A 61-year-old male with a history of bilateral corneal transplants due to Fuchs’ endothelial dystrophy arrives at the emergency department (ED), reporting progressive visual decline in his right eye over the past three days. He describes associated redness, photophobia, and mild foreign body sensation. He denies trauma but acknowledges inconsistent use of his prescribed steroid eye drops.
Physical Exam Findings:
- Visual Acuity: 20/60 in the right eye (previously 20/30), 20/25 in the left eye.
- External Exam: Mild conjunctival redness, absence of purulent discharge.
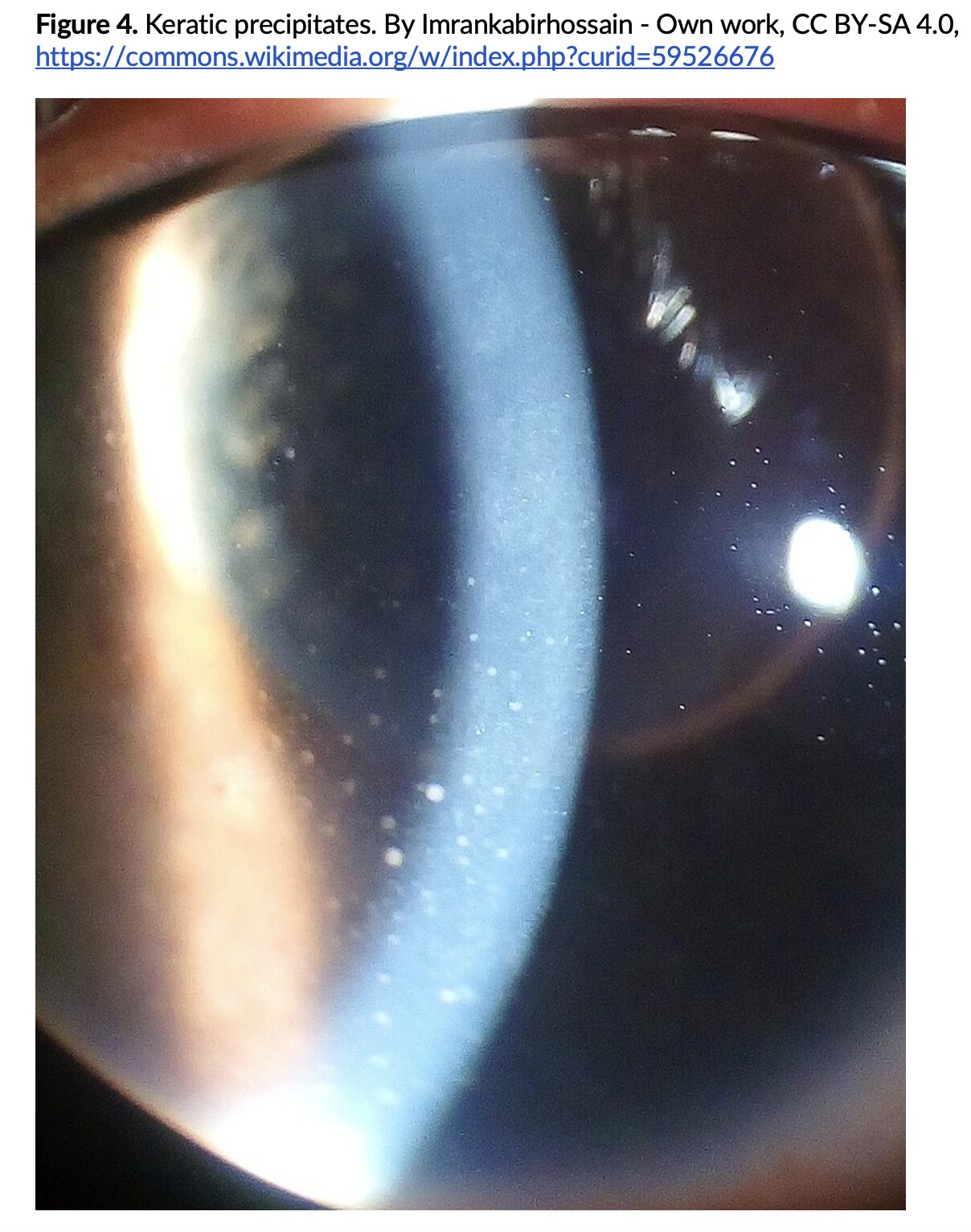
- Slit-Lamp Exam: Corneal swelling with scattered keratic precipitates, mild anterior chamber inflammation.
