Author: Juliette Conte, MD (EM Resident, Brooke Army Medical Center) and Lloyd Tannenbaum, MD (EM Resident, Brooke Army Medical Center)// Edited by: Jamie Santistevan, MD (@jamie_rae_EMdoc – EM Physician, Presbyterian Hospital, Albuquerque, NM); Manpreet Singh, MD (@MPrizzleER – Assistant Professor of Emergency Medicine / Department of Emergency Medicine – Harbor-UCLA Medical Center); and Brit Long, MD (@long_brit – EM Attending Physician, San Antonio, TX)
Welcome to this edition of ECG Pointers, an emDOCs series designed to give you high yield tips about ECGs to keep your interpretation skills sharp. For a deeper dive on ECGs, we will include links to other great ECG FOAMed!
This week we are continuing our Syncope Series with a discussion of Wolff-Parkinson-White (WPW). As a refresher, any patient that presents with syncope should have a thorough history and physical exam, with an ECG. These recommendations are based on the ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope which has been endorsed by ACEP as guidelines for clinical practice. As previously discussed, I screen every ECG for DQ@HEB:
D: Delta wave (Wolff-Parkinson-White)
Q: QT Prolongation
@: AV nodal blocks
H: HCM (look for dagger Q waves)
E: Epsilon wave (Arrhymogenic Right Ventricular Dysplasia)
B: Brugada pattern
The Case:
An 18-year-old active duty military basic trainee with no known medical history presents to the Emergency Department after losing consciousness in the middle of his two-mile run. On presentation, the patient is at his baseline mental status with no acute complaints. His neurological exam is unremarkable. He reports no prodrome prior to the syncopal event, and the only thing he remembers is his buddy standing over him shouting his name. An ECG is obtained and shown below:

This ECG shows normal sinus rhythm at 75 bpm with short PR interval and widened ventricular complexes with the delta wave morphology consistent with Wolff-Parkinson-White (WPW). (ECG compliments of Dr. Tyler Davis).
You suspect the patient has a pre-excitation syndrome. How do you manage a patient like this? Do you discharge home or admit? What if the patient became symptomatic again in the ED and develops hemodynamic instability?
Let’s talk a little more about Wolff-Parkinson-White Syndrome, and then we’ll return to the case.
2015 ACC/AHA/HRS Definition of WPW Syndrome: A syndrome characterized by documented SVT or symptoms consistent with SVT in a patient with ventricular pre-excitation during sinus rhythm.1
**If ECG findings of ventricular pre-excitation occur in patients without symptoms or history of arrhythmia, the disorder is called asymptomatic ventricular preexcitation or asymptomatic WPW.2 The isolated ECG finding is called a WPW-pattern.
Pathophysiology of WPW:
Patients with WPW have impulse-conducting fascicles within the atria, known as an accessory pathway (AP). This pathway results in an electrical connection between the atria and ventricles, across the annulus fibrosis, that bypasses the atrioventricular (AV) node. This pathway, referred to as the Bundle of Kent, can be located at various locations within the atria and can have numerous different histopathologic and electrophysiologic properties. Numerous other accessory pathways exist between the atria and ventricles, however these pathways have distinct histopathologic features from the Bundle of Kent and do not manifest as the typical ECG findings in WPW. Some examples of the other pathways include James fibers seen in LGL syndrome, Brechenmacher fibers, and Mahaim fibers.
What ECG changes do we see in WPW?
