Author: Courtney Cassella, MD (@Corablacas, EM Resident Physician, Icahn SoM at Mount Sinai) // Edited by: Jamie Santistevan, MD (@Jamie_Rae_EMdoc, Admin and Quality Fellow at UW, Madison, WI) and Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW Medical Center / Parkland Memorial Hospital)
Clinical Case
A 32 year-old woman, with a past medical history of polycystic ovary syndrome, G1P0 pregnant at 6 weeks presents to the emergency department with pelvic pain for one day. She has 7/10 cramping pelvic pain, predominantly on the left side. This is a desired pregnancy conceived through IVF. Review of systems is positive for mild nausea but no vomiting. She denies fever, diarrhea, urinary complaints, vaginal bleeding, or vaginal discharge. Examination reveals normal vital signs; pelvic exam is notable for a closed os, physiologic discharge, and bilateral adnexal tenderness left greater than right.
Introduction
Assisted Reproductive Technologies (ART) are multiple techniques that allow gamete manipulation outside the body. Commonly we think of in vitro fertilization (IVF), defined as eggs fertilized by sperm outside the womb. ART is increasing in popularity. In 20131, there were ~160,000 ART procedures resulting in ~53,000 live births. Furthermore, 39% of patients who undergo egg retrieval will become pregnant with an intrauterine pregnancy and 82% will carry to term.2 Gynecologists specializing in reproductive endocrinology and infertility monitor ART patients closely. However, certain entities will bring these patients to the emergency department and it is important to understand the basics of ART and its complications.
Steps of IVF2
- Ovarian Stimulation
- Drugs used: Human menopausal Gonadotropin/hCG, FSH/hCG, clomiphene citrate, GnRH
- Oocyte retrieval
- Fertilization with capacitated sperm or intracytoplastmic sperm injection (ICSI)
- Embryo culture
- Embryo transfer
- Typically with 2 embryos
- Risks associated with ovarian stimulation
- Ovarian Hyperstimulation Syndrome
- Ovarian torsion from ovarian stimulation causing adnexal cysts/enlargement.
- For more information on ovarian torsion: http://www.emdocs.net/ovarian-torsion-pearls-and-pitfalls/
- Ovarian Cancer
- Surgical Risks
- General anesthetic
- Damage to other structures: 1 in 2500 retrievals
- Pelvic infection
- For more information on pelvic infections: http://www.emdocs.net/tubo-ovarian-abscess-pearls-pitfalls/
- Risks associated with pregnancy
- Multiple gestations
- Likelihood of twin pregnancy is 10% with clomid, 20-30% after IVF with 2 embryos, 10-20% after intrauterine implantation
- ~40% of ART conceived infants are twins1
- Ectopic and Heterotopic Pregnancies
- Miscarriage
- Preterm Birth and Low Birth Weight infants
- Multiple gestations
Ovarian Hyperstimulation Syndrome (OHSS)3
http://www.ultrasound-images.com/ovaries/
OHSS is a syndrome that occurs secondary to ovarian stimulation from infertility treatments. It is characterized by bilateral ovarian cysts. The syndrome can occur days to weeks following gonadotropin administration. Risk factors include <35 years old, polycystic ovarian syndrome, slender body habitus, multiple pregnancy, and hCG luteal supplementation. OHSS occurs in approximately 1 in 10 women undergoing IVF however the severity is variable. The incidence of the moderate form is 2-4 % and severe is 0.1-0.5%.4, 5 Table 1 demonstrates the presentation and symptoms of each severity level.

Physical Exam
- **Bimanual pelvic exam is contraindicated due to extreme fragility of ovaries that are high risk of rupture or hemorrhage => defer until after discussion with gynecology3
- Cardiac: Distant heart sounds (rarely) secondary to pericardial effusion
- Lung: Decreased breath sounds at the bases secondary to pleural effusions
- Distended abdomen +/- fluid wave, dull to percussion secondary to ascites
Work-up6
- Serum ß–hCG
- CBC – may demonstrate hemoconcentration (hematocrit >55%) or leukocytosis
- BMP – Evaluate renal function, may have hyponatremia or hyperkalemia
- LFT – Abnormal LFTs indicate severe OHSS
- PT/PTT/INR – Evaluate for coagulopathy
- EKG to evaluate for hyperkalemia (given renal failure and electrolyte abnormalities)
- Pelvic ultrasound–
- Findings may include
- Bilateral cystic ovaries, often enlarged
- Free fluid (ascites)
- Assess for ovarian torsion or ectopic
- Findings may include
Mild OHSS does not require any treatment as most symptoms resolve spontaneously in 1 week.6 Patients should have close follow-up and good return precautions. The mainstay of treatment for moderate to severe OHSS is supportive care with intravenous fluid resuscitation. Given the massive third spacing, one can consider colloid solution although this is controversial.7 In addition to basic care, prompt gynecology consultation is necessary. This is in part because the differential for OHSS includes ectopic or heterotopic pregnancy and the enlarged ovaries are at risk for torsion. Moderate to severe OHSS may have coagulopathy, ED physicians should consider work-up for thrombotic events or anticoagulation with heparin or enoxaparin (lovenox). The decision for anticoagulation should be made in conjunction with a specialist.4 OHSS patients, particularly those with moderate to severe symptoms require admission and consideration for intensive care.
