Authors: Danae Massengill, MD (Medical Toxicology Fellowship Rocky Mountain Poison and Safety, Denver Health); Christine Murphy, MD (Atrium Health Emergency Department) // Reviewed by: James Dazhe Cao, MD (@JamesCaoMD, Associate Professor of EM, Medical Toxicology, UT Southwestern Medical Center, Dallas, TX); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Historical Case:
Over a 2-week period in November 2008, 13 cases of unexplained acute renal failure occurred among children from a hospital in Lagos State, Nigeria. Upon review of the history, several of the patients had been exposed to a liquid acetaminophen-based teething medication.1
Clinical Questions:
- When should a clinician suspect diethylene glycol (DEG) toxicity?
- What is the management of suspected or confirmed DEG toxicity?
- What are the public health implications of DEG toxicity?
Background:
- DEG is a clear, colorless, odorless liquid with a sweet taste.
- An industrial chemical used as a solvent, lubricant, or chemical intermediate, DEG is also found in automobile fluids, cleaning products, and canned heat cooking fuels.
- In mass poisoning cases, DEG has been substituted as a solvent in oral medications and in topical medicinal products.2
- Clinically significant toxicity has been reported from oral and topical exposures.2
- Patients with suspected or known DEG ingestions present a diagnostic and therapeutic challenge as the mechanisms of DEG toxicity in humans are not completely understood.
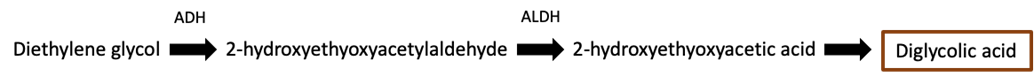
- Pharmacokinetics:2
-
- No minimal toxic dose has been established, however, doses up to 22 mg seem to be safe for adults from the available literature.
- DEG is rapidly absorbed when ingested and can reach peak plasma and brain tissue concentrations within four hours of ingestion.
- The majority of DEG is eliminated unchanged in the urine under normal physiologic conditions.
- However, up to 40% of DEG is metabolized to diglycolic acid (DGA) which is the proposed toxic metabolite of concern. DGA concentrates in the kidney tissue and causes nephrotoxicity, as well as neurotoxicity.
- Elimination half-life data is not well established but increases in larger overdoses and as renal injury begins to occur.
Epidemiology/Public Health Implications:
- Implicated in the Sulfanilamide Disaster of 1937, DEG toxicity was responsible for the death of 105 people across 15 states, one-third of which were children.4
- This disaster led to new standards of drug safety with the establishment of the Federal Food, Drug and Cosmetic Act of 1938.4
- Despite the policy changes in the United States, epidemic poisonings involving DEG continue to impact adults and children on a global scale with 14 mass poisonings occurring since the Sulfanilamide Disaster.5,6
- Unfortunately, most patients exposed to epidemic poisonings present after the onset of symptoms, at which point end-organ effects from toxicity have already started to occur and may not be reversible.
Clinical Presentation:
- Target organs of acute DEG toxicity are the kidney, liver, and nervous system.
- Toxicity typically evolves through three phases:2,3,7,8,9
- Phase 1: Gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea, and hepatotoxicity), elevated osm gap, and anion gap metabolic acidosis
- Phase 2: Acute oliguric or anuric renal failure secondary to acute tubular necrosis
- Acute kidney injury (AKI) is the hallmark of DEG toxicity.
- Phase 3: Neurologic complications, such as neuropathies, cranial nerve palsies, denervation, convulsions, encephalopathy, and coma
- Patients who develop AKI following DEG exposure are at risk for developing neurologic complications.
Diagnosis:
- Diagnosis without a clear history of exposure is very challenging.
- The clinician should rely on a high index of suspicion, clinical history and routine lab work including serum electrolytes, kidney function studies, and blood gas measurements.2
- Careful consideration should be given to the use of the osm gap, as this should not be used to exclude toxic alcohol ingestion.2
- Laboratory assays for DEG are not widely available and have long turn-around-times, thus have limited utility in diagnosis in the emergency department.
Management:
- While limited evidence supports gastrointestinal decontamination due to the severity of clinical effects following DEG exposure, it is reasonable to perform nasogastric/orogastric tube aspiration or give activated charcoal if patient presentation is within 1-2 hours of ingestion.2
- Administration of an alcohol dehydrogenase (ADH) inhibitor, such as fomepizole, is recommended in suspected or known DEG poisoning.
-
- The dosing of fomepizole is identical to that used for other toxic alcohols, with a loading dose of 15 mg/kg IV, followed 12 hours later by 10 mg/kg every 12 hours for 4 doses.2,10
- If patient requires hemodialysis, then the dosing interval should be every 4 hours.2,10
- Initial stabilization of DEG toxicity includes correcting acid-base abnormalities, electrolyte abnormalities, and volume resuscitation.
- Pay careful attention to fluid balance, as DEG has osmotic diuretic effects.
- Volume resuscitation as needed while adjusting for any developing acute kidney injury.
- Hemodialysis is indicated if there is evidence of acidosis or end-organ effects (acute kidney injury, coma, etc.)
- Renal injury often results in patients needing long-term hemodialysis.
- Inpatient/outpatient nerve conduction studies may be helpful in establishing the extent of neuropathy.
- Patients with suspected intoxication or asymptomatic patients with ingestions present the greatest challenge.
- These patients should be observed for at least 24 hours, following electrolytes and acid-base status closely for any changes.
- For patients receiving fomepizole, the 24-hour observation should begin 12 hours following the last dose of fomepizole.2
Case Follow-up:
- Following an investigation, the Nigeria Field Epidemiology and Laboratory Training Program (N-FELTP), CDC, and the Food and Drug Administration (FDA) identified 57 cases of DEG poisoning among children £ 3 years old, of whom 54 died.1
- Of the 57 children, 96% had confirmed exposures to the acetaminophen-based teething medication.
- Twenty-four of the 57 children identified underwent dialysis and two received fomepizole.
Clinical Pearls:
- DEG toxicity should be considered in cases of unexplained acute kidney, liver, or nervous system dysfunction, especially if occurring in outbreaks or clusters.
- Due to the limited availability of laboratory assays for DEG, clinicians should rely on a high index of suspicion, history, and routine lab work for diagnosing DEG toxicity.2
- Management of suspected or confirmed DEG toxicity encompasses a spectrum including observation, supportive care, ADH inhibitor therapy, and hemodialysis.2
- Contaminated pharmaceutical products should be included in the differential diagnosis of deaths of unknown origin.7
- Considering epidemiologic trends, the data suggest that DEG mass poisonings will continue to occur.
References:
- Abubukar et al. “Fatal Poisoning Among Young Children from Diethylene Glycol-Contaminated Acetaminophen — Nigeria, 2008—2009”. CDC’s Morbidity and Mortality Weekly Report. 11 Dec. 2009.
- Schier, Capt. Joshua G. “Diethylene Glycol” in Goldfrank’s Toxicologic Emergencies, 11e Eds. Lewis S. Nelson, et al. McGraw Hill, 2019. Accessed August 2022.
- Besenhofer, Lauren M., et al. “Inhibition of Metabolism of Diethylene Glycol Prevents Target Organ Toxicity in Rats.” Toxicological Sciences, vol. 117, no. 1, 2010, pp. 25–35., https://doi.org/10.1093/toxsci/kfq167.
- Ballentine, Carol. “Sulfanilamide Disaster.” FDA Consumer Magazine, June 1981, https://www.fda.gov/files/about%20fda/published/The-Sulfanilamide-Disaster.pdf. Accessed August 2022.
- Conklin, Laura, et al. “Long-Term Renal and Neurologic Outcomes among Survivors of Diethylene Glycol Poisoning.” JAMA Internal Medicine, vol. 174, no. 6, 1 June 2014, pp. 912–917. https://doi.org/10.1001/jamainternmed.2014.344.
- Bastani P, Jammeh A, Lamar F, Malenfant JH, Adewuyi P, Cavanaugh AM, Calloway K, Crisp C, Fofana N, Hallett TC, Jallow A, Muoneke U, Nyassi M, Thomas J, Troeschel A, Yard E, Yeh M, Bittaye M. Acute Kidney Injury Among Children Likely Associated with Diethylene Glycol-Contaminated Medications – The Gambia, June-September 2022. MMWR Morb Mortal Wkly Rep. 2023 Mar 3;72(9):217-222. doi: 10.15585/mmwr.mm7209a1. PMID: 36862590; PMCID: PMC9997663.
- O’Brien, Katherine L. “Epidemic of Pediatric Deaths from Acute Renal Failure Caused by Diethylene Glycol Poisoning.” JAMA, vol. 279, no. 15, 15 Apr. 1998, pp. 1175–1180., https://doi.org/10.1001/jama.279.15.1175.
- Robinson, Corie N., et al. “In-Vivo Evidence of Nephrotoxicity and Altered Hepatic Function in Rats Following Administration of Diglycolic Acid, a Metabolite of Diethylene Glycol.” Clinical Toxicology, vol. 55, no. 3, 11 Jan. 2017, pp. 196–205., https://doi.org/10.1080/15563650.2016.1271128.
- Schep, Leo J., et al. “Diethylene Glycol Poisoning.” Clinical Toxicology, vol. 47, no. 6, 8 July 2009, pp. 525–535., https://doi.org/10.1080/15563650903086444.
- Howland, Mary Ann. “Fomepizole” in Goldfrank’s Toxicologic Emergencies, 11e Eds. Lewis S. Nelson, et al. McGraw Hill, 2019. Accessed August 2022.








