Author: Rachel Bridwell, MD (EM Resident Physician, San Antonio, TX) // Edited by: Brit Long, MD (@long_brit, EM Attending Physician, San Antonio, TX) and Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 31-year-old male presents for headache for the past 72 hours. He has a history of tension headaches, but confirms that this headache feels different, worse when he bends over. Collateral information from a friend is notable for a seizure yesterday, but the patient refused to come in at that time. He states that he has been non-compliant with his ART, and his last known CD4 count one month prior was 200. Review of systems is remarkable for 15 lb unintentional weight loss in the past month.
Triage vital signs (VS): BP 105/60, HR 103, T 100.2 temporal, RR 24, SpO2 98% on room air.
Pertinent physical examination findings:
General: Alert and oriented x 2, stuporous
Eyes: Extraocular movements intact, PERL, photophobia
Fundoscopic exam: increased cup to disc ratio
CV: Tachycardic, no murmurs, rubs, or gallops.
Pulmonary: Eupneic, lungs clear to auscultation bilaterally
Neuro: Noted motor deficit of RUE and RLE, gait instability, CN notable for VII right sided weakness and noted loss of right nasolabial folds
What could be going on, and what’s the next step in your evaluation and treatment?
Answer: CNS Toxoplasmosis1-14
- Background: Caused by Toxoplasma gondii, an obligate intracellular protozoan which multiplies in the intestines of cats. Oocyts are excreted in cat feces, which can invade hosts and form tissue cysts1
- Epidemiology:
- Risk Factors: Patients with HIV not diagnosed, not on ART, or non-compliant with ART, Also those with AIDS
- Toxoplasmosis: Most common CNS manifestation in AIDS1
- Undercooked meat, cat feces
- TB: Increased risk of infection at all CD4 counts
- 5-9% AIDS patients are infected with TB, of whom 2-18% develop CNS manifestations2
- CNS TB has 70% mortality rate2
- 5-9% AIDS patients are infected with TB, of whom 2-18% develop CNS manifestations2
- Toxoplasmosis: Most common CNS manifestation in AIDS1
- See Table 1 for risk factors for each CNS manifestation
- Risk Factors: Patients with HIV not diagnosed, not on ART, or non-compliant with ART, Also those with AIDS
- Clinical Presentation:
- Headache—any new or different headache in an individual with known HIV seropositive status should undergo CT and LP to evaluate
- One study of 110 HIV+ presenting to ED, new seizure, depressed or altered orientation, HA different in quality or > 3 days, head CT sensitivity 100% on finding new focal lesions3
- Personality changes, focal neurologic deficit, seizures, altered mental status, movement disorders
- Headache—any new or different headache in an individual with known HIV seropositive status should undergo CT and LP to evaluate
- Evaluation:
- Assess ABCs and VS
- May show fever, tachycardia, hypotension, but due to immunosuppression, signs of infection may be absent
- Perform a complete physical examination.
