Authors: Brett Lee, MD (EM Resident Physician, LAC+USC Medical Center) and Jeff Riddell, MD (Assistant Professor of Clinical Emergency Medicine, LAC+USC Medical Center) // Edited by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
A 35-year-old right-hand dominant male with no past medical history presents to your ED. He is a construction worker and is endorsing left second finger pain after accidentally shooting his finger with a paint gun. By the time you see him, he has received hydrocodone 5-325 mg in triage and is endorsing improvement in his pain. He denies numbness, tingling, or decreased range of motion. Your exam is significant only for a small punctate lesion at the tip of his index finger, but is otherwise unremarkable. He is requesting to leave to return to work. What is the next most appropriate step in management?
Introduction
Orthopedic injuries are common in the emergency department and range from deceptively innocuous appearing injuries to amputated extremities. While many patients can be treated and discharged by the emergency physician, several conditions need emergent surgical evaluation. In this blog post, we break these down into three categories: infectious, neurovascular, and traumatic injuries.
Infectious
Non-Gonococcal Septic Arthritis
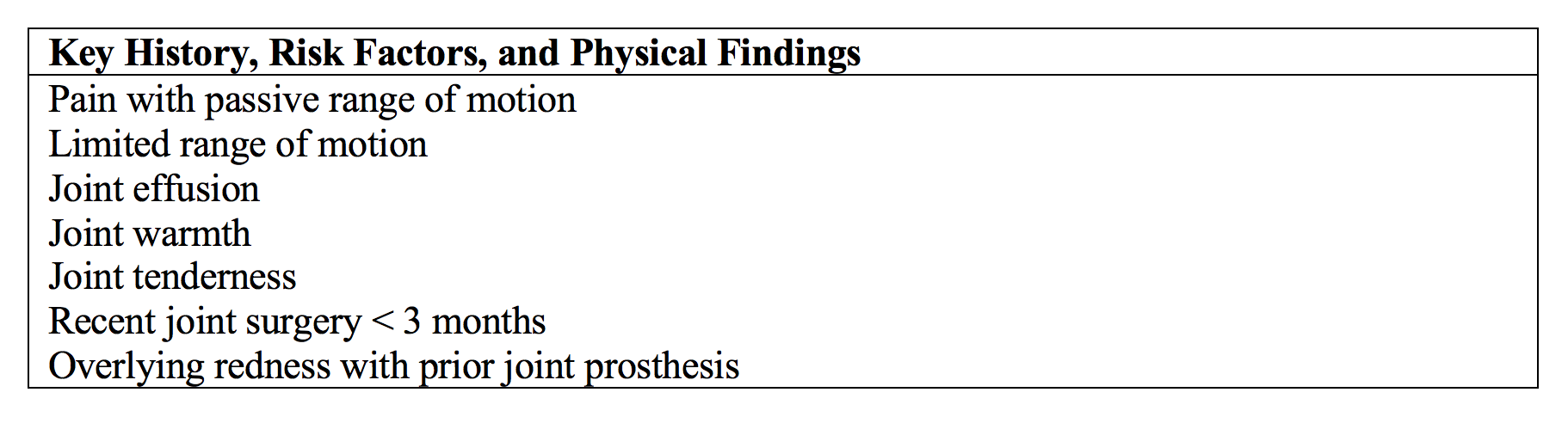
An infection in the joint space is a potentially lethal condition that has significant rates of morbidity if not addressed promptly. Septic arthritis accounts for roughly 8% of ED patients presenting for an acutely painful joint.1 Certain conditions should raise the suspicion of septic arthritis including elderly population, diabetes, rheumatoid arthritis, joint prosthesis or recent joint surgery, overlying skin infection, IVDU or alcoholism, and prior intraarticular corticosteroid injection. Patients classically present with an acute monoarticular arthritis associated with warmth, swelling, restricted range of motion, and fever, although not all of these factors have to be present. The knee is the most commonly affected joint, but other joints such as the wrist, hip, and ankles are not uncommon sites. The table below outlines key features of septic arthritis. 2,3,4
In any patient where septic joint is suspected, arthrocentesis must be performed. The table below can help guide providers in diagnosis.