- Intraocular pressure (IOP): 18 mmHg (right eye), 14 mmHg (left eye).
Question: What is the diagnosis?
Answer: Corneal graft rejection
Background:
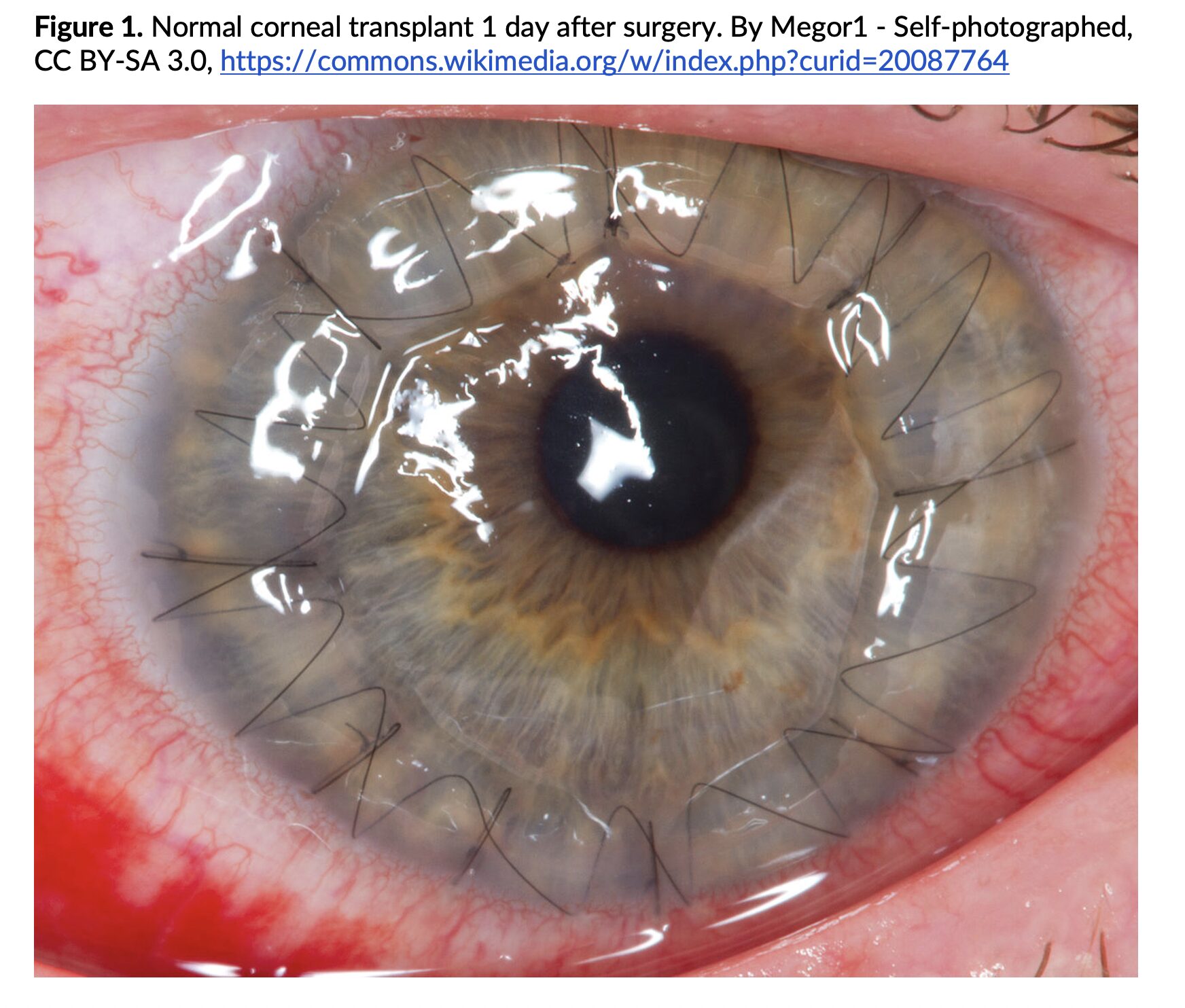
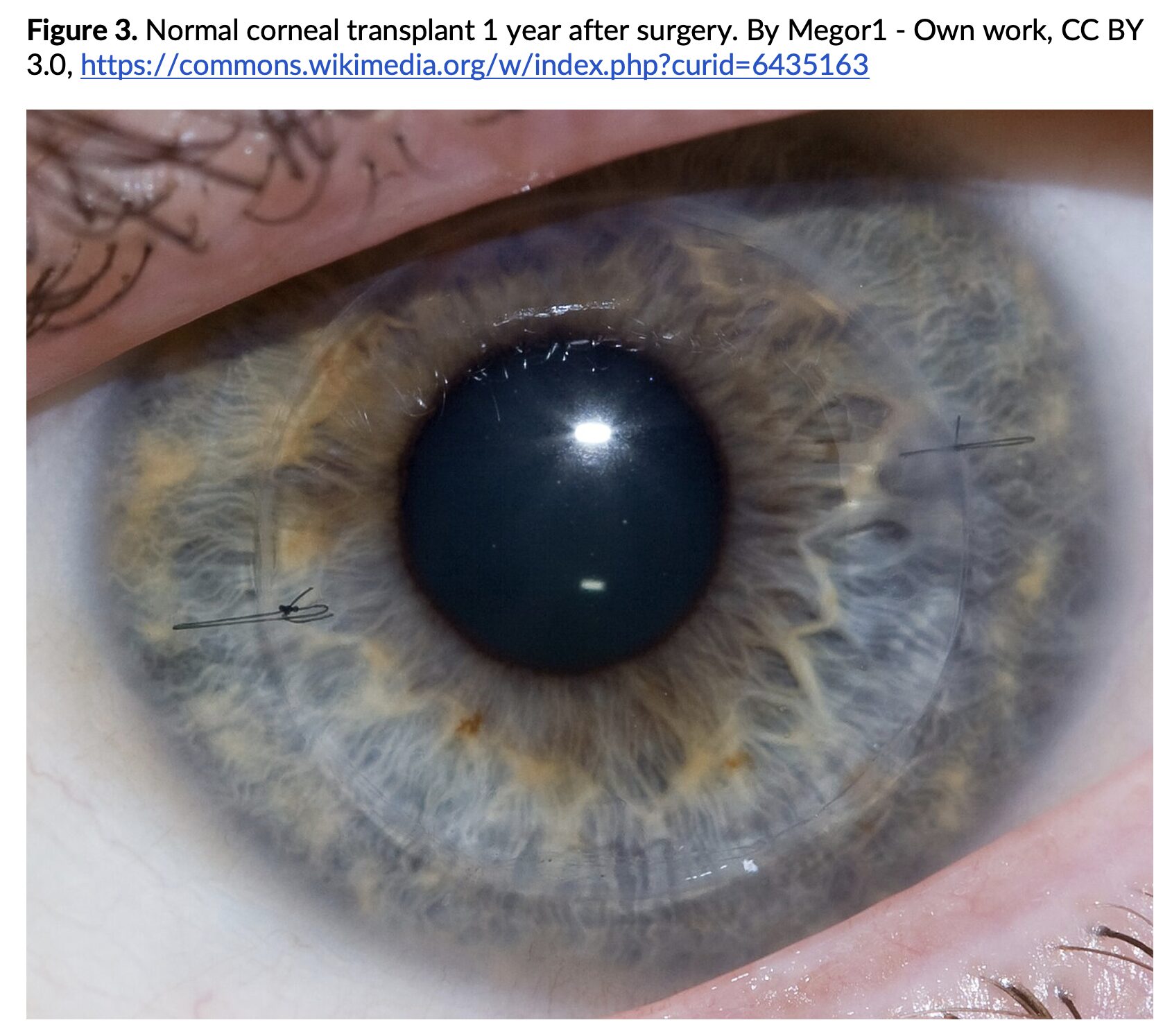
- Corneal transplantation, also known as keratoplasty, is a widely utilized surgical procedure aimed at restoring vision in individuals with corneal diseases.1
- What is it: surgical procedure in which a diseased or damaged cornea is replaced with donor corneal tissue from an eye bank.2
- Most common technique is penetrating keratoplasty (PK) = entire thickness of the central cornea is removed using a trephine and replaced with a full-thickness donor graft sutured into place.3
- Lamellar techniques such as Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) and Descemet Membrane Endothelial Keratoplasty (DMEK) selectively replace only the posterior layers of the cornea (endothelium and Descemet’s membrane), preserving anterior stromal integrity.3,4
- These modern techniques offer faster recovery times, lower rejection risk, and better visual outcomes for endothelial disorders like Fuchs’ dystrophy.3,4
- Despite its high success rate, complications may arise post-operatively that warrant ED evaluation.