- Ocular: CN palsies may be seen, papilledema,
- Neuro: Focal neurologic deficits, CN palsies, movement disorders
- Integumentary: other signs of opportunistic infection may be present e.g. Kaposi Sarcoma
- ENT: Look for candidiasis, which may extend further with odynophagia and esophageal involvement
- Imaging: CT with contrast prior to LP to evaluate for mass effect and diagnosis (See Table 1)
- Mass effect: CNS lymphoma, toxoplasmosis, tuberculoma, abscess
- Laboratory evaluation:
- CBC with differential, renal/liver function, VBG with lactate, CD4 count, blood cultures x 2
- CD4 proxy: ALC = WBC x % lymphocytes4
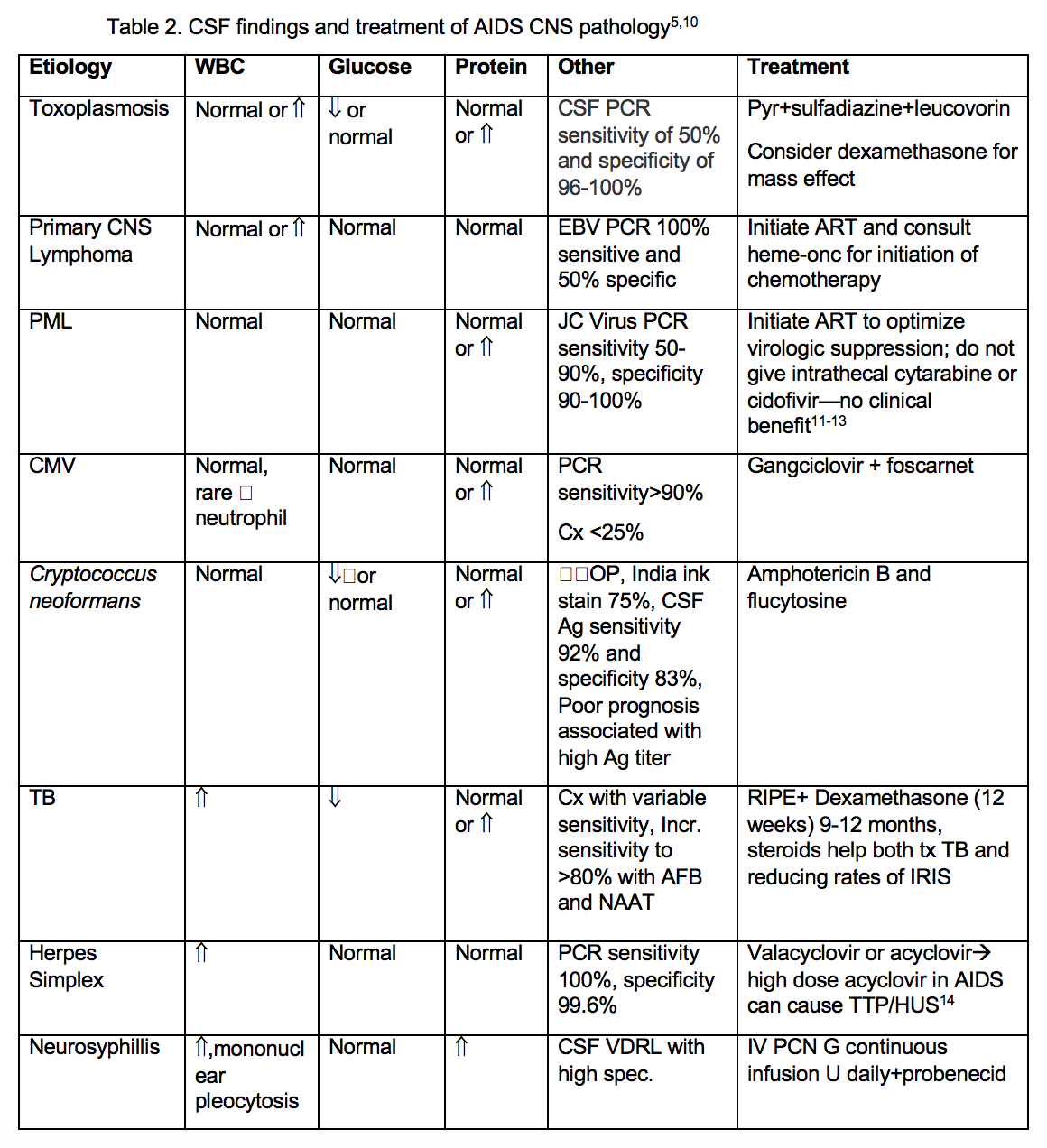
- LP—Cytology, glucose, protein, Gram stain, culture opening pressure, specific antigens—See table 2
- Toxoplasmosis: serum PCR sensitivity 80% and specificity 90%5
- Cryptococcus: India Ink and Cryptococcus antigen
- PML: JC virus CSF PCR, sensitivity dropped from 90% to 58% in HAART era2
- CBC with differential, renal/liver function, VBG with lactate, CD4 count, blood cultures x 2
- Assess ABCs and VS
- Treatment:
- ABCs—ensure detailed neuro exam prior to intubation
- Early and broad-spectrum antibiotics, antifungals, antivirals
- Toxoplasmosis—Pyrimethamine and sulfadiazine, folinic acid 10 mg; Consider dexamethasone for edema or mass effect
- If immunosuppressed, use bactrim or pyrimethamine with another agent
- Primary CNS lymphoma—Chemotherapy
- Cryptococcal meningitis—Amphotericin B and Flucytosine
- See Table 2 for more comprehensive etiology specific treatment
- Toxoplasmosis—Pyrimethamine and sulfadiazine, folinic acid 10 mg; Consider dexamethasone for edema or mass effect
- Steroids
- If administered in primary CNS lymphoma, may obscure histologic diagnosis6
- Increases mortality in Cryptococcal meningitis/encephalitis6
- Resuscitation and pain control
- Admit to ICU
- Infectious Disease consult
- Immune Reconstitution Inflammatory Syndrome (IRIS) – Paradoxical worsening of clinical status with initiation of ART as immune system reactivates and begins to fight a previously acquired infection (often opportunistic)7
- Can mimic ARDS
- Significant morbidity and mortality in CNS TB, estimated to approach 20%8
- Cryptococcal CNS IRIS estimated to be 2-20%7,9
- Consider Neurosurgery consult
- Definitive dx may require biopsy for definitive
- Pearls:
- CT with contrast prior to LP in a position to assess opening pressure
- CD4 count estimation from absolute lymphocyte count (ALC)
- ALC < 1200 correlates to CD4 count < 200, SN 72.7% and SP 100%4
- ALC > 2000 predicts CD4 count > 200



A 54-year-old man with a history of HIV and recent CD4 count of 85 presents with headache for 3 days. The patient’s sister says that he has been increasingly confused over the last 3 days. While in the Emergency Department, he has a seizure which resolves spontaneously. Electrolytes are within normal limits. A CT scan is performed and is shown above. Which of the following medication regimens should be given?
