Authors: Nicole Vetter, MD (EM Resident Physician, University of Connecticut Emergency Medicine Residency) and Jesse Sturm, MD (Pediatric Emergency Medicine Attending, Connecticut Children’s Medical Center) // Edited by: Jennifer Robertson, MD, MSEd and Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UT Southwestern Medical Center / Parkland Memorial Hospital)
Case: You are in the middle of a ketamine sedation on a 7-year-old child whose forearm fracture is being reduced by the orthopedist. You notice the patient is becoming more agitated so you push another 1mg/kg dose of ketamine. Shortly after, you notice a diminished respiratory rate and capnography waveform. Soon after, the patient’s oxygen saturations drop. What are the next steps?
Procedural sedation and analgesia (PSA) is a core skill set of the emergency physician (EP). It improves patient satisfaction by providing amnesia, anxiolysis and analgesia. Sedation also makes our consultants happier as it facilitates an easier and faster procedure.
However, studies show that EPs inadequately treat pain in the emergency department (ED) for multiple reasons (1):
- Fear of over-sedation
- Fear of adverse events
- Inadequate knowledge
- Inadequate dosing
- Insufficient time
- Insufficient resources
10 Common PSA Errors
Error #1: Delaying deep sedation until fasting times are met
- The American Society of Anesthesiologists (ASA) states that the current fasting guidelines are based on insufficient evidence but still “strongly recommend” the following (2):
- 2 hours for clear liquids, 6 hours for a solid light meal and 8 hours for a fatty or fried meal
- ASA guidelines are often extrapolated to procedural sedation in the ED
- However, literature for procedural sedation in the ED states that fasting makes no difference on the risk of emesis or aspiration (3).
- Harms of delaying the procedure include increased pain, progression of lesion, and a more difficult procedure
- The American College of Emergency Physicians (ACEP) Clinical Policy 2013 guidelines state that procedural sedation should not be delayed in the ED based on fasting time (4)
- Always ensure, however, that your decisions on nil per os (NPO) status in sedation reflect your hospital’s applicable policies
Error #2: Believing PSA carries less risk than endotracheal intubation
- Do not be any less vigilant during PSA than you would for a critical patient requiring emergent intubation
- The risks of undergoing PSA may be less given that sedation in the ED generally involves healthy patients. However, PSA carries greater risk to those performing the sedation
- When PSA goes wrong, it is usually attributed to the sedation (as opposed to the emergently intubated patient who is very high risk to begin with)
Error #3: Minimizing risk of airway and breathing complications while using ketamine
- While it is true that ketamine has an excellent safety profile, airway/breathing events do occur by a variety of mechanisms
- Central apnea
- Airway malpositioning
- Laryngospasm
- Hypersalivation
- Over sedation with ketamine can be corrected with early recognition and appropriately-sized equipment at the bedside
Error #4: Not having full intubation setup nearby
- PSA = ‘Prepared to Solve Apnea’
- Hypoventilation/apnea is a predictable and acceptable consequence of PSA if that amount of sedation is required to facilitate the procedure
- Therefore, be prepared to manage airway obstruction and apnea using a stepwise approach (see below)
Error #5: Responding to hypoventilation or apnea with early and/or aggressive use of the bag-valve mask (BVM)
- In a comparison of intubated versus PSA patients:
- Oxygenation is more likely the predominant issue in intubated patients due to paralysis and thus, are more likely to benefit from early use of BVM
- In the PSA patient, hypoventilation is most likely due to airway or breathing issues