Epidemiology:
- Corneal transplantation is one of the most frequently performed solid tissue transplants, with 50,925 procedures performed in 2023.5
- Penetrating keratoplasty (PK) has a one-year graft survival rate exceeding 90%, though outcomes vary depending on the underlying diagnosis.6
- Common indications include keratoconus, Fuchs’ endothelial dystrophy, corneal scarring, and infectious keratitis.1
- Graft rejection occurs in approximately 10–20% of transplant recipients, with higher rates in high-risk cases (vascularized corneas, previous graft failure).6
Evaluation:
- A meticulous eye exam is vital in identifying post-transplant complications. Key aspects include:
- Visual Acuity Testing: Detects changes suggestive of graft failure or rejection.
- External Inspection: Evaluates for infection signs, discharge, or conjunctival redness.
- Slit-Lamp Examination:
- Determines corneal clarity and presence of edema or infiltrates.
- Identifies keratic precipitates (Fig. 4) indicative of inflammation or rejection.
- Assesses the anterior chamber for cell/flare, hypopyon, or fibrin.
- Inspects sutures for possible loosening, breakage, or irritation.
- IOP Measurement: Detects elevated IOP, commonly associated with steroid use.7
- Fluorescein Staining: Identifies epithelial damage, wound separation, or recurrent erosions.
Clinical Presentation and Management by Etiology:
Early Postoperative Complications
- Graft Failure8
- Primary failure results from surgical trauma or endothelial dysfunction.
- Symptoms: Persistent blurred vision, corneal edema.
- Management: Emergent ophthalmology consultation, may require repeat keratoplasty.
- Infection (Endophthalmitis or Keratitis)9
- Can be bacterial, fungal, or viral and threaten graft survival.
- Symptoms: Pain, photophobia, decreased vision, hypopyon.
- Management: Emergent ophthalmology consultation, cultures, and intravitreal antibiotics.
- Elevated IOP/Glaucoma7
- Steroids post-op may increase IOP, risking optic nerve damage.
- Symptoms: Ocular pressure, headache, visual blurring.
- Management: Emergent ophthalmology consultation, initiate IOP-lowering agents.
Late Postoperative Complications
- Graft Rejection6,10
- Can occur weeks to years after surgery.
- Symptoms: Redness, photophobia, blurry vision, FB sensation.
- Signs: Corneal edema, keratic precipitates, anterior chamber reaction.
- Management: High-dose topical corticosteroids and urgent ophthalmology involvement.
- Suture-Related Issues/Wound Dehiscence11
- Sutures may become loose or cause mechanical irritation.
- Symptoms: FB sensation, redness, irritation.
- Management: Artificial tears, protective eyewear, ophthalmologic assessment.
- Recurrence of Primary Disease1
- Underlying corneal pathology such as Fuchs’ or keratoconus may recur and require intervention.
Prognosis:
- Graft survival rates are highest within the first year post-transplant but decline over time due to immunologic or mechanical factors.
- Long-term success is strongly influenced by the indication for transplant, patient adherence to medications (particularly corticosteroids), and early detection of complications.¹-⁴
- Prompt treatment of graft rejection can often restore graft clarity and preserve vision, particularly when initiated within days of symptom onset.⁶
Pearls:
- Always consider graft rejection in a transplant patient presenting with photophobia, vision changes, or redness — even years post-op.
- Inconsistent steroid use is a major contributor to late-onset rejection.
- Slit-lamp findings such as keratic precipitates and anterior chamber inflammation are key indicators of rejection.
- Elevated IOP may occur silently; always assess pressures, particularly if patients are on topical steroids.
- Early ophthalmology consultation significantly improves outcomes.