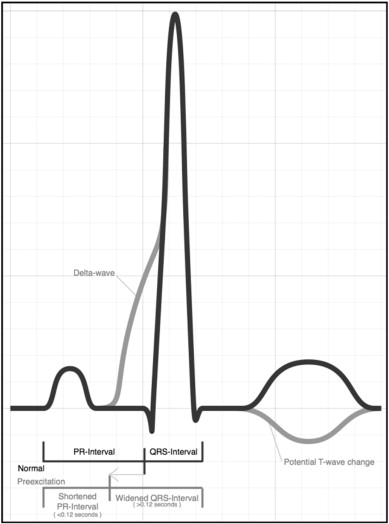
Source: Hoyt W, Snyder CS. The asymptomatic Wolff-Parkinson-White syndrome. 2012. doi:10.1016/j.ppedcard.2012.11.003

Source: https://en.ecgpedia.org/index.php?title=File:Wpw2.svg
In WPW, impulses from the AP and the AV node simultaneously transmit to the ventricles, resulting in early depolarization from the AP in combination with normal depolarization through the AV node-His-Purkinje system. There is a short PR interval, which should normally represent a delay of impulse through the AV node, due to early ventricular depolarization that has bypassed the AV node. The early upstroke of the QRS, termed the delta wave, represents early ventricular depolarization that has traveled anterograde through the AP outside of the AV node-His-Purkinke system. Ventricular conduction outside of the His-Purkinje system results in early but slower depolarization of the ventricles. The remainder of the QRS is representative of normal ventricular depolarization through the AV node and the His-Purkinje system. (A combination of a sinus beat and a ventricular beat is also known as a fusion beat. Fusion beats are also seen in Ventricular Tachycardia).
Background:
This combination of ECG findings, characteristic of WPW, were first reported in 1930 by Drs. Wolff, Parkinson, and White in 11 young, healthy patients without structural cardiac disease who were discovered to have a short P-R interval with a wide QRS and paroxysms of SVT.3 This study initially credited the early ventricular depolarization to abnormal CNS stimulation of the heart, hypothesizing that the pre-excitation was not due to any structural cardiac abnormalities (i.e. an accessory pathway) but rather a neurologic mechanism.
Curious about where the “Bundle of Kent” got its name? Around the same time period, Dr. Stanley Kent had already published evidence of lateral atrio-ventricular conductive tissue connections, which he believed to be the physiologic AV nodal tissue.4 Dr. Kent was an anatomist at Oxford attempting to determine how the electrical signals moved from the atria (then called auricles) to the ventricles. This extranodal conductive tissue was later determined to be the pathologic accessory pathway in WPW, and Dr. Kent remains credited with the discovery.
Epidemiology of WPW: Prevalence of 0.1 to 3.1 per 1000.5
Clinical Presentation: Patients with WPW can present with a spectrum of symptoms ranging from asymptomatic to dizziness, palpitations, chest pain, shortness of breath, near-syncope, syncope, or even sudden cardiac death.
Cardiac Rhythms associated with WPW:
Sinus Rhythm (see our patient’s initial ECG):
- ECG Findings:
- PR interval <120 msec
- Delta wave – slurred upstroke of initial portion of the QRS complex
- QRS complex > 100msec
- Possible ST/T wave changes directly opposite the major delta and QRS complexes
- Type A (left-sided accessory pathway): positive delta wave in all precordial leads with R/S>1 in V1
- Type B (right-sided accessory pathway): negative delta wave in leads V1 and V2
- Management:
- Asymptomatic (i.e. incidental finding on EKG): Refer patient for outpatient routine follow-up for risk stratification with an echocardiogram, exercise stress testing and/or electrophysiologic studies. These patients may undergo regular periodic observation or possible catheter ablation.2
- Symptomatic: Admit patient to cardiology if unstable, persistently tachycardic, persistently symptomatic, experienced a syncopal episode, or required cardioversion. The ACC/AHA recommend catheter ablation and/or oral antiarrhythmics for long-term management in these patients.1
Reentrant Paroxysmal SVT (80% of arrhythmias in WPW): A conductive loop is created between the AP and the AV node. Conduction travels anterograde (from atria to ventricle) down one pathway and retrograde (from ventricle to atria) up the alternate pathway. Since there are two pathways for the electrical impulses to take (down the physiologic pathway and up the accessory pathway or vice-versa), there are two different arrhythmias associated with WPW. They are diagramed in the picture below and then explained.

