Authors: Veronica Morgan, MD (EM Resident Physician, UTSW – Dallas, TX); Vietvuong Vo, MD (Assistant Professor of EM/Attending Physician, UTSW – Dallas, TX) // Reviewed by: Sophia Görgens, MD (EM Resident Physician, Zucker-Northwell NS/LIJ, NY); Cassandra Mackey, MD (Assistant Professor of Emergency Medicine, UMass Chan Medical School); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 67-year-old female with past medical history of hypertension presents with acute onset of chest pain without associated symptoms. She describes the pain as left-sided, non-radiating, and 9/10 in severity.
Initial vital signs include BP of 157/80, HR of 96, RR 14, SpO2 of 97% on RA, T 37.5. On exam, she is clutching her chest and is in acute distress due to pain with no other remarkable findings. ECG shows ST-segment elevation in V3-V6 only with depression in aVR. Initial troponin is mildly elevated. The catheterization lab is activated, but catheterization shows no coronary artery occlusion.
On further questioning, the patient denies recent illness but does mention that her daughter passed away in a car accident yesterday.
What is the diagnosis?
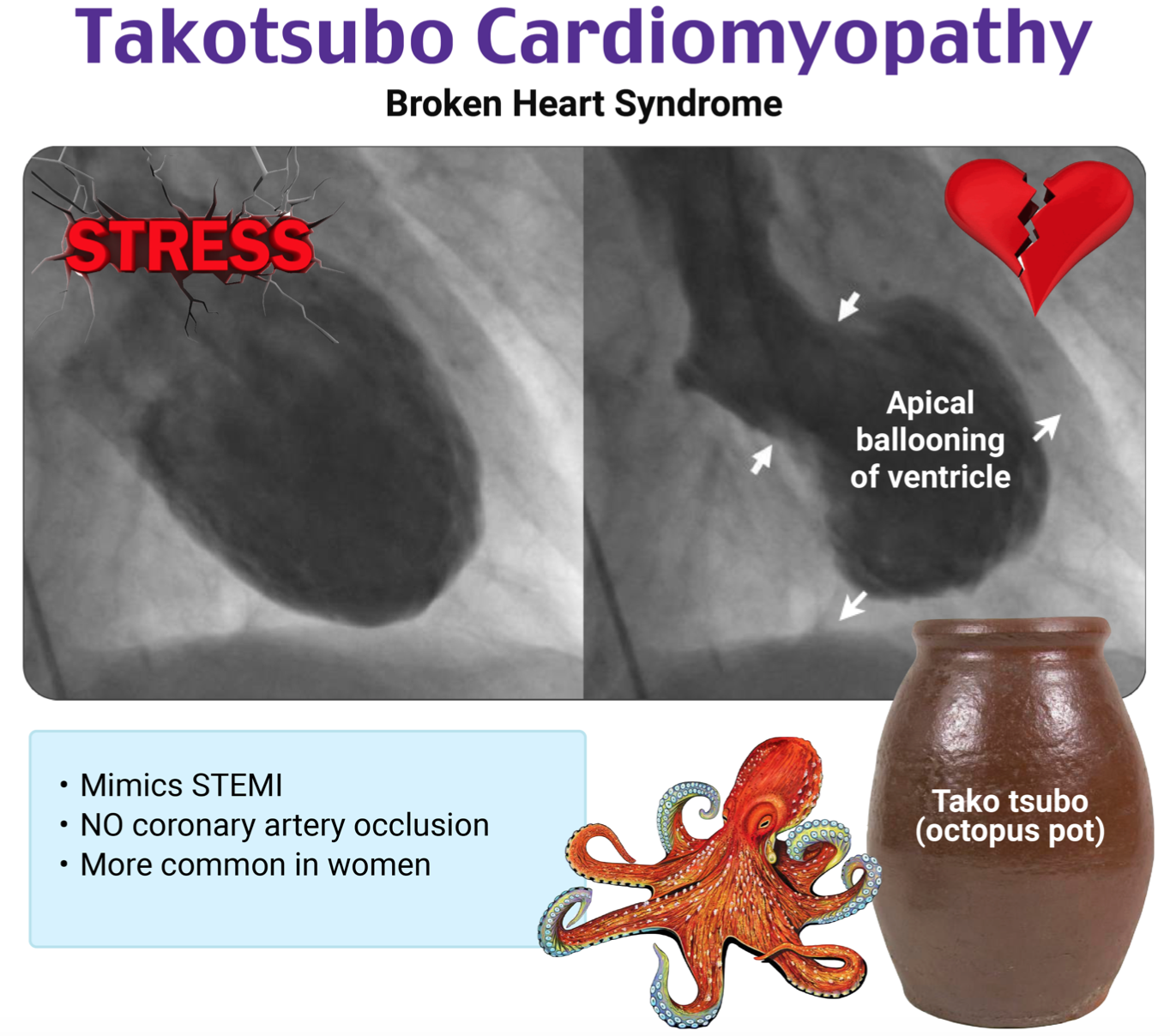
Answer: Takotsubo Cardiomyopathy 1-18
Background:
- Also known as transient apical ballooning syndrome, apical ballooning cardiomyopathy, stress-induced cardiomyopathy, stress cardiomyopathy, Gebrochenes-Herz syndrome, and broken-heart syndrome. 1
Etiology:
- Transient regional systolic dysfunction of the left ventricle in the absence of angiographically significant coronary artery disease or acute plaque rupture 1
- Apical takotsubo is the most common (80%) 2
- Thought to be due to intense catecholamine surges causing myocardial stunning
- Epinephrine affects beta-adrenergic receptors, which have the highest density at the apex of the heart
Epidemiology:
- Risk factors: female sex, increased age, estrogen deficiency, genetic factors, emotional or physical stress, prior history of Takotsubo 3
- Incidence unclear, one systematic review of patients presenting with suspected acute myocardial infarction (MI) measured a prevalence of 1.7 to 2.2% 5
- In one large series, 90% patients were women with an average age of 65 years old 6
Clinical Presentation:
- Often triggered by intense emotional or physical stress
- Identifiable stressors are only present in 70% of cases4
- Examples include death of relatives, natural calamities, accidents or major trauma, arguments, financial loss, diagnosis of medical illness, stimulant drugs 1
- Even positive life events can lead to this; so-called “happy-heart syndrome” 1
- Most common symptoms include chest pain, dyspnea, syncope, palpitations 7
- Physical exam
- May have arrhythmia or signs of heart failure, valvular damage, or cardiogenic shock 1
- Patients with ACS can present with the same findings
Evaluation:
- ECG – cannot reliably differentiate between Takotsubo and occlusive MI 8
- Dynamic ECG changes may evolve in typical stages 8
- Stage 1 – ST segment elevation
- Stage 2 – Normalization of ST segment
- Stage 3 – Diffuse T wave inversions (often appears on day 1-3)
- Stage 4 – Normalization of T waves