When arthrocentesis is suggestive of septic arthritis or diagnosis is suspected clinically while awaiting definitive diagnosis, patients should be started on antibiotics. Choice of antibiotic regimen varies depending upon likely causative organism. Staph and strep infections are the most common organisms; therefore, vancomycin and ceftriaxone is a reasonable regimen to start for most patients. In addition, ceftriaxone covers gram negative and gonococcal arthritis, which will be discussed in further detail below. In the elderly, immunocompromised, health-care or nursing home exposed, and IV drug using populations, broader gram negative and pseudomonal coverage should be added with a 4th generation cephalosporin such as cefepime. After empiric treatment is initiated, orthopedic surgery should be consulted, as patients require inpatient admission for IV antibiotics, drainage, and possible open surgery. 5,6,19
Gonococcal Arthritis
Gonococcal arthritis is another form of septic arthritis that requires emergent orthopedic consultation. Its presentation is distinct from non-gonococcal septic arthritis by a number of factors. GC arthritis typically affects young, healthy, sexually active patients and is a complication of disseminated Neisseria gonorrhoeae. As a result, patients may also experience concomitant migratory arthralgias, fever, chills, dermatitis, and tenosynovitis. While variation exists, cutaneous lesions are classically described as pustular, localized to the dorsal aspect of distal extremities near joints, and transient (lasting only 4-6 days with or without treatment). Genitourinary symptoms may also aid in the diagnosis; however, notably, the majority of patients have asymptomatic genital, anal, or pharyngeal infections. In contrast to non-gonococcal arthritis, more distal joints such as the fingers, wrists, elbows, and knees are more commonly affected and may even be polyarticular.6,7,20
Diagnosis is also made by arthrocentesis with synovial analysis with similar findings to nongonococcal arthritis; however, some differences make this diagnosis more challenging. Culture may be negative in up to 50% of patients, and gram stains are frequently unreliable. Therefore, clinical suspicion should help guide your therapy. Treatment is similar to non-gonococcal septic arthritis including IV antibiotics and drainage. Of note, IM ceftriaxone and azithromycin/doxycycline as used to treat gonococcal urethritis or PID are not sufficient to treat gonococcal arthritis, and patients should be initiated on IV ceftriaxone; however, patients should still be treated for concurrent chlamydial infection. Patients should be admitted to the hospital for IV antibiotics, joint aspiration, and possible surgical exploration.6,7