This image shows the different pathways that electricity can take in patients with WPW. Image obtained from: https://www.pondermed.com/case-based/case-1-whos-afraid-of-big-bad-wolff/ For more FOAM on WPW, see their great WPW write up at that link!
- Orthodromic AVRT: Impulses travel anterograde down the AV node-His Purkinje system and retrograde up the AP. Accounts for 90-95% of AVRT in WPW.
- ECG: Narrow complex tachycardia
- Rapid, regular, narrow QRS complexes
- Delta wave not seen
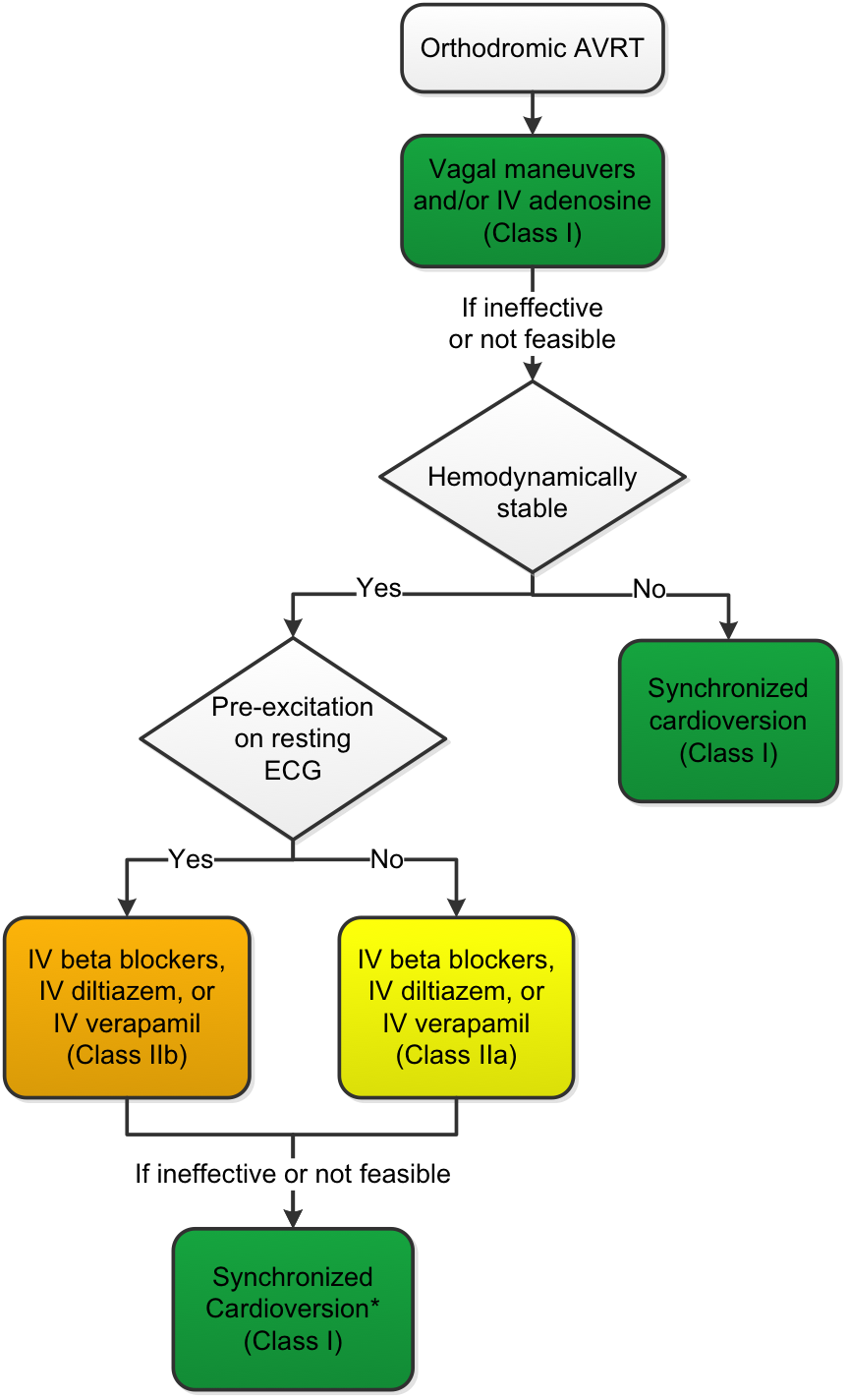
- Management: Basically, follow standard ACLS protocol for SVT.