Ectopic8, 9 and Heterotopic10-13 Pregnancies
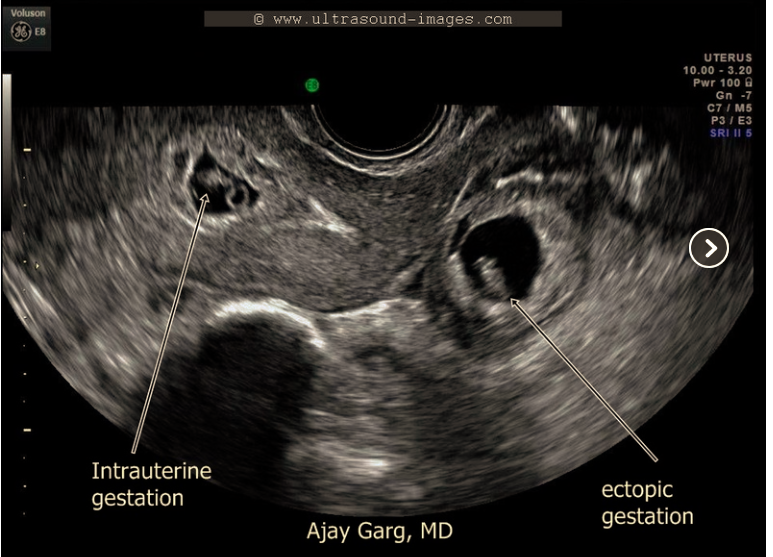
http://www.ultrasound-images.com/early-pregnancy/#HETEROTOPIC%20GESTATION
Ectopic pregnancy is when an embryo implants outside of the uterus. The population incidence is 2%14 and it is the leading cause of maternal death in the first trimester.15 For this reason, female patients of childbearing age presenting to the ED with pelvic pain, vaginal bleeding, and/or unstable vital signs should be evaluated for pregnancy and if pregnant, ectopic pregnancy.
Presentation
- Pelvic pain – suprapubic or lateralized
- Vaginal bleeding of any degree
- Amenorrhea
- Syncope
- Hypotension
- Tachycardia or bradycardia
ART doubles the risk of ectopic pregnancy.2 Therefore, ART is an important risk factor about which to ask patients when evaluating for ectopic pregnancy. Possible reasons for ectopic pregnancy after in vitro include misplaced catheter tip, too much force or volume used during embryo transfer, or retrograde transport of the embryo.16 Table 2 outlines risk factors for ectopic pregnancy17 as well as factors that increase the risk of ectopic in ART patients.18

Heterotopic pregnancy is concurrent intrauterine and ectopic pregnancies. Although rare overall, in ART patients the possibility is significantly greater.
The diagnosis of heterotopic pregnancy can be challenging as the usual evaluation for ectopic pregnancy, ultrasound and serum ß–hCG levels, demonstrates an expected rise in hCG and intrauterine pregnancy (IUP). Practitioners should maintain a high index of suspicion for heterotopic pregnancy in any ART patient.
Work-up of ectopic pregnancy should include a minimum of transabdominal and/or transvaginal ultrasound. Classically, if ultrasound demonstrates an IUP, ectopic pregnancy is excluded. However, evaluation for IUP alone is not sufficient in ART given the elevated risk of heterotopic pregnancy. For this reason ultrasound evaluation of the adnexa, most often performed by radiology or gynecology, is essential. Findings or signs that warrant urgent evaluation by gynecology, even in the presence of IUP, include free fluid in the abdomen, abnormal adnexa on ultrasound, or hemodynamic instability.10, 13
Work-up
- Serum ß–hCG
- CBC – Evaluate for anemia
- Type and Screen – determine Rh if vaginal bleeding
- BMP
- PT/PTT/INR
- Transabdominal and/or Transvaginal Ultrasound
- In ART, presence of IUP alone does not exclude ectopic pregnancy
In ART patients with suspected ectopic, early consultation with gynecology and obstetrics is essential. Treatment of heterotopic pregnancy is difficult because often the viable IUP is desired. Systemic therapy with methotrexate is not an option due to toxicity to the IUP. Management of heterotopic is difficult and at the discretion of the gynecologist. Hemodynamic instability warrants prompt surgical exploration.10, 13
Case Resolution
Bedside transvaginal ultrasound revealed an intrauterine pregnancy with trace free fluid. Given the history of ART, the patient was sent to radiology ultrasound and found to have multiple small (<1cm) follicles bilaterally and a complex adnexal mass on the left. Gynecology was promptly consulted for evaluation for heterotopic pregnancy or OHSS. The patient was taken to the OR and a heterotopic pregnancy was resected from the left adnexa.
