipsilateral sacral compression. | 48.7% | |
| II. Rami fracture and ipsilateral crescent fracture. | 7.4% | ||
| III. Rami fracture and contralateral APC injury. | 9.3% | ||
| Anterior-posterior compression (APC) | I. Symphysis diastasis <2cm; SI joints intact. | 0% | |
| II. Symphysis diastasis with disruption of the anterior SI ligaments. | 11.1% | ||
| III. Symphysis diastasis with disruption of the anterior and posterior SI ligaments. | 4.3% | ||
| Vertical shear (VS) | Vertical displacement of one or both hemipelvices. | 5.6% | |
| Combined | A combination of the above injuries. | 6.8% | |
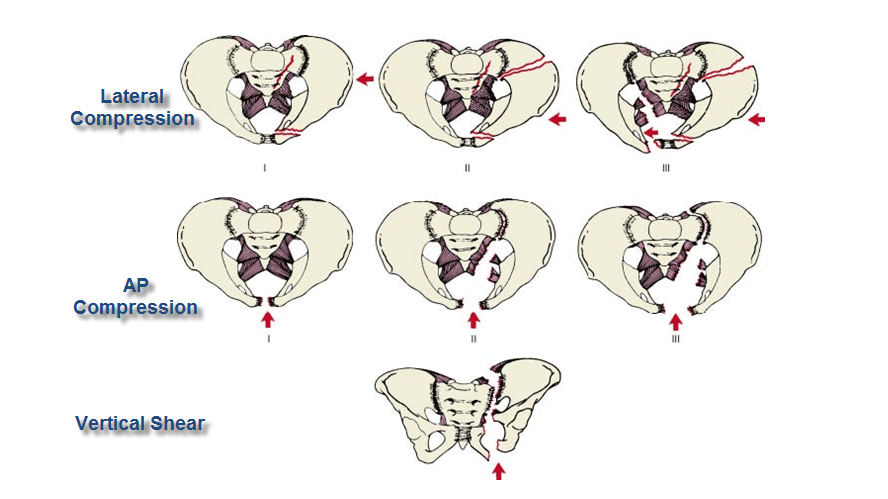
Young-Burgess Classification (boneandspine.com)

Vertical Shear Fracture with Diastasis of the Pubic Symphysis (radiologykey.com)
X-Ray Findings
- Views: Anterior-Posterior (AP) image most commonly obtained
- Diagnostic Findings
- Separation of the pubic symphysis greater than 0.5 cm
- Vertically oriented fractures through components of both the anterior and posterior pelvis
- Results in superior displacement of the lateral “acetabulum-containing” fragment of the pelvis
- Isolated anterior ring injury
- Uncommon in high-energy mechanism
- Pelvis is a ring structure and a single disruption of the ring is uncommon
- If a concomitant posterior injury is not visualized, consider obtaining a CT to further evaluate
- In one study of patients with apparent isolated pubic ramus fractures on X-ray, 96.8% (171/177) had posterior injuries revealed on CT (Scheyerer 2012)
- Additional Images:
- Consider pelvic inlet and outlet views to better demonstrate hemipelvis displacement
- Should only be performed in hemodynamically stable patients

Fracture involving left sacroiliac joint and left pubic rami, with superior displacement of the lateral fragment (www.healio.com/orthopedics/journals/ortho)