Infectious Flexor Tenosynovitis
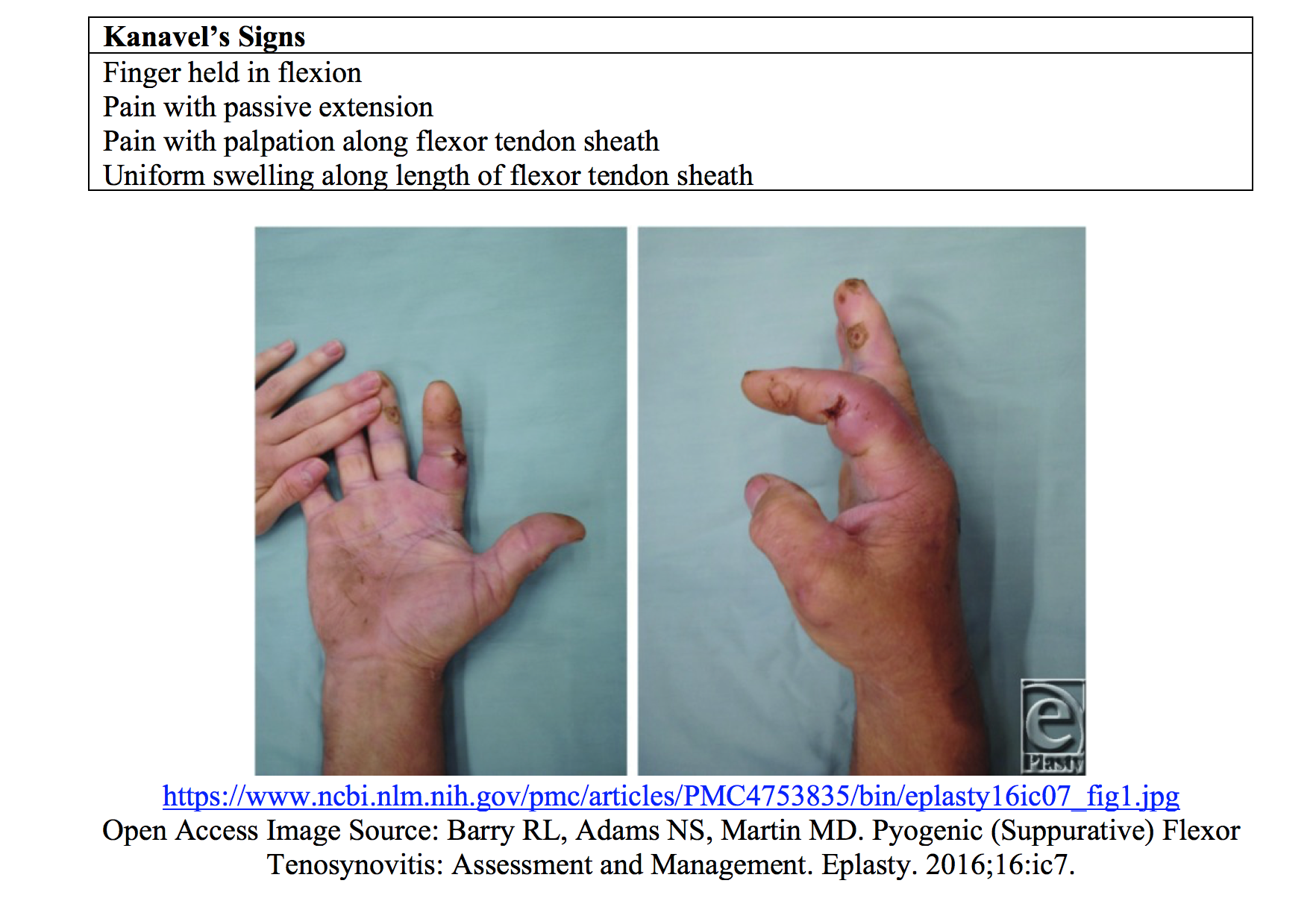
Infectious flexor tenosynovitis is another diagnosis requiring emergent orthopedic evaluation. FTS is a bacterial infection of the flexor tendon sheath, a potential space between the visceral epitenon layer and the outer parietal layer. Infections within this area can lead to rapid pressure build up, disruption of the neighboring anatomical barriers, and spread of the infection through the hand and forearm. Severe complications such as tendon necrosis, osteomyelitis, and loss of function are well documented with this disease process. Diagnosis should be made clinically in any patient with positive Kanavel’s signs, which are reviewed in the table below.8,9
Once identified, early IV antibiotics covering for staph, MRSA, and streptococcus should be initiated. Orthopedics should be consulted early, as these patients often need surgical intervention.9
Infected Fight Bite and Deep Hand Space Infections
For many of the same reasons as FTS, deep hand space infections are especially important to diagnose early. These infections frequently occur via direct inoculation or through local spread from infected tendons or bursae. Direct inoculations are frequently seen from human or animal bites, lacerations, IV drug use, or following surgical intervention. As with flexor tenosynovitis, the most common organisms tend to be MRSA, staph aureus, and streptococcal infections; however, human and animal bites should warrant consideration of more atypical organisms such as Eikenella and Pasteurella. Given the potential for local destruction, neurovascular complications, and potential spread of infection, IV antibiotic therapy and early consultation should be initiated early in anyone suspected of such an infection.9,10,11

Necrotizing Soft Tissue Infections
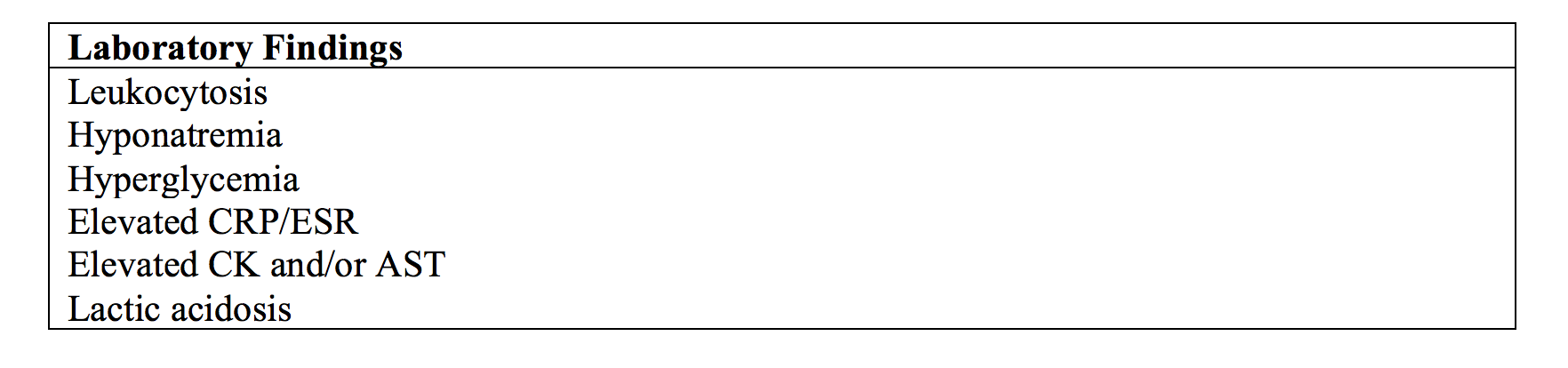
NSTI’s have the potential to cause significant morbidity and have high rates of mortality if not identified and treated early. Infections may be polymicrobial or monomicrobial, gas-producing or non-gas-producing, and may affect any layer of soft tissue ranging form epidermis to fascia to muscle body. Lower extremities are more frequently affected than upper extremities especially in patients with diabetes and those with compromised blood flow. These infections progress rapidly over the course of hours, rarely occurring sub-acutely over days. The table below reviews the most common findings in NSTI’s.12