Pearls and Pitfalls for ART Patients
- Complications bringing patients to the ED post ART include: pelvic infection, ovarian torsion, OHSS, ectopic/heterotopic pregnancy, and miscarriage
- Early consultation with gynecology may be helpful in all post-procedure or pregnant ART patients
- If suspecting OHSS defer pelvic examination until consultation with gynecology
- Severe OHSS is a life threatening syndrome requiring aggressive IVF resuscitation
- Beware of electrolyte abnormalities and coagulopathy in OHSS
- Presence of IUP alone does not exclude ectopic pregnancy in ART
- Obtain adnexal ultrasound to evaluate for ectopic in ART patients
- If IUP is visualized, free fluid in the abdomen, abnormal adnexa, or hemodynamic instability should prompt surgical exploration for heterotopic
References/Further Reading
- Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, et al. Assisted Reproductive Technology Surveillance – United States, 2013. Morbidity and mortality weekly report Surveillance summaries. 2015;64(11):1-25.
- Michalakis KG, DeCherney AH, Penzias AS. Assisted Reproductive Technologies: In Vitro Fertilization & Related Techniques. In: DeCherney AH, Nathan L, Laufer N, Roman AS, editors. CURRENT Diagnosis & Treatment: Obstetrics & Gynecology, 11e. New York, NY: McGraw-Hill; 2013.
- Waller N. Complications of Gynecologic Procedures. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM, editors. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. New York, NY: McGraw-Hill; 2016.
- Mor YS, Schenker JG. Ovarian hyperstimulation syndrome and thrombotic events. American journal of reproductive immunology. 2014;72(6):541-548.
- Rutkowski A, Dubinsky I. Ovarian hyperstimulation syndrome: imperatives for the emergency physician. The Journal of emergency medicine. 1999;17(4):669-672.
- Justice HM, Counselman FL. Ovarian hyperstimulation syndrome: an important complication of in vitro fertilization. The American journal of emergency medicine. 2008;26(1):115 e113-114.
- Youssef MA, Mourad S. Volume expanders for the prevention of ovarian hyperstimulation syndrome. The Cochrane database of systematic reviews. 2016;8:CD001302.
- Heaton HA. Ectopic Pregnancy and Emergencies in the First 20 weeks of Pregnancy. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM, editors. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. New York, NY: McGraw-Hill; 2016.
- Robertson J. Ectopic Pregnancy. emDocs. http://www.emdocs.net/ectopic-pregnancy/. Published 2014. Accessed August 25, 2016.
- Brunette DD, Roline C. Heterotopic pregnancy resulting from in vitro fertilization. The American journal of emergency medicine. 2011;29(8):960 e961-962.
- Maruotti GM, Sarno L, Morlando M, Sirico A, Martinelli P, Russo T. Heterotopic pregnancy: it is really a rare event? The importance to exclude it not only after in vitro fertilization but also in case of spontaneous conception. Fertility and sterility. 2010;94(3):e49; author reply e50.
- Richards SR, Stempel LE, Carlton BD. Heterotopic pregnancy: reappraisal of incidence. American journal of obstetrics and gynecology. 1982;142(7):928-930.
- Sucov A, Deveau L, Feola P, Sculli L. Heterotopic pregnancy after in vitro fertilization. The American journal of emergency medicine. 1995;13(6):641-643.
- Centers for Disease C, Prevention. Ectopic pregnancy–United States, 1990-1992. MMWR Morbidity and mortality weekly report. 1995;44(3):46-48.
- From the Centers for Disease Control and Prevention. Ectopic pregnancy–United States, 1990-1992. Jama. 1995;273(7):533.
- Svare J, Norup P, Grove Thomsen S, Hornnes P, Maigaard S, Helm P, et al. Heterotopic pregnancies after in-vitro fertilization and embryo transfer–a Danish survey. Human reproduction. 1993;8(1):116-118.
- Ankum WM, Mol BW, Van der Veen F, Bossuyt PM. Risk factors for ectopic pregnancy: a meta-analysis. Fertility and sterility. 1996;65(6):1093-1099.
- Perkins KM, Boulet SL, Kissin DM, Jamieson DJ, National ARTSG. Risk of ectopic pregnancy associated with assisted reproductive technology in the United States, 2001-2011. Obstetrics and gynecology. 2015;125(1):70-78.
- Donadio NF, Donadio N, Martins PT, Cambiaghi Cde G. [Heterotopic gestation: diagnostic possibility after in vitro fertilization. A case report]. Revista brasileira de ginecologia e obstetricia : revista da Federacao Brasileira das Sociedades de Ginecologia e Obstetricia. 2008;30(9):466-469.
- De VR, Pratt JH. Simultaneous intrauterine and extra-uterine pregnancy. Proceedings of the staff meetings Mayo Clinic. 1948;23(7):166-168.