Malgaigne Fracture (Case courtesy of Dr Hani Salam, Radiopaedia.org. From the case rID: 12132)
Emergency Department Management
- Early recognition and treatment of hemorrhagic shock is the most important factor for survival. (Halawi 2015)
- 63% prevalence of hemorrhagic shock in these injuries
- Potential for massive retroperitoneal hemorrhage from bony fragments and lacerated blood vessels
- Venous bleeding more common but arterial hemorrhage can also occur
- Retroperitoneal space can accumulate up to 4 liters of blood before venous tamponade occurs
- With only 3 cm of additional pubic symphysis diastasis (separation), the pelvis doubles in volume, allowing for significantly more bleeding before tamponade.
- Emergency Stabilization Approach
- Place pelvic binder
- Focus on trauma resuscitation
-
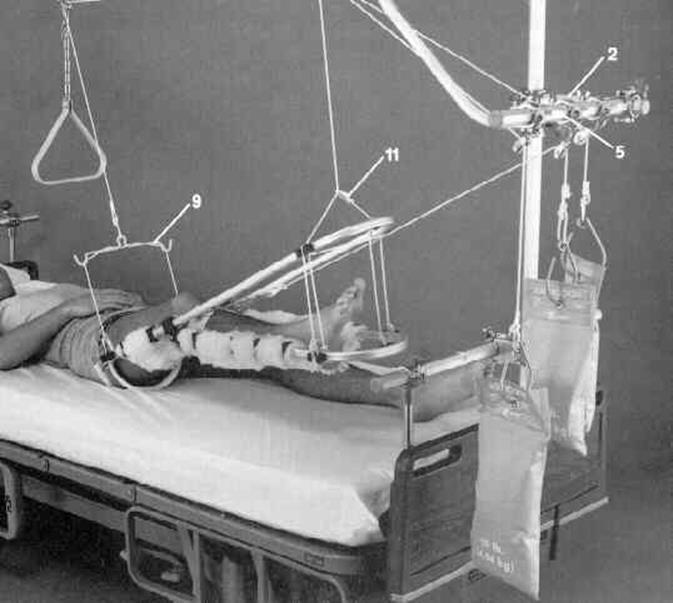
Traction Set Up (wheelessonline.com)
Orthopedic Stabilization Approach
- Goals: Prevent movement of fracture fragments, stabilize pelvis and reduce pelvic volume (Halawi 2015)
- Apply axial traction to vertically align the two pelvic fracture fragments
- Place supracondylar femoral pin into side with migrated fragment
- Apply 25-30 lbs of traction to reduce pelvis
- Attempt to obtain equal leg lengths as indicator of alignment
- After traction accomplished, apply pelvic binder or bedsheet
- Continued management depends on other traumatic injuries and priorities but may include external fixation, angiography with embolization, laparotomy with pelvic packing. Consult trauma surgery, orthopedics, and interventional radiology for embolization
Prognosis
- High associated mortality rate
- Isolated pelvic fracture with hypotension: 15-40%
- Associated intra-abdominal injury: > 50%
- Associated intra-abdominal and head injuries: > 90%
- Hemorrhagic shock is the leading cause of death
- Chronic pain
- At a median follow up of 52 months, 64% of patients reported chronic post-traumatic pelvic pain (Halawi 2016)
- Sexual dysfunction
- 61% of men reported sexual dysfunction after pelvic ring injury (Halawi 2016)
Take Home Points
- Suspect vertical shear pelvic fracture in any patient with a high-energy axial-directed force of injury. Common exam findings include leg length discrepancy and pelvic instability
- Superior displacement of hemipelvis on radiography is diagnostic but may be absent. Consider CT imaging if posterior injuries are not visible on X-ray and if patient is hemodynamically stable.
- Immediate management focuses on placement of a pelvic binder and a focus on trauma resuscitation
Read More
EMCrit: Severe Pelvic Trauma
EM: RAP: Pelvic Fractures – Anatomy of the Bleed
EM: RAP HD Videos: Pelvic Fractures
EM: RAP: Pelvic Binder Placement
Core EM: How to Place a Pelvic Binder
References
Burgess AR et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30(7):848-56. PMID: 2381002
Dalal SA et al. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma 1989;29(7): 981-1000. PMID: 2746708
Durkin A et al. Contemporary management of pelvic fractures. Am J Surg 2006;192(2): 211-23. PMID: 16860634
Halawi MJ. Pelvic ring injuries: Emergency assessment and management. J Clin Orthop Trauma 2015;6(4): 252-8. PMID: 26566339
Halawi, MJ. Pelvic ring injuries: Surgical management and long-term outcomes. J Clin Orthop Trauma 2016;7(1): 1-6. PMID: 26908968
Scheyerer MJ et al. Detection of posterior pelvic injuries in fractures of the pubic rami. Injury 2012; 43(8): 1326-9. PMID: 22682148
Scott I et al. The prehospital management of pelvic fractures: initial consensus statement. Emerg Med J 2013;30: 1070-1072. PMID: 24232012