Systemic toxicity is common, with patients often presenting febrile and tachycardic. As the disease progresses, patients may become hypotensive, septic, and develop anesthesia over the affected area secondary to neurovascular destruction. It is important to remember necrotizing soft tissue infections are a clinical diagnosis that can only be truly confirmed with surgical intervention; however, other key diagnostic features may lead one to consider to a diagnosis of NSTI.12
Decision making tools such as the LRINEC score may aid in the diagnosis of NSTI’s; however, physicians must be aware the LRINEC score has high rates of false positives and false negatives and should not be used for definitive diagnosis.17 In cases of suspected NSTI, there should be no delay in initiation of IV antibiotics and surgical consultation given high rates of morbidity and mortality. In cases of lower or moderate suspicion, labs as above and CT imaging with contrast may aid in the diagnosis, but should not delay surgical consultation. IV antibiotics should be of broad spectrum including coverage of MRSA, gram positives, gram negatives, and anaerobes. In addition, clindamycin should be included in coverage as it limits toxin release.12,
Neurovascular Injuries
Compartment Syndrome
Compartment syndrome is a true surgical emergency characterized by increasing pressures within fascial compartments leading to neurovascular compromise. Acute compartment syndrome is most commonly caused after significant trauma associated with fractures or dislocations; however, other common etiologies include crush injuries, burns, penetrating trauma, vascular injuries, bleeding diathesis, and overly constrictive bandages. Common locations include the forearm and leg with less common areas including the foot, thigh, gluteal, and abdominal regions. Sign and symptoms of compartment syndrome are outlined below.13
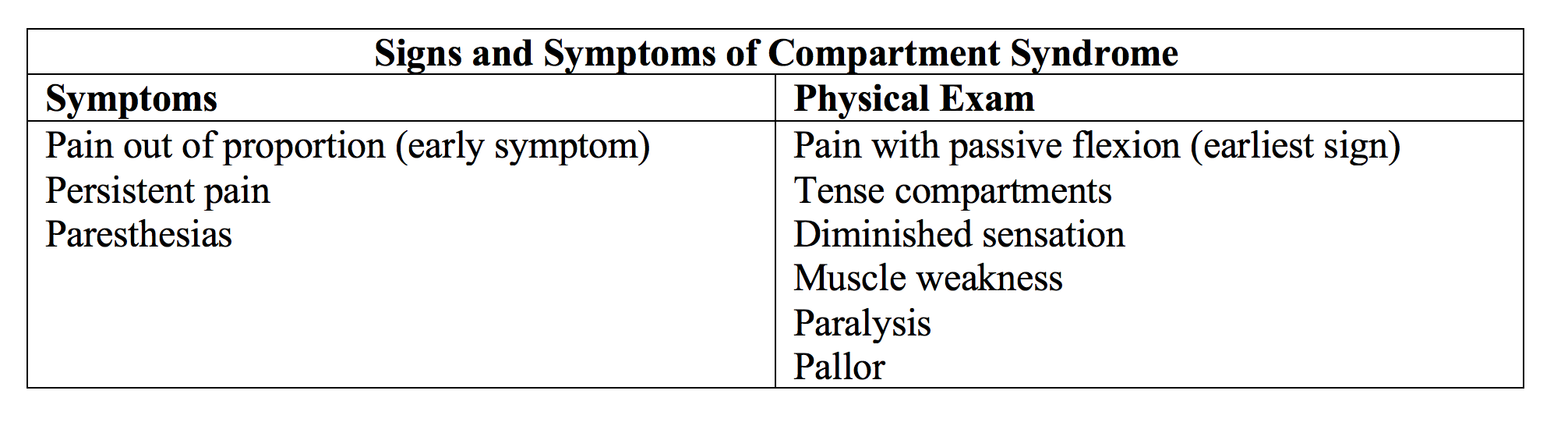
Without prompt recognition, compartment syndrome can lead to muscle contracture, sensory deficits, paralysis, and possibly limb amputation. Diagnosis should be made clinically, but can be confirmed by direct measurements of compartment pressures with manometers. Delta pressures can be used to determine likelihood of compartment syndrome.13

ED management should include removal of constrictive bandages or casting, placing the limb at level with the heart, and prompt surgical consultation for monitoring and possible fasciotomy.13
High Pressure Injection Injuries