- Other steps should first be taken first to correct airway/breathing before using BVM
- Also, the risk of vomiting with BVM is greater as PSA patients are not paralyzed
- Use the BVM as only a PART of a stepwise approach to hypoventilation in PSA patients:
- Detection of the condition
- Stop any drug (s) and stop the ongoing procedure
- Position the patient – chin lift, bring head up, towel roll under shoulders
- Jaw thrust
- Suction if needed
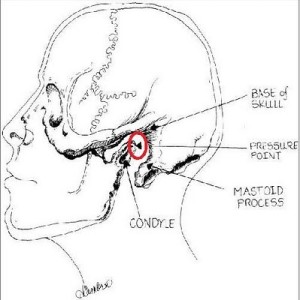
- If laryngospasm: apply pressure to laryngospasm notch (medial to earlobe between mastoid & condyle of jaw) (5)
- Use the BVM slowly and gently, ensuring a good seal and chest rise
- If unable to correct complications with high quality BVM, prepare to intubate
Error #6: If the oxygen saturation is ok, then the patient is breathing ok
- Focus on ventilation during PSA (not oxygenation)
- Capnometry alerts clinician to hypoventilation earlier than clinical assessment or pulse oximetry
- Use End Tidal CO2 (ETCO2) for all PSA – Level B recommendation by ACEP Clinical Policy (4)
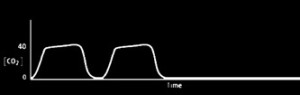
- The numeric value of ETCO2 is sometimes less important than the presence or absence of a waveform
- Do not correct apnea and hypoventilation with passive oxygen delivery alone (i.e. nasal cannula, facemask). Refer to stepwise approach above
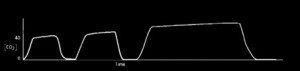
Bradypnea (slow breathing/tidal volumes preserved –> ETCO2 rises):
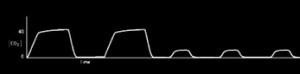
Hypopnea (shallow breathing/low TV –> ETCO2 falls):
Apnea (breathing stops):
Error #7: Withholding ketamine sedation on adults
- Ketamine provides excellent sedation and analgesia, and it can be safely used in adults
- An emergence reaction only occurs in 10-20% of adults and can be reduced with pre-induction comfort and coaching (6)
- How the patient feels entering a ketamine “trip” directly affects how they will emerge from the “trip”
- Give midazolam in 2mg doses (up to 4mg) if emergence reaction is of concern
- Concern for tachycardia and hypertension (HTN)
- A transient increase in heart rate (HR) or blood pressure (BP) for 15 minutes or so is almost always irrelevant (except in patients with severe coronary artery disease)
- If there is excessive HTN, give 10-20mg of propofol
Error #8: Adding an opioid with ketamine for sedation
- “Intravenous Subdissociative-Dose Ketamine versus Morphine for Analgesia in the Emergency Department” (7)
- Pain relief with ketamine (0.3mg/kg) and morphine (0.1mg/kg) are statistically similar
- Adding an opiate to a ketamine sedation will subject the patient to the adverse effects of opiates without any added benefit
Error #9: Using the same dosing strategy for propofol sedations as with fentanyl/midazolam
- Propofol is much shorter acting and does not accumulate in tissues like fentanyl/midazolam
- Will need to rebolus propofol to stay on top of the sedation
- Example propofol dosing strategy:
- Give a generous bolus up front (1-2mg/kg) over 20 seconds
- Anticipate a brief period of hypoventilation or apnea
- Rebolus 0.5mg/kg every 5-10 minutes as needed
Error #10: Using the same PSA dosing strategy for the elderly
- Elderly patients are highly sensitive to opiates, benzodiazepines, and propofol
- They will have longer periods of hypoventilation and hypotension
- Start low, go slow
*Adapted from Reuben Strayer’s PSA screencast at emupdates.com (8)
References / Further Reading
- Grant PS. Analgesia delivery in the Emergency Department. Am J Emerg Med, 2006;24(7):806–809.
- Apfelbaum et al. American Society of Anesthesiologists Committee. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011;114(3):495-511.
- Thorpe RJ, Benger J. Preprocedural fasting in emergency sedation. Emerg Med J 2010; 27:254–261.
- Godwin SA, et al. Clinical policy: procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2014;63(2)247-258.
- Larson CP Jr. Laryngospasm–the best treatment. Anesthesiology. 1998;89(5):1293-4.
- Strayer RJ, et al. Adverse events associated with ketamine for procedural sedation in adults. Am J Emerg Med. 2008 Nov;26(9):985-1028.
- Motov S, et al. Intravenous Subdissociative-dose Ketamine Versus Morphine for Analgesia in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2015; 66(3):222-229.
- Strayer, Reuben. “The Procedural Sedation Screencast Trilogy.” Emergency Medicine Updates. 28 Nov 2013. Web. 18 Mar 2016.








7 thoughts on “10 Procedural Sedation Errors in the Emergency Department”
I really like this, except for :
‘Error #6: If the oxygen saturation is ok, then the patient is breathing ok
• Focus on ventilation during PSA (not oxygenation)
o Capnometry alerts clinician to hypoventilation earlier than clinical assessment or pulse oximetry
• Use End Tidal CO2 (ETCO2) for all PSA – Level B recommendation by ACEP Clinical Policy (4)
o The numeric value of ETCO2 is sometimes less important than the presence or absence of a waveform
• Do not correct apnea and hypoventilation with passive oxygen delivery alone (i.e. nasal cannula, facemask). Refer to stepwise approach above’
This is a bit contradictory – if the O2 Sat is OK, why do you care about the CO2? _ transient hypercapnea is not relevant to safety in most patients and is a good respiratory stimulant! Our recent Cochrane review found that routine capnometry in PSA is associated with more interventions and no change in outcome, apart from a possible INCREASE in hypotension (probably because reassurance that you will pick up respiratory depression more reliably makes people more aggressive with medication).
Samuel G. Campbell
MB BCh, FCFP(EM), Dip PEC(SA), FCCHL.
Professor, Department of Emergency Medicine
Dalhousie University
Chief, Charles V. Keating Emergency and Trauma Centre
Queen Elizabeth II HSC
1796 Summer St, Halifax, Nova Scotia. B3H 3A7
Ph: 902-473 2020
Fax: 902-473 3617
I really like this, except for :
‘Error #6: If the oxygen saturation is ok, then the patient is breathing ok
• Focus on ventilation during PSA (not oxygenation)
o Capnometry alerts clinician to hypoventilation earlier than clinical assessment or pulse oximetry
• Use End Tidal CO2 (ETCO2) for all PSA – Level B recommendation by ACEP Clinical Policy (4)
o The numeric value of ETCO2 is sometimes less important than the presence or absence of a waveform
• Do not correct apnea and hypoventilation with passive oxygen delivery alone (i.e. nasal cannula, facemask). Refer to stepwise approach above’
This is a bit contradictory – if the O2 Sat is OK, why do you care about the CO2? _ transient hypercapnea is not relevant to safety in most patients and is a good respiratory stimulant! Our recent Cochrane review found that routine capnometry in PSA is associated with more interventions and no change in outcome, apart from a possible INCREASE in hypotension (probably because reassurance that you will pick up respiratory depression more reliably makes people more aggressive with medication).
Samuel G. Campbell
MB BCh, FCFP(EM), Dip PEC(SA), FCCHL.
Professor, Department of Emergency Medicine
Dalhousie University
Chief, Charles V. Keating Emergency and Trauma Centre
Queen Elizabeth II HSC
1796 Summer St, Halifax, Nova Scotia. B3H 3A7
Ph: 902-473 2020
Fax: 902-473 3617
I’d have to disagree with “Error #8: Adding an opioid with ketamine for sedation”. The cited study looked at level of analgesia and not level of procedural sedation.
Pingback: Länkar v24 | Internmedicin
[…] Vetter and Jesse Sturm have a great review of 10 procedural sedation errors made in the ED. […]
Pingback: PSA must read | SEH-LUMC.NL
Pingback: LITFL Review 231 • LITFL Medical Blog • FOAMed Review