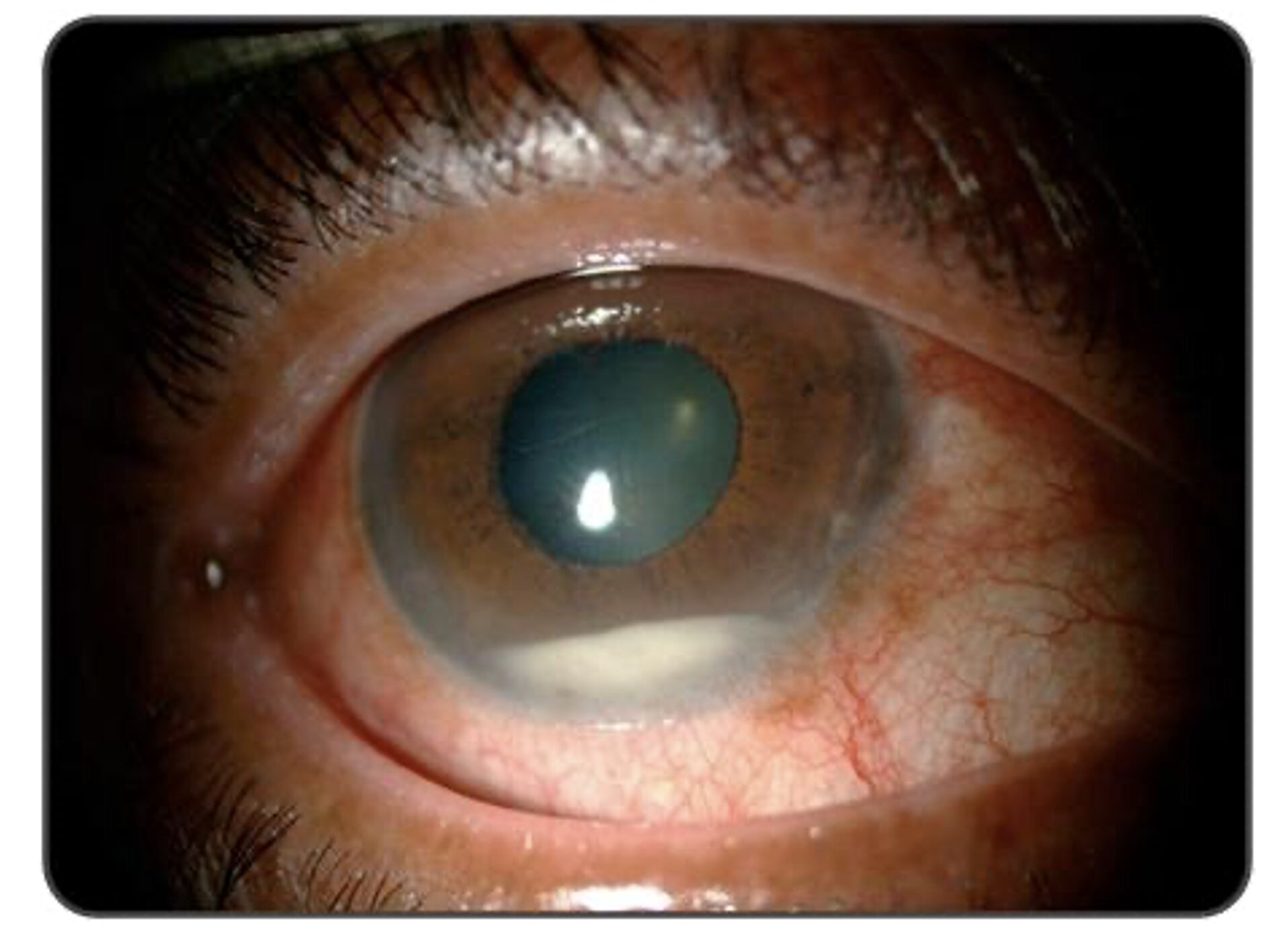
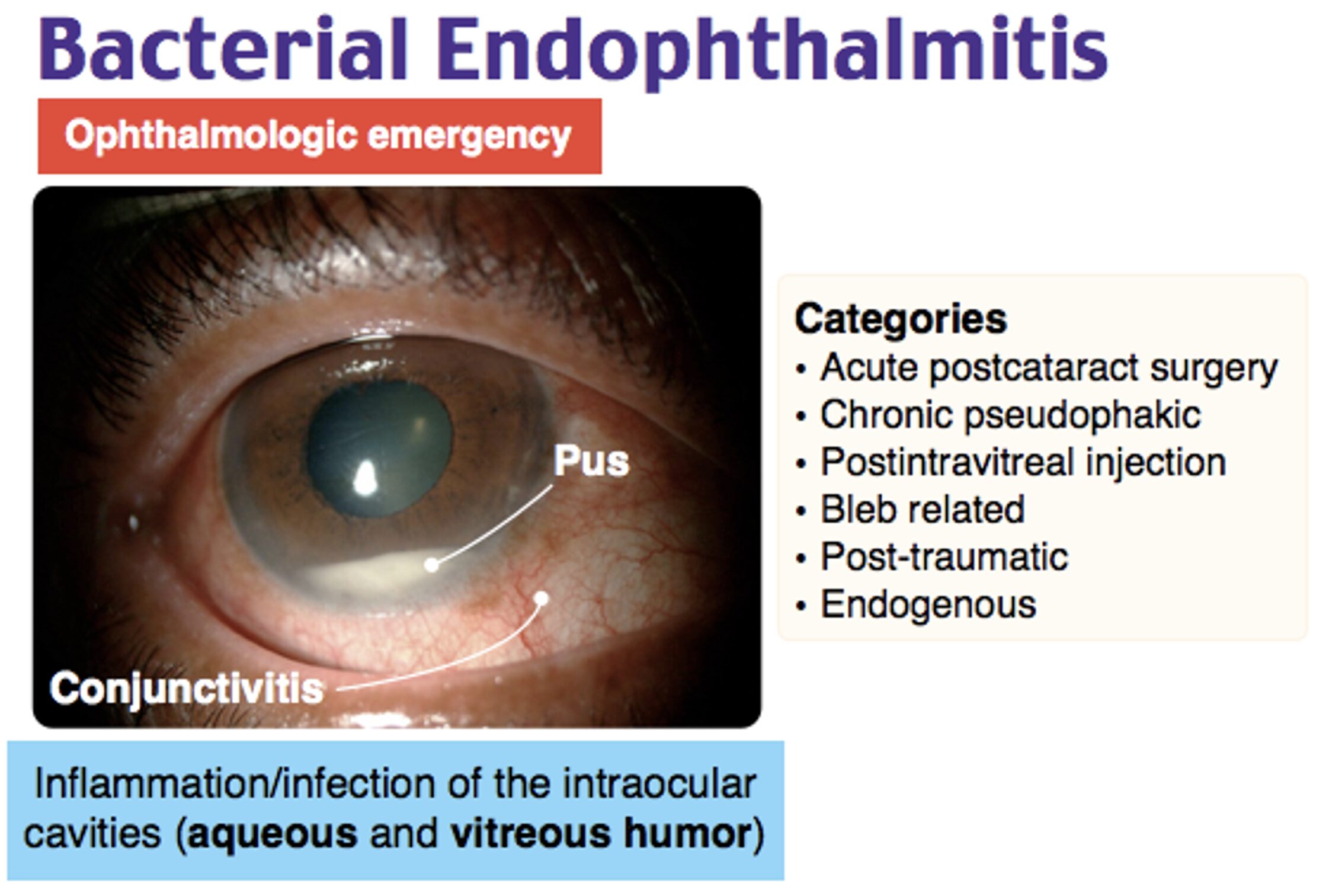
A 72-year-old man presents with a painful red eye and visual loss worsening over the last 24 hours. He recently had cataract surgery. Examination of the eye reveals the image above. Which of the following is the most likely diagnosis?
Acute angle closure glaucoma
A) Bacterial keratitis
B) Endophthalmitis
C) Hyphema
D) Traumatic iritis
Correct answer: B
This patient’s presentation of pain, progressive vision loss, eye redness, and hypopyon (yellow layering in the anterior chamber) is highly suggestive of postoperative endophthalmitis, a serious intraocular infection that occurs after intraocular surgery, most commonly cataract surgery. The rapid progression within 24 hours is characteristic of acute post-surgical bacterial endophthalmitis, which is most often caused by coagulase-negative Staphylococcus, Staphylococcus aureus, or Streptococcus species.
Endophthalmitis is caused by microbial invasion of the intraocular spaces, leading to a severe inflammatory response with purulent accumulation. Risk factors include recent intraocular surgery, wound leaks, immunosuppression, and contaminated surgical instruments or intraocular lenses. Patients classically present with eye pain, photophobia, conjunctival injection, corneal edema, hypopyon, and decreased visual acuity. The hallmark feature, hypopyon, represents inflammatory exudate pooling in the anterior chamber and is a key diagnostic clue.
Diagnosis is clinical but confirmed with aqueous or vitreous tap cultures. Emergency department management includes urgent ophthalmology consultation, intravitreal antibiotics (vancomycin plus ceftazidime), and possible vitrectomy in severe cases. Prompt treatment is crucial to prevent complications such as retinal detachment, phthisis bulbi, and permanent blindness.
