Featured on #FOAMED REVIEW 34TH EDITION – Thank you to Michael Macias from emCurious for the shout out!
Featured on the LITFL Review #169 – Thanks to Simon Laing (@HEFTEMCAST) and the LITFL Review group for the shout out!
Authors: Kirsten Morrissey, MD & Hilary E. Fairbrother, MD, MPH, FACEP // Edited by: Jennifer Robertson, MD and Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Background
In the United States, injury remains the leading cause of death and disability in children (1). Based on data from the National Trauma Database, the leading mechanisms of injury were falls in children 0-9 years of age, and motor vehicle collisions (MVCs) in children ages 10-18 (1). Overall, MVCs accounted for more than 60% of trauma-related deaths in children under age 18. Although blunt trauma accounts for the majority of pediatric injury, in children without insurance or with public insurance penetrating trauma accounted for 21% of injuries among adolescents (1).
While the general ATLS approach to trauma is similar in both adults and pediatrics, there are anatomic and physiologic differences to consider in the pediatric trauma patient. The goal for this article is to discuss these differences as we review pearls and pitfalls of pediatric trauma.
ABCDE and beyond…
Airway and Breathing
Airway remains the priority in the initial assessment. However, there are a few important considerations in the pediatric population.
- Children become hypoxemic more quickly than adults and may require more rapid intervention.
- A young child will also have a larger tongue, a more floppy epiglottis, and a larger head.
- Infants are obligate nasal breathers, which is an important consideration with facial trauma.
- Unlike adults, the cricoid cartilage in children is the narrowest part of the airway. Use of a shoulder roll, an oral airway, a smaller size ET tube, and a straight blade in younger patient may assist you with intubation (3).
- A needle cricothyrotomy should be performed in children under 8 years of age rather than a surgical cricothyrotomy.
- As long as appropriate cuff pressures are used, a cuffed ET tube may be used in ages outside of the newborn period (3).
Circulation
The circulating blood volume in a pediatric patient is approximately 70-80 ml/kg. It is important to remember that children remain normotensive for a longer period of time and may sustain significant blood loss before developing hypotension. Early compensatory measures include elevated heart rate and systemic vascular resistance. Pay close attention to tachycardia that does not improve after initial assessment and pain medications. Early aggressive fluid resuscitation may help prevent decompensated shock (3).
Disability
A rapid assessment of the neurologic status can be obtained through use of the AVPU scale, used to describe decreasing levels of consciousness. AVPU stands for:
- Alert
- responsive to Voice
- responsive to Pain
- Unresponsive
Rapidly obtaining a blood glucose level is also an important part of initial assessment.
Exposure
As always it is important to completely undress and logroll your trauma patient, but remember that children have a larger ratio of surface area to body mass. Smaller patients are more susceptible to hypothermia, so keep them warm after exposure and examination.
Pediatric trauma scores
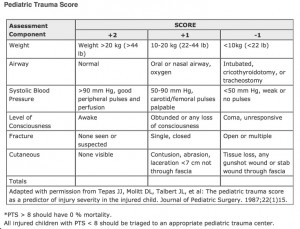
Trauma classification is important to help with triage decision making and rapid assessment of severity. Tools available include the Glasgow Coma Scale (GCS), Trauma Score (TS), and the Pediatric Trauma Score (PTS).
The pediatric trauma score includes six components and is designed to assist with rapid triage of the injured child. It has good correlation with injury severity and mortality risk, but should be used with caution in patients with isolated blunt abdominal trauma (4) as the PTS does not correlate well with trauma severity in this group.
Image adapted from: https://www.ebmedicine.net/topics.php?paction=showTopicSeg&topic_id=132&seg_id=2659
Head
Head injury is the most common cause of death in pediatric trauma, and falls are the most common mechanism of head injury in children (2).
- In an infant, a scalp laceration can cause bleeding significant enough to cause hemodynamic compromise (2).
- The majority of simple skull fractures in pediatric patients do not require intervention, but it is important to remember that they are associated with up to 20-fold increase in risk of intracranial injury.
- Children under the age of 18 months may still have an open fontanelle, so check to see if it is bulging or flat. Infants and young children are at higher risk of intracranial injuries, and parietal and occipital fractures are most commonly associated with injury (5).
- Clinical signs of intracranial injury may be more subtle in infants, and a modified GCS scale for infants should be used (2).