Known primarily as an injury to industrial laborers, high pressure injection injuries can have devastating consequences. These injuries occur primarily in the patient’s non-dominant hand via a high-pressure gun such as grease gun or paint gun. Tissue damage occurs by three primary mechanisms. First, injected fluid travels through areas of least resistance including along the neurovascular bundles. This injury causes dissection of the soft tissue, vasospasm, and increasing edema resulting in compression, tissue ischemia, and thrombosis. Second, toxic substrates can cause tissue destruction and necrosis. Fibrosis is a long-term complication that can markedly restrict hand function. Thirdly, primary and secondary infections may occur as a result of injury.14,15,16
In spite of the significant damage that occurs beneath the surface, clinical presentations are often underwhelming. As described above, patients normally present with a small punctate injury; however, as the edema and necrosis worsens, patients develop significant pain, neurovascular compromise, and loss of function.14,15,16

In the emergency department, a thorough neurovascular exam should be performed, followed by gentle irrigation of any open wounds. Pain control is important; however, ring blocks (especially of fingers) should be avoided as these may worsen vascular flow. Information regarding the injected substrate should be obtained, and the patient should be monitored for systemic toxicity. Known complications include allergic reaction, rhabdomyolysis, lead toxicity, and hemolysis. Poison control should be consulted in cases of suspected toxic substrate, tetanus should be updated, and patients should be started on a third-generation cephalosporin. Emergent orthopedic consultation is warranted, as patients will likely need surgical debridement. Even in cases of prompt and appropriate therapy, patients frequently have poor outcomes including sensation defects, persistent pain, contracture, and amputation.14,15,16
Take Home Messages
- Septic arthritis most commonly affects the knee and should be on the differential for any monoarticular arthritis with limited passive range of motion and joint effusion.
- Non-gonococcal septic arthritis commonly occurs in elderly, immunocompromised, and those with prosthetic joints.
- Gonococcal arthritis is more frequent in young, healthy patients and is associated with migratory arthralgias, fever, chills, dermatitis, and tenosynovitis.
- Kanavel’s signs for FTS include: finger held in flexion, pain with passive extension, pain with palpation along flexor tendon sheath, and uniform swelling along length of flexor tendon sheath.
- Necrotizing soft tissue infection is a clinical diagnosis.
- A compartment pressure > 30 mm Hg and a delta pressure of < 30 mm Hg is suggestive of compartment syndrome.
- High pressure injuries seem innocuous but are a true orthopedic emergency.
This is the first of two posts on orthopedic emergencies. Stay tuned for the second post in this series on traumatic orthopedic emergencies!
This post is sponsored by www.ERdocFinder.com, a supporter of FOAM and medical education, who with their sponsorship are making FOAM material more accessible to emergency physicians around the world.
References / Further Reading:
- Shmerling RH, Delbanco TL, Tosteson AN, Trentham DE. Synovial fluid tests. What should be ordered? JAMA. 1990;264(8):1009-14.
- Margaretten ME, Kohlwes J, Moore D, Bent S. Does this adult patient have septic arthritis? JAMA. 2007;297(13):1478-88.
- Goldenberg DL. Septic arthritis and other infections of rheumatologic significance. Rheum Dis Clin North Am. 1991;17(1):149-56.
- Carpenter CR, Schuur JD, Everett WW, Pines JM. Evidence-based diagnostics: adult septic arthritis. Acad Emerg Med. 2011;18(8):781-96.
- Allison DC, Holtom PD, Patzakis MJ, Zalavras CG. Microbiology of bone and joint infections in injecting drug abusers. Clin Orthop Relat Res. 2010;468(8):2107-12.
- Shirtliff ME, Mader JT. Acute septic arthritis. Clin Microbiol Rev. 2002;15(4):527-44.
- O’brien JP, Goldenberg DL, Rice PA. Disseminated gonococcal infection: a prospective analysis of 49 patients and a review of pathophysiology and immune mechanisms. Medicine (Baltimore). 1983;62(6):395-406.
- Barry RL, Adams NS, Martin MD. Pyogenic (Suppurative) Flexor Tenosynovitis: Assessment and Management. Eplasty. 2016;16:ic7.
- Kennedy CD, Huang JI, Hanel DP. In Brief: Kanavel’s Signs and Pyogenic Flexor Tenosynovitis. Clin Orthop Relat Res. 2016;474(1):280-4.
- Rigopoulos N, Dailiana ZH, Varitimidis S, Malizos KN. Closed-space hand infections: diagnostic and treatment considerations. Orthop Rev (Pavia). 2012;4(2):e19.
- Kalbfell E, Adams NS, Cullen WT. Collar Button Abscess. Eplasty. 2016;16:ic6.
- Hakkarainen TW, Kopari NM, Pham TN, Evans HL. Necrotizing soft tissue infections: review and current concepts in treatment, systems of care, and outcomes. Curr Probl Surg. 2014;51(8):344-62.
- Via AG, Oliva F, Spoliti M, Maffulli N. Acute compartment syndrome. Muscles Ligaments Tendons J. 2015;5(1):18-22.
- Amsdell SL, Hammert WC. High-pressure injection injuries in the hand: current treatment concepts. Plast Reconstr Surg. 2013;132(4):586e-591e.
- Saraf S. High-pressure injection injury of the finger. Indian J Orthop. 2012;46(6):725-7.
- Verhoeven N, Hierner R. High-pressure injection injury of the hand: an often underestimated trauma: case report with study of the literature. Strategies Trauma Limb Reconstr. 2008;3(1):27-33.
- Neeki MM, Dong F, Au C, et al. Evaluating the Laboratory Risk Indicator to Differentiate Cellulitis from Necrotizing Fasciitis in the Emergency Department. West J Emerg Med. 2017;18(4):684-689.
- Nelson JA. Compartment pressure measurements have poor specificity for compartment syndrome in the traumatized limb. J Emerg Med. 2013;44(5):1039-44.
- Sharff KA, Richards EP, Townes JM. Clinical management of septic arthritis. Curr Rheumatol Rep. 2013;15(6):332.
- Ghosn SH, Kibbi AG. Cutaneous gonococcal infections. Clin Dermatol. 2004;22(6):476-80.










1 thought on “Orthopedic Emergencies: When to Ask for a Little Help from Our Friends”
Pingback: emDOCs.net – Emergency Medicine EducationOrthopedic Emergencies: When to Ask for a Little Help from Our Friends - Part Deux - emDOCs.net - Emergency Medicine Education