Acute angle-closure glaucoma (A) can present with eye pain and vision loss, but it is distinguished by a fixed, mid-dilated pupil, a cloudy cornea, and elevated intraocular pressure. Hypopyon is not a feature of glaucoma.
Bacterial keratitis (B) involves corneal ulceration, fluorescein uptake, and stromal infiltrates, often following contact lens use or trauma. Unlike endophthalmitis, bacterial keratitis does not typically present with hypopyon unless it is severe.
A hyphema (D) is blood in the anterior chamber, usually caused by trauma. When the patient is in an upright position, blood will layer along the inferior aspect of the anterior chamber. As the hyphema increases in size, it elevates intraocular pressure. In some cases, admission is warranted for patients with large hyphemas (> 50%), decreased vision, sickle cell disease, and elevated intraocular pressure. Treatment is aimed at decreasing pressure with topical (beta-blocker, alpha agonist, or carbonic anhydrase inhibitors) and systemic therapy (carbonic anhydrase inhibitor, mannitol).
Traumatic iritis (E) occurs after blunt trauma in which the iris and ciliary body are inflamed causing ciliary spasm. Patients report significant photophobia and eye pain. Examination of the eye reveals perilimbal conjunctival injection (also called ciliary flush) and a small, poorly dilating pupil. Photophobia occurs when light is shone on both the affected and unaffected eye. On slit lamp exam, cells (white and red) and flare (protein) are noted in the anterior chamber. Treatment is with a topical cycloplegic agent to minimize spasm.
Further Reading
Further FOAMed:
- https://www.emdocs.net/emin5-slit-lamp-anatomy/
- https://timroot.com/slit-lamp-exam-video/
- https://www.emdocs.net/em3am-corneal-ulcer/
- https://www.emdocs.net/em3am-corneal-abrasion/
- https://www.emdocs.net/approach-to-the-red-eye/
- https://www.emdocs.net/ophthalmologic-medications-pearls-pitfalls-for-the-ed/
- https://www.emdocs.net/8578-2/
References:
- Dana MR, Qian Y, Hamrah P. Twenty-five–Year Panorama of Corneal Immunology: Emerging Concepts in the Immunopathogenesis of Microbial Keratitis, Peripheral Ulcerative Keratitis, and Corneal Transplant Rejection. Cornea. 2000;19(5):625-643. doi:10.1097/00003226-200009000-00008
- Zafar S, Wang P, Woreta FA, et al. Postoperative Complications in Medicare Beneficiaries Following Endothelial Keratoplasty Surgery. Am J Ophthalmol. 2020;219:1-11. doi:10.1016/j.ajo.2020.05.033
- Gorovoy MS. Descemet-Stripping Automated Endothelial Keratoplasty. Cornea. 2006;25(8):886-889. doi:10.1097/01.ico.0000214224.90743.01
- Guerra FP, Anshu A, Price MO, Giebel AW, Price FW. Descemet’s Membrane Endothelial Keratoplasty. Ophthalmology. 2011;118(12):2368-2373. doi:10.1016/j.ophtha.2011.06.002
- Eye Bank Association of America. 2023 Eye Banking Statistical Report. Accessed April 11, 2025. https://restoresight.org/members/publications/statistical-report/
- Thompson RW, Price MO, Bowers PJ, Price FW. Long-term graft survival after penetrating keratoplasty. Ophthalmology. 2003;110(7):1396-1402. doi:10.1016/S0161-6420(03)00463-9
- Wu S, Xu J. Incidence and risk factors for post-penetrating keratoplasty glaucoma: A systematic review and meta-analysis. Ahmad A, ed. PLOS ONE. 2017;12(4):e0176261. doi:10.1371/journal.pone.0176261
- Cohen EJ, Brady SE, Leavitt K, et al. Pseudophakic bullous keratopathy. Am J Ophthalmol. 1988;106(3):264-269. doi:10.1016/0002-9394(88)90359-5
- Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19(3):227-234. doi:10.1111/1469-0691.12118
- Lam H, Dana MR. Corneal graft rejection. Int Ophthalmol Clin. 2009;49(1):31-41. doi:10.1097/IIO.0b013e3181924e23
- Pagano L, Shah H, Al Ibrahim O, et al. Update on Suture Techniques in Corneal Transplantation: A Systematic Review. J Clin Med. 2022;11(4):1078. doi:10.3390/jcm11041078