- Skull fractures and intracranial injuries, especially in infants, should raise concern for possible non-accidental trauma as discussed below.
In the pediatric patient it is particularly important to limit unnecessary radiation exposure. Recently, significant efforts have been made to decrease utilization of unnecessary head CT scans. For minor head trauma the PECARN head trauma study can assist with risk stratification and decision making for imaging. Secondary analyses from the initial study data published in 2014 have reported on the low risk of clinically important traumatic brain injury (ci-TBI) in patients presenting with only vomiting or loss of consciousness alone (6,7). With no other significant findings, observation rather than immediate head CT should be considered for these patients.
Image adapted from: Kuppermann et al, 2009
Neck
It is important to consider the anatomic differences between the pediatric and adult cervical spine when addressing potential injury. Upper cervical segments in children under 8 years old are hypermobile during flexion and more prone to flexion injuries (8). Although injury is uncommon, children under age 8 are more susceptible to higher cervical injury (above C3). Children have a high fulcrum at level C2-3, more prevertebral soft tissue, less developed musculature, larger heads, and anterior wedging and horizontal facets (9). As a result the increased mobility and positioning of the vertebra allow for the segments to twist, glide, and separate more easily without obvious damage (8).
The above anatomic differences lead us to a discussion of SCIWORA (spinal cord injury without radiographic abnormality), which remains a controversial and often confusing diagnosis. It has classically been defined in patients with concerns for C spine injury but no evidence of injury on x-ray or CT scan (9). In the era of widespread MRI availability, some experts believe that injuries found on MRI should not be classified as SCIWORA (9,10).
When to obtain imaging of cervical spine? At a minimum, children with a suspected injury or high risk mechanism should receive 3 view radiographs including cross table lateral, AP and odontoid views. This can be difficult to impossible to obtain in a young child. CT and/or MRI may be needed based on clinical exam or history. In the original National Emergency X-Radiography Utilization Study (NEXUS), only 2.5% of patients were under age 8, making it difficult to apply to the pediatric population (11). A follow-up study using NEXUS criteria provided evidence that NEXUS criteria can safely be applied to children over 8 years old (12). Under age 8, there still remains a lack of strong evidence based guidelines. Providers often utilize a combination of applicable NEXUS criteria, suspicion based on history, clinical clearance, and radiograph results in clinical practice.
Chest
A major pitfall is assuming that there are no intrathoracic injuries in a child without external signs of trauma.
- Pediatric patients have a more compliant chest wall with a greater amount of cartilage and bone elasticity.
- They are less likely to experience rib fractures even with significant trauma than adult trauma patients.
- Pulmonary contusion is the most common pediatric chest injury (2).
- It is important to remember that intrathoracic injury may be present without any external evidence of trauma or bony abnormality.
- The mediastinum is more easily displaced in children. Venous return and cardiac output can become compromised more easily than in adults with thoracic trauma (2).
- Intrapleural injuries are the second most common injuries in pediatric thoracic trauma (2).
- Have an early and high index of suspicion for tension pneumothorax.
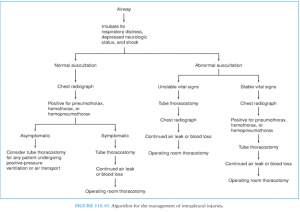
Image adapted from: Fleisher & Ludwig 2010
Blunt cardiac injury (BCI) is uncommon in children, but can be missed in those children with lack of external signs of trauma. BCI should be suspected in the presence of ecchymoses, focal tenderness, muffled heart sounds, new murmur, or abnormal extremity pulses. The management of BCI is still controversial and cardiac enzymes have questionable diagnostic value (2).
Abdomen/pelvis
The ribcage offers less protection of the intra-abdominal organs in infants and toddlers. Children also have weaker abdominal muscles and decreased abdominal fat, offering less overall organ protection. The most commonly injured intra-abdominal organ in pediatric trauma is the spleen. The liver is the second most commonly injured (2). Handlebar injuries should raise suspicion for pancreatic injury or pancreatitis in children (5).
A large prospective study showed that in children presenting to the ED after an MVC, a positive seat belt sign was significantly more predictive of an intra-abdominal injury, predominately gastrointestinal in nature (13). The literature also supports that between 0-2% of patients with a seatbelt sign but without abdominal pain or tenderness have intra-abdominal injury requiring intervention (13,14).