- Hemodynamically stable: Vagal maneuvers, adenosine, IV diltiazem, IV verapamil, beta blockers, synchronized cardioversion (if all else fails)
- Hemodynamically unstable: Synchronized cardioversion
- ECG: Narrow complex tachycardia
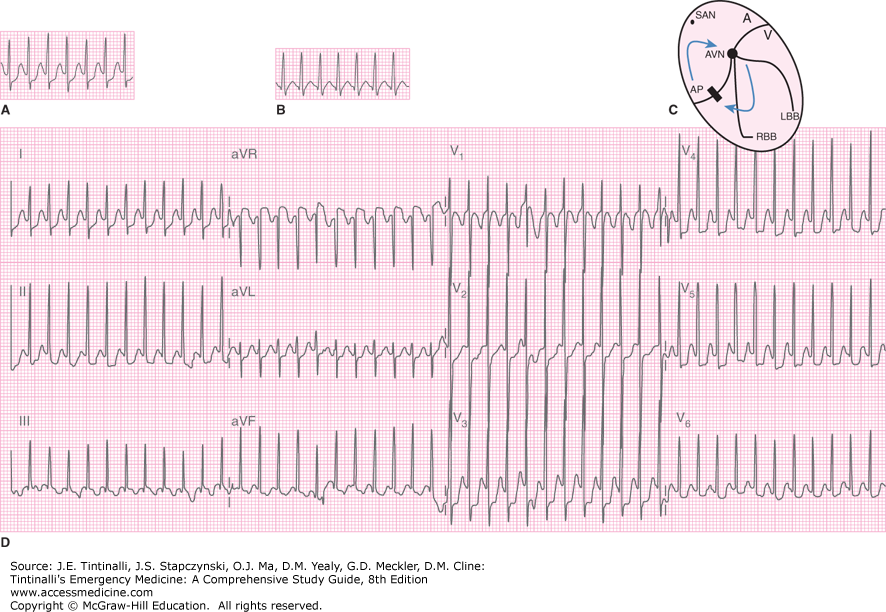
This image shows a classic example of what an EKG will look like in a patient with Orthodromic Conduction.
This flowsheet shows the management of Orthodromic AVRT, taken from 1.
- Antidromic AVRT: Impulses travel anterograde down the AP and retrograde through the AV node. Rare, occurs in less than 5% of patients with WPW6
- ECG: Wide complex, regular tachycardia (SVT with aberrancy)
- Regular tachycardia
- QRS complex >120 msec
- Ventricular rate 220-300 bpm
- May be confused with VTach
- Management:
- Hemodynamically stable: IV Procainamide 20-50mg/min IV over 30min up to 17mg/kg max
- Hemodynamically unstable: Synchronized cardioversion
- Avoid beta-blockers, calcium-channel blockers, adenosine and digoxin!! These may precipitate ventricular fibrillation.
- ECG: Wide complex, regular tachycardia (SVT with aberrancy)
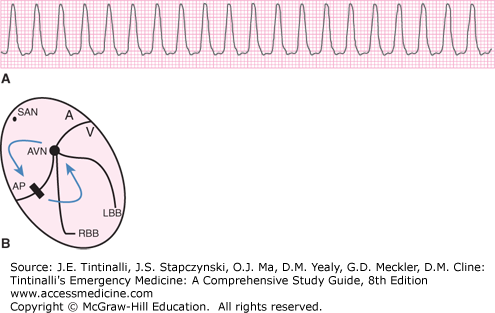
This image shows a classic example of Antidromic Conduction
Atrial fibrillation with WPW (a subset of orthodromic AVRT): 20% to 30% of patients with WPW will also have atrial fibrillation. The coincidence of these arrhythmias is not correlated with additional structural cardiac disease.