- STE in stage 1 usually in pre-cordial leads although can be diffuse with no or minimal elevation in V1, as shown in the ECG below 9
- Dynamic ECG changes may evolve in typical stages 8

- Features that suggest Takotsubo versus MI within 6 hours of symptom onset 9
- Absence of reciprocal ST depression
- Due to myocardial dysfunction being limited to the apex 8
- Lack of STE in V1 with concomitant STD in aVR
- Absence of reciprocal ST depression
- Diffuse TWI mainly in precordial leads but can be more diffuse 8
- Duration of TWI long compared to short duration of STE
- May cause wide TWI resembling a SAH T wave pattern 11

- Lab Findings
- Cardiac biomarkers such as troponin may be mildly elevated 12
- BNP can be elevated due to the stress on the myocardium and usually exceeds those seen with ACS, but this is overall nonspecific 13
- TTE Findings
- Classical variant (i.e., apical ballooning pattern) – systolic ballooning of the apex of the left ventricle with akinesia and hyperkinesis of the base (80%) 12
- Atypical variants
- Mid-ventricular variant – mid-ventricular hypokinesis w/ normal apical function (14.6%)
- Basal type (reversed variant) – basal hypokinesis w/ normal function of the apex (2.2%)
- Focal variants – focal areas of hypokinesis, most commonly the anterolateral segment dysfunction (1.5%)
- Global hypokinesis – diffuse hypokinesis (<1%)
- Right ventricular involvement – up to 15% of cases may involve the RV 14
- Poor prognostic sign
- These patients tend to have higher number of comorbidities compared to those without
- Have higher risk of complications such as shock and heart failure
- Seen on echo as biventricular ballooning
- Poor prognostic sign
- Left ventricular outflow tract obstruction (LVOTO) due to turbulent blood flow in the aortic outflow tract pulling the mitral valve anterior leaflet anteriorly 15
- Leads to mitral valve regurgitation
- Occurs in the classical (apical variant) in about 10% of cases
- Cardiac MRI 16
- Can help differentiate between Takotsubo and acute MI if coronary angiography has not been performed, is inconclusive, or is unavailable
- Compared to acute MI, Takotsubo will have not have late gadolinium enhancement
- Can help with diagnosis of exclusion by excluding other causes of left ventricular dysfunction such as myocarditis or emboli
- Can also evaluate for complications like mural thrombus, RV dysfunction, or pericardial effusion
- Can help differentiate between Takotsubo and acute MI if coronary angiography has not been performed, is inconclusive, or is unavailable
- Cardiac Catheterization 1
- Typically demonstrates normal coronary anatomy or some degree of coronary atherosclerosis but no severe occlusion
Diagnosis:
- Diagnosis of exclusion as it is often indistinguishable from ACS
- Usually made after coronary angiography in combination with the ECG and echo findings
- Mayo Clinic diagnostic criteria (all of the following criteria below are required to meet diagnosis): 17
- Transient hypokinesis, akinesis, or dyskinesis in the left ventricular mid segments with or without apical involvement
- Regional wall motion abnormalities beyond a single epicardial vascular distribution
- The absence of obstructive coronary disease or angiographic evidence of acute plaque rupture
- New ECG abnormalities (ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin
- The absence of pheochromocytoma and myocarditis
- Differentiation from occlusive MI or acute coronary syndrome
- Even when the STE pattern and cardiac ultrasound both suggest Takotsubo, coronary angiography is still essential to rule out MI 10
Treatment:
- No prospective randomized data on management; generally base on expert consensus and clinical experience1
- Cardiology consultation is necessary, as many of these patients will require coronary angiography to exclude ACS
- Hemodynamically stable treatment
- Initial treatment is similar to ACS in the ED, including aspirin, nitroglycerin for pain 1
- Hemodynamically unstable with LVOTO 15
- Fluid resuscitation if adequate EF and no signs of fluid overload
- Beta-blockade can improve LVOTO
- Use those with short half-life such as esmolol
- Avoid diuretics and positive inotropes as they exacerbate LVOTO
- Hemodynamically unstable without LVOTO 15
- Inotropes can improve cardiac output and organ perfusion however
- Can increase sympathetic tone, further exacerbating underlying cause of the cardiomyopathy
- Can use volume resuscitation and phenylephrine instead of inotrope to support perfusion without increasing stress on myocardium
- In severe shock, ECMO can be used as bridge to recovery if available
- Inotropes can improve cardiac output and organ perfusion however
Prognosis:
- Recent observation data suggest that rates of adverse events and death are similar to those with acute coronary syndrome 18
- In-hospital mortality approximates 3%, driven by heart failure, malignant arrythmia, cardioembolic events
- Although more prevalent in post-menopausal females, when it occurs in males, there is a 3 times increased risk of adverse cardiac/cerebrovascular events and death 18
- Likely due to increased risk and burden of comorbidities
Pearls:
- This is not a benign event as it has similar mortality to that of acute coronary syndrome
- Do not anchor on patient presenting with a major life stressor as about 30% do not
- Recognition of left ventricular outflow tract obstruction is imperative as it has major implications on management
- Diagnosis of exclusion usually made after cardiac catheterization, so in general, assume and treat as acute coronary syndrome

A 72-year-old woman presents to the emergency department due to dyspnea. She reports worsening dyspnea on exertion for the past 2 days and a recent diarrheal illness that resolved without treatment 4 days ago. Vital signs show T of 99.0°F (37.2°C), BP of 85/48 mm Hg, HR of 112 bpm, RR of 20/min, and SpO2 of 96% on room air. Physical examination shows a late-peaking systolic murmur with cool distal extremities. The oral mucosa is moist. Electrocardiogram shows sinus tachycardia with ST elevation in leads V1, V2, and V3. Serum troponin and B-type natriuretic peptide are elevated. Bedside ultrasound shows hypokinesis of the basal portion of the left ventricle with an apparent sigmoid-shaped septum and a dilated inferior vena cava. Which of the following is the best next step in the management of this patient’s condition?
A) Dobutamine infusion and emergent cardiology consultation
B) Emergency pericardiocentesis
C) Heparin infusion
D) Intravenous crystalloid fluid resuscitation
E) Phenylephrine infusion and emergent cardiology consultation
Answer: E
Takotsubo syndrome, also known as takotsubo cardiomyopathy and stress cardiomyopathy, is a transient syndrome characterized by regional systolic dysfunction primarily of the left ventricle in the absence of obstructive coronary artery disease or plaque rupture. It was first described in Japan in 1991, where researchers noted a balloon shape to the left atrium resembling a trap used to catch octopuses in Japan. Both emotional and physical stressors can precede takotsubo syndrome, and known triggers include pregnancy, vomiting, diarrhea, hypoglycemia, and emotional distress. The underlying pathophysiology involves a stress-induced surge of catecholamines that cause dysfunction of cardiac myocytes. The exact cause of the apical ballooning that leads to the octopus trap shape is not known, but the prevailing theory is that regional myocardial stunning occurs due to excessive excitatory neurotransmitter stimulation.
Chest pain is the most common symptom in patients with takotsubo syndrome, with dyspnea and palpitations somewhat less common. Symptoms of heart failure and cardiogenic shock may develop in more severe cases. Takotsubo syndrome is often exceedingly difficult to distinguish from acute myocardial infarction in the emergency department, as there is significant overlap in many clinical and diagnostic features. The most common findings on ECG are ST elevation, most often in the anterior precordial leads, as well as sinus tachycardia and QT interval prolongation. Troponin and B–type natriuretic peptide are often elevated. Echocardiography shows regional wall motion abnormalities, typically in the left ventricle and, rarely, in the right ventricle. The typical finding is systolic apical ballooning of the left ventricular, but atypical findings can include mid-ventricular hypokinesis with sparing of the apex, hypokinesis of the base with sparing of the mid-ventricle and apex, and dysfunction of an isolated section of the left ventricle. Rarely do patients develop global hypokinesis.
Because takotsubo syndrome is often clinically indistinguishable from acute myocardial infarction, primary management includes cardiac catheterization for coronary angiography and percutaneous coronary intervention. Prior to this intervention, management in the ED is mainly supportive of the patient’s hemodynamic and cardiac status. Patients with features of shock may require vasopressors, and the decision on the specific drug hinges on the presence or absence of left ventricular outflow tract (LVOT) obstruction. Up to 25% of patients with takotsubo cardiomyopathy also develop a dynamic LVOT that is similar to hypertrophic cardiomyopathy, but the mechanism is not completely clear. Ultrasound findings can show bulging of the interventricular septum into the LVOT, which can be interpreted as a sigmoid-shaped septum on bedside evaluation. Patients with concomitant LVOT can develop shock without significant ventricular dysfunction, otherwise confusing the presentation and altering treatment decisions. Those requiring hemodynamic support without LVOT obstruction may benefit from inotropessuch as dobutamine. However, inotropes are known to worsen LVOT obstruction and should not be given to patients with evidence of shock and LVOT. Therefore, phenylephrine is the vasopressor of choice. Patients should be admitted to the hospital for rhythm monitoring and serial cardiac enzymes, but the long-term prognosis of takotsubo syndrome is generally good. Almost all patients with takotsubo syndrome show full resolution of clinical symptoms and normalization of systolic function and ballooning of the left ventricular apex.
Patients with evidence of LVOT obstruction (as demonstrated on ultrasound in this patient) should not receive inotropic medications like dobutamine (A), as this carries a high risk of worsening the obstruction.
Emergency pericardiocentesis (B) is a temporizing procedure reserved for critically ill patients with pericardial effusion and cardiac tamponade, neither of which this patient has.
Anticoagulation in the form of heparin infusion (C) is commonly used in patients with acute myocardial infarction and other ischemic conditions but does not have a role in the management of takotsubo syndrome.
This patient’s recent diarrheal illness raises suspicion for hypovolemia, which would be treated with fluid resuscitation (D), but her moist oral mucosa and dilated inferior vena cava suggest an eu- or hypervolemic state. Additional fluids will not improve her condition and may worsen it.
Further Reading
Further FOAMed:
https://emcrit.org/ibcc/takotsubo/
https://radiopaedia.org/articles/takotsubo-cardiomyopathy?lang=us
References:
- Ahmad SA, Brito D, Khalid N, et al. Takotsubo Cardiomyopathy. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430798/?report=classic
- Keramida K, Backs J, Bossone E, Citro R, Dawson D, Omerovic E, Parodi G, Schneider B, Ghadri JR, Van Laake LW, Lyon AR. Takotsubo syndrome in Heart Failure and World Congress on Acute Heart Failure 2019: highlights from the experts. ESC Heart Fail. 2020 Apr;7(2):400-406. doi: 10.1002/ehf2.12603
- Amin HZ, Amin LZ, Pradipta A. Takotsubo Cardiomyopathy: A Brief Review. J Med Life. 2020;13(1):3-7. doi:10.25122/jml-2018-0067
- Takotsubo syndrome. EMCrit Project. Accessed May 15, 2023. https://emcrit.org/ibcc/takotsubo/
- Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006 Jul;27(13):1523-9.
- Sattar Y, Siew KSW, Connerney M, Ullah W, Alraies MC. Management of Takotsubo Syndrome: A Comprehensive Review. Cureus. 2020 Jan 3;12(1):e6556. Doi: 10.7759/cureus.6556
- CTG Labs – NCBI. beta.clinicaltrials.gov. Accessed May 16, 2023. https://beta.clinicaltrials.gov/study/NCT01947621
- Namgung J. Electrocardiographic Findings in Takotsubo Cardiomyopathy: ECG Evolution and Its Difference from the ECG of Acute Coronary Syndrome. Clinical Medicine Insights: Cardiology. 2014;8:CMC.S14086. doi:https://doi.org/10.4137/cmc.s14086
- Kosuge M, Ebina T, Hibi K, et al. Simple and Accurate Electrocardiographic Criteria to Differentiate Takotsubo Cardiomyopathy From Anterior Acute Myocardial Infarction. Journal of the American College of Cardiology. 2010;55(22):2514-2516. doi:https://doi.org/10.1016/j.jacc.2009.12.059
- Chest pain, sinus tachycardia, and ST Elevation. hqmeded-ecg.blogspot.com. http://hqmeded-ecg.blogspot.com/2018/01/chest-pain-sinus-tachycardia-and-st.html
- Lee VH, Connolly HM, Fulgham JR, Manno EM, Brown RD Jr, Wijdicks EF. Tako-tsubo cardiomyopathy in aneurysmal subarachnoid hemorrhage: an underappreciated ventricular dysfunction. J Neurosurg. 2006;105(2):264-270. doi:10.3171/jns.2006.105.2.264
- Templin C, Ghadri JR, Diekmann J, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015;373(10):929-938. doi:10.1056/NEJMoa1406761
- Frohlich GM, Schoch B, Schmid F, et al. Takotsubo cardiomyopathy has a unique cardiac biomarker profile: NT-proBNP/myoglobin and NT-proBNP/troponin T ratios for the differential diagnosis of acute coronary syndromes and stress induced cardiomyopathy. International Journal of Cardiology. 2012;154(3):328-332. doi:https://doi.org/10.1016/j.ijcard.2011.09.077
- Citro R, Bossone E, Parodi G, et al. Clinical profile and in-hospital outcome of Caucasian patients with takotsubo syndrome and right ventricular involvement. 2016;219:455-461. doi:https://doi.org/10.1016/j.ijcard.2016.06.039
- Di Vece D, Silverio A, Bellino M, et al. Dynamic Left Intraventricular Obstruction Phenotype in Takotsubo Syndrome. Journal of Clinical Medicine. 2021;10(15):3235. doi:https://doi.org/10.3390/jcm10153235
- Singh T, Khan H, Gamble DT, Scally C, Newby DE, Dawson D. Takotsubo Syndrome: Pathophysiology, Emerging Concepts, and Clinical Implications [published correction appears in Circulation. 2022 May 17;145(20):e1053]. Circulation. 2022;145(13):1002-1019. doi:10.1161/CIRCULATIONAHA.121.055854
- Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008 Mar;155(3):408-17.
- Brinjikji W, El-Sayed AM, Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am Heart J. 2012 Aug;164(2):215-21.