The PECARN network published a prediction rule that identifies patients at low risk for intra-abdominal injury (IAI). The prediction rule comprises the following components in decreasing order of importance: no evidence of abdominal wall trauma or seat belt sign, Glasgow Coma Scale score greater than 13, no abdominal tenderness, no evidence of thoracic wall trauma, no complaints of abdominal pain, no decreased breath sounds, and no vomiting. If all components are negative, the rule has a negative predictive value of 99.9% for IAI. This rule can be used to help identify low risk patients who do not need a CT scan. Currently, the prediction rule still requires external validation (15). A secondary analysis, published in December 2014, reported that the sensitivity of abdominal pain and tenderness for IAI decreased with decreasing GCS and has a sensitivity of 79% for pain (95% CI, 76%-83%) in patients with a GCS of 15 (16).
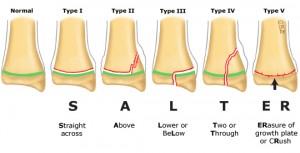
Musculoskeletal
The main difference between pediatric and adult musculoskeletal trauma lies in the fact that the pediatric skeleton is immature. Children are more prone to fractures at the physes of their bones. In particular, the Salter-Harris classification for epiphyseal fractures is an important scale to help judge fracture severity. In general, a higher grade is indicative of more injury to the growth plate itself. This is joint dependent and in general, the Salter-Harris classification system is widely used and is the most useful way for professionals to communicate information on pediatric physeal fractures.
Salter-Harris classification of physeal fractures
Image adapted from: www.uptodate.com “General principles of fracture management: fracture patterns and descriptions in children”
The growth plate is shown in green. The mnemonic refers to the fracture line and its relationship to the growth plate. The metaphysis is the bone above the growth plate, and the epiphysis is the bone below. Type I fractures disrupt the physis. Type II fractures involve a break from the growth plate up into the metaphysis, with the periosteum usually remaining intact. Type III fractures are intraarticular fractures through the epiphysis that extend across the physis. Type IV fractures cross the epiphysis, physis, and metaphysis. Type V fractures are compression injuries to the physis.
Non-accidental trauma (NAT)
NAT is an extremely important and an often underestimated pediatric diagnosis. It accounts for approximately 10% of pediatric patients hospitalized due to trauma. Delayed recognition occurs frequently, and contributes to increased mortality. In a pediatric trauma study, there was an almost six-fold increase in mortality with NAT patients compared to accidental trauma patients. Delayed recognition was estimated in approximately 20% of the NAT cases (17). Abusive head trauma in a young infant may present subtly with nonspecific findings including vomiting, poor feeding, delayed development, or irritability. Head trauma is the most common cause of death due to NAT and subdural hemorrhage and retinal hemorrhages are the most common findings (18). Red flags for possible NAT include patterned bruises or lesions, bruising in a young or non-ambulating child, bruising on areas other than the extremities, symmetric burns (immersion pattern), or any injury that does not match the history or developmental level of the child. By keeping NAT on your differential you may help save the life of a child!
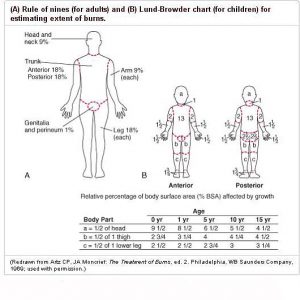
Burns
After addressing your ABCs and evaluating for inhalation injuries, all burn patients should have a rapid assessment of severity including depth, type of burn, location and size. Burn wound assessment in pediatrics is different than in adults. (2). Over the age 10 years, you may use the adult “rule of 9s.” The patient should be undressed with sterile covers placed over wounds. IV fluid resuscitation should be initiated in patients with burns over 20% BSA. The Parkland formula may be used to guide fluid resuscitation while monitoring urine output and heart rate in children. Always remember to appropriately address pain in your infant and pediatric burn patients.
Ultrasound
Ultrasound is a promising and valuable imaging modality to help reduce radiation exposure in the pediatric trauma evaluation. One meta-analysis showed a sensitivity of 66% and a specificity of 95% of the focused assessment of sonography for trauma (FAST) for identifying hemoperitoneum in pediatric patients (19). Emergency department and bedside ultrasonography has also been shown to be useful in the evaluation of pediatric long bone and skull fractures, and vertebrae abnormalities in neonates (20, 21, 22). Ultrasound should also be considered for use in peripheral nerve blocks and vascular access.