- ECG: Wide complex, irregular tachycardia
- Irregular ventricular rate
- Beat-to-beat variation in QRS morphology
- Management:
- Hemodynamically stable (most will be unstable): IV procainamide (20-50mg/min IV over 30min up to 17mg/kg max) or IV ibutilide
- Hemodynamically unstable with wide, irregular rhythm: Unsynchronized cardioversion7
- Avoid beta-blockers, calcium-channel blockers, adenosine and digoxin!! These may precipitate ventricular fibrillation.
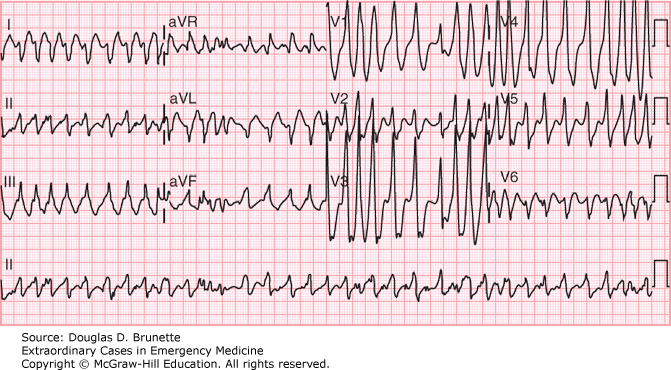
Citation: Electrocardiogram, Brunette DD. Extraordinary Cases in Emergency Medicine; 2019. Available at: https://accessemergencymedicine.mhmedical.com/content.aspx?sectionid=203273679&bookid=2514&jumpsectionID=203273777&Resultclick=2 Accessed: January 12, 2019 Copyright © 2019 McGraw-Hill Education. All rights reserved
Yikes! This rate is approximately 300 bpm! This is a classic example of atrial fibrillation with WPW. Someone should assess this patient immediately!
Case conclusion:
Let’s return to our case from above. The patient remained hemodynamically stable in the Emergency Department with no reoccurrence of tachydysrhythmia. He was admitted to the Cardiology service and underwent an electrophysiologic study with radioablation of a right-sided accessory pathway.
References:
- Caldwell MA, Calkins H, Conti JB, et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2016;133:506-574. doi:10.1161/CIR.0000000000000311
- Hoyt W, Snyder CS. The asymptomatic Wolff-Parkinson-White syndrome. 2012. doi:10.1016/j.ppedcard.2012.11.003
- Wolff L, Parkinson J, White PD. Bundle-Branch Block with Short P-R Interval in Healthy Young People Prone to Paroxysmal Tachycardia. Am Heart J. 1930;5(6):685-705.
- Kent AF. Researches on the Structure and Function of the Mammalian Heart. J Physiol. 1893;14(4-5):i2-254. http://www.ncbi.nlm.nih.gov/pubmed/16992052. Accessed January 12, 2019.
- Dixon AC. Syncope, Dysrhythmias, and ECG Interpretation in Children. In: Tintinalli JE, Stapczynski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. New York, NY: McGraw-Hill Education; 2016. http://accessemergencymedicine.mhmedical.com/content.aspx?aid=1132927325.
- Ali R, Tahir A, Nadeem M, Shakhatreh MI, Faulknier B. Antidromic Atrioventricular Reentry Tachycardia with Wolff Parkinson White Syndrome: A Rare Beast. doi:10.7759/cureus.2642
- Alpert JS, Calkins H, Joaquin Cigarroa zx E, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Vol 64.; 2014. doi:10.1016/j.jacc.2014.03.022