A) Amphotericin B
B) Ganciclovir and foscarnet
C) Pyrimethamine, sulfadiazine and leucovorin
D) Trimethoprim-sulfamethoxazole
Answer: C
The patient has toxoplasmosis, an opportunistic infection caused by the parasite Toxoplasma gondii. Patients at risk are those who are immunocompromised or have CD4 counts less than 100. Patients experience headache, confusion, lethargy and seizures. CT scan of the head reveals multiple, subcortical, ring-enhancing lesions. The lesions are usually present on non-contrast enhanced CT, but if clinical suspicion is high, a CT with contrast should be performed to increase detection. Definitive diagnosis requires a brain biopsy, however, treatment is recommended in patients with a compatible clinical presentation and CT findings. Empiric treatment for toxoplasmosis is pyrimethamine, sulfadiazine and leucovorin. CNS lymphoma also causes ring-enhancing lesions in patients with AIDS. However, the lesions are usually solitary and located in the periventricular white matter. In addition, symptoms in these patients are usually gradually progressive over months rather than days as in this patient.
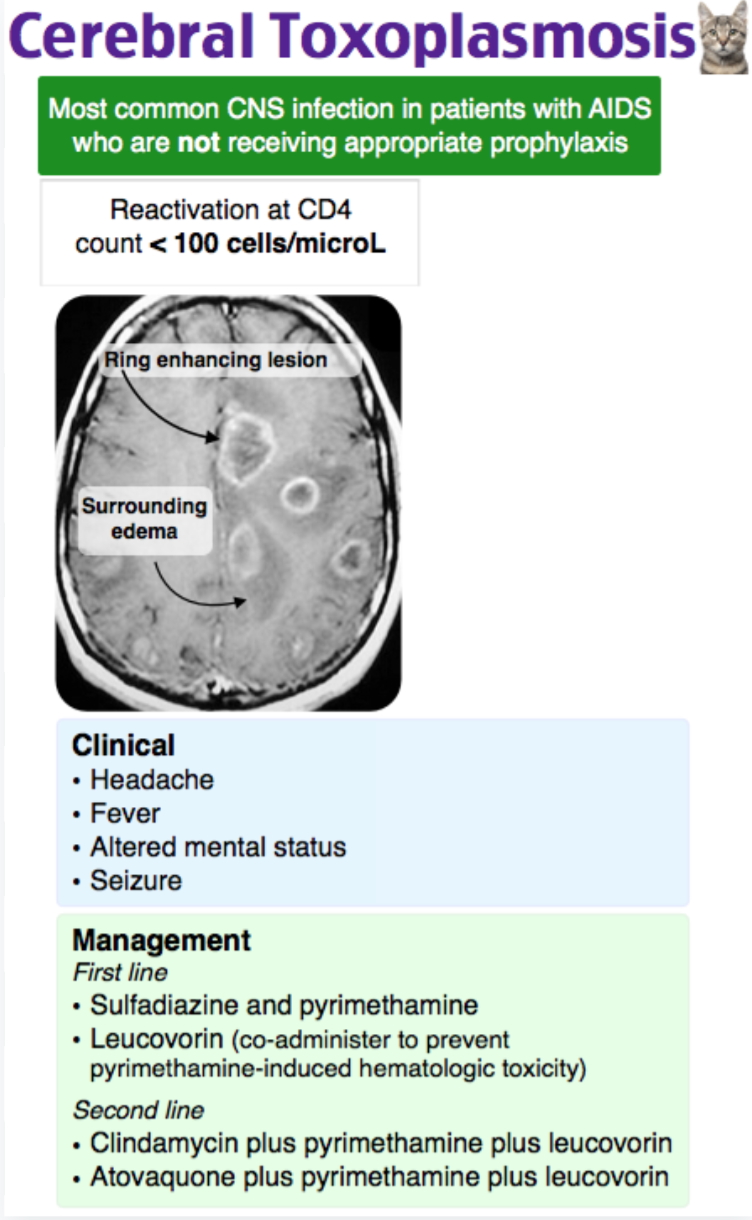
Amphotericin B (A) is the treatment for cryptococcal meningitis. In this condition, the head CT is usually normal, and a lumbar puncture demonstrates leukocytosis and a positive cryptococcal antigen. Ganciclovir and foscarnet (B) combination therapy is the treatment for CMV retinitis or encephalitis. CMV encephalitis usually causes multifocal micronodules and ventriculoencephalitis on MRI. Trimethoprim-sulfamethoxazole (D) or dapsone with folinic acid are regimens for chronic suppression of toxoplasmosis to prevent relapse after initial treatment, but are not indicated for acute management.