Current research
There are still many areas of pediatric trauma where additional research is required. In both the USA and worldwide, efforts are being made to improve understanding of pediatric trauma, improve management, and continue to find safe ways to limit radiation exposure. In addition to the larger PECARN studies mentioned above, there are many interesting smaller studies recently published. An Egyptian study recently reported in 2014 found that a D-dimer level might be an important adjunct in the evaluation of children with head trauma, with low levels suggesting absence of TBI and improved outcomes (23).
Although tranexamic acid has been shown to decrease mortality and use of blood products in severely injured adults (24), it was previously not studied in pediatric trauma. A recently published study, the pediatric trauma and tranexamic acid study (PED-TRAX), reviewed retrospective data from Afghanistan to demonstrate that tranexamic acid given to pediatric trauma patients overseas in combat setting showed decreased mortality (25).
As always in pediatrics it is important to include family members in the decision making process, and provide support services for parents dealing with children involved in trauma. Know who your support staff members are and how to reach them in advance.
References:
- Tracy ET,Englum BR,Barbas AS, Foley C, Rice HE, Shapiro ML. Pediatric injury patterns by year of age. J Pediatr Surg. 2013 Jun;48(6):1384-8.
- Fleisher GR, Ludwig S. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2010.
- Kenefake ME, Swarm M, Walthall J. Nuancesinpediatric trauma. Emerg Med Clin North Am. 2013 Aug;31(3):627-52.
- Saladino R, Lund D, Fleisher G. The spectrum of liver and spleen injuries in children: failure of the pediatric trauma score and clinical signs to predict isolated injuries. Ann Emerg Med. 1991;20(6):636.
- Cline DM , Ma OJ, Cydulka RK, Meckler GD, Handel DA, Thomas SH. Tintinalli’s Emergency Medicine Manual, 7th ed. New York: McGraw-Hill Professional; 2012.
- Lee LK, Monroe D, Bachman MC, Glass TF, Mahajan PV, Cooper A, Stanley RM, Miskin M, Dayan PS, Holmes JF, Kuppermann N, Traumatic Brain Injury (TBI) Working Group of Pediatric Emergency Care Applied Research Network (PECARN). Isolated loss of consciousness in children with minor blunt head trauma. JAMA Pediatr. 2014 Sep;168(9):837-43.
- Dayan PS, Holmes JF, Atabaki S, Hoyle J Jr, Tunik MG, Lichenstein R, Alpern E, Miskin M, Kuppermann N, Traumatic Brain Injury Study Group of the Pediatric Emergency Care Applied Research Network (PECARN). Association of traumatic brain injuries with vomiting in children with blunt head trauma. Ann Emerg Med. 2014;63(6):657.
- Pang D. Spinal cord injury without radiographic abnormality in children, 2 decades later. Neurosurgery.2004 Dec;55(6):1325-42;discussion 1342-3.
- Mahajan P,Jaffe DM,Olsen CS, Leonard JR, Nigrovic LE, Rogers AJ, Kuppermann N, Leonard JC. Spinal cord injury without radiologic abnormality in children imaged with magnetic resonance imaging. J Trauma Acute Care Surg. 2013 Nov;75(5):843-
- Yucesoy K, Yuksel KZ. SCIWORA in MRI era. Clin Neurol Neurosurg. 2008 May;110(5):429-33
- Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94.
- Viccellio P, Simon H, Pressman BD, et al. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108:E20.
- .Borgialli DA, Ellison AM, Ehrlich P, Bonsu B, Menaker J, Wisner DH, Atabaki S, Olsen CS, Sokolove PE, Lillis K, Kuppermann N, Holmes JF; for the Pediatric Emergency Care Applied Research Network (PECARN). Association Between the Seat Belt Sign and Intra-abdominal Injuries in Children With Blunt Torso Trauma in Motor Vehicle Collisions. Acad Emerg Med. 2014 Nov;21(11):1240-1248
- Sokolove PE, Kuppermann N, Holmes JF. Association between the “seat belt sign” and intra-abdominal injury in children with blunt torso trauma. Acad Emerