Originally published on Ultrasound G.E.L. on 9/5/17 – Visit HERE to listen to accompanying PODCAST! Reposted with permission.
Follow Dr. Michael Prats, MD (@PratsEM), Dr. Creagh Bougler, MD (@CreaghB), and Dr. Jacob Avila, MD (@UltrasoundMD) from Ultrasound G.E.L. team!
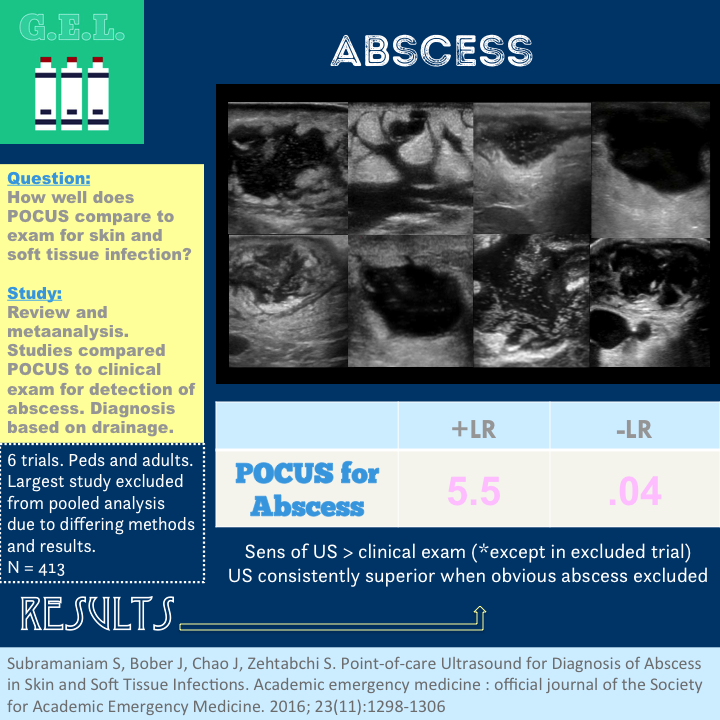
Point-of-care Ultrasound for Diagnosis of Abscess in Skin and Soft Tissue Infections
Academic Emergency Medicine November 2016 – Pubmed Link
Take Home Points
1. POCUS is more accurate than physical exam for distinguishing abscess from cellulitis in cases where abscess is not clinically evident.
2. POCUS has a negative likelihood ratio of 0.04 for identifying abscess (pooled data).
Background
Skin and soft tissue infections, which include cellulitis and abscess, are a common problem. It is important to distinguish between these two because treating cellulitis like an abscess could result in an unnecessary procedure (incision and drainage) whereas treating an abscess like cellulitis (antibiotics alone) could result in failure of treatment. Unfortunately, the physical exam has been shown to not be as good as we would like (as it has in many many cases). Luckily, ultrasound is pretty good at this. This is a systematic review and metaanalysis designed to see exactly how good it is.
Question
How well does ultrasound compare to clinical examination for the identification of abscess in patients with skin and soft tissue infection (SSTI)?
Population
Study populations varied as this was a review
Inclusion for studies:
- Compared clinical exam to ultrasound for detection of abscess in any age, in the emergency department
- Criterion standard for diagnosis must include pus drainage at incision or follow up
Exclusion for studies:
- Not in ED or using emergency physicians
- Included intraoral abscesses or abscess requiring drainage in operating room
Design
Systematic review and metaanalysis
Searched MEDLINE, web of science, CINAHL, EMBASE, Cochrane, ClinicalTrials.gov, Google Scholar, EBSCO, contacted experts, searched abstracts at major conferences, searched references of identified studies. Search originally through May 21, 2015. Updated January 1, 2016.
Heterogeneity calculated with DerSimonian and Laird’s Q test
Intervention
In these studies, point of care ultrasound for detecting an abscess was compared to confirmation of abscess by drainage of pus
Follow up ranged from 2 to 7 days
Who did the ultrasounds?
Varied by study
Some were describes as novices, others were POCUS credentialed, some did not say.
Training ranged from 30 minutes of combined didactic and hands-on training to 2 day course + 25 reviewed ultrasounds.
The Scan
Linear probe
Exact protocols likely varied by study.
Learn how to do soft tissue ultrasound! 5 min sono on Soft Tissue
Results
The Studies
6 trials included
- 800 aggregate patients
- 2005 to 2015, all from United States
- N ranged from 40 to 387
- 4 pediatrics, 2 adult papers (2 largest ones were pediatric, 67.3% of total population)
Heterogeneity – significant overall
- One study (the largest one by Marin, et al.) has significant different study design (see discussion below). With this removed, heterogeneity was not statistically significant
- Two studies compared clinical exam to clinical exam + POCUS instead of clinical exam alone to POCUS alone
Primary Outcome
N = 413 *with Marin trial excluded
Pooled Sensitivity = 97% (94-98%)
Pooled Specificity = 83% (75-88%)
+LR 5.5
-LR 0.04
Other Findings
In all studies except the Marin study, ultrasound was more sensitive than clinical exam below.
3/6 studies showed ultrasound more specific than clinical exam, the other half showed clinical exam was more specific.
In comparing the two studies looking at the not-clinically obvious population, the study with more rigorous training outperformed the other with less training
Limitations
Cellulitis could evolve into abscess – might count against POCUS (false negative) at follow up visit.
5/6 trials limited by having two reference standards. The follow up visit end point is biased because the suspicious ones were drained and small ones that weren’t might have resolved by this point. This would inflate the sensitivity and specificity.
All observational trials only.
Might have been better if they included studies that used clinical patient centered outcomes at follow up instead of strict definition of “drainage of pus”. This would reflect the “clinically significant” abscess that required drainage.
Other variables were not parsed out: size of abscess, location of abscess. Do these matter in determining how useful ultrasound is?
Discussion Points
The Marin study is worth mentioning because it really made the result difficult to interpret. It was the largest study included, and entirely pediatric. Unlike some of the others, this study did NOT exclude clinically obvious abscesses. This is the only study included that showed clinical exam to be superior in sensitivity and specificity to clinical exam plus POCUS. However, when they looked at the population of SSTIs that were not obvious, then POCUS was way better. It makes sense that if the answer is clinically obvious, ultrasound would not likely improve your accuracy in diagnosis.
Take Home Points
1. POCUS is more accurate than physical exam for distinguishing abscess from cellulitis in cases where abscess is not clinically evident.
2. POCUS has a negative likelihood ratio of 0.04 for identifying abscess (pooled data).
Our score