FOAMed:
References:
- Bowen LN, Smith B, Reich D, Quezado M, Nath A. HIV-associated opportunistic CNS infections: pathophysiology, diagnosis and treatment. Nat rev Neurol.2016 Oct 27;12(11):662-674.
- Smith AB, Smirniotopoulos JG, Rushing EJ. Central Nervous System Infections Associated with Human Immunodeficiency Virus Infection: Radiologic-Pathologic Correlation. RSNA 2008; 28(7): 2033-59.
- Rothman RE, Keyl PM, McArthur JC, Beauchamp NJ Jr, Danyluk T, Kelen GD. A decisionguidelinefor emergency department utilization of noncontrast head computedtomography in HIV-infected patients. Acad Emerg Med. 1999 Oct;6(10):1010-9.
- Obirikorang C et al. Total Lymphocyte Count as a Surrogate Marker for CD4 Count in Resource-Limited. BMC Infectious Diseases Journal 2012; 12 (128): 1 – 5.
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medical Association of the Infectious Diseases Society of America. Available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed Sep 22 2018.
- Marx, J. A., & Rosen, P. (2017). Rosen’s emergency medicine: Concepts and clinical practice(9th ed.). Philadelphia, PA: Elsevier/Saunders.
- Akgün KM, Huang L, Morris A, Justice AC, Pisani M, Crothers K. Critical illness in HIV-infected patients in the era of combination antiretroviral therapy. Proc Am Thorac Soc. 2011 Jun;8(3):301-7.
- Muller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger M. Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: a systematic review and meta-analysis. Lancet Infect Dis 2010;10:251–261.
- Manosuthi W, Kiertiburanakul S, Phoorisri T, Sungkanuparph S, Manosuthi W, Kiertiburanakul S, et al. Immune reconstitution inflammatory syndrome of tuberculosis among HIV-infected patients receiving antituberculous and antiretroviral therapy. Journal of Infection. 2006;53(6):357–63.
- Tan IL, Smith BR, Von Geldern G, Mateen FJ, McArthur JC. HIV-associated infections of the CNS. Lan Neur. 2012; 11(7): 605-617.
- Hall CD, Dafni U, Simpson D, et al. Failure of cytarabine in progressive multifocal leukoencephalopathy associated with human immunodeficiency virus infection. AIDS Clinical Trials Group 243 Team. N Engl J Med. May 7 1998;338(19):1345-1351.
- Gasnault J, Kousignian P, Kahraman M, et al. Cidofovir in AIDS-associated progressive multifocal leukoencephalopathy: a monocenter observational study with clinical and JC virus load monitoring. J Neurovirol. Aug 2001;7(4):375-381.
- Lima MA, Bernal-Cano F, Clifford DB, Gandhi RT, Koralnik IJ. Clinical outcome of long-term survivors of progressive multifocal leukoencephalopathy. J Neurol Neurosurg Psychiatry. Aug 14 2010.
- Bell WR, Chulay JD, Feinberg JE. Manifestations resembling thrombotic microangiopathy in patients with advanced human immunodeficiency virus (HIV) disease in a cytomegalovirus prophylaxis trial (ACTG 204). Medicine (Baltimore). Sep 1997;76(5):369-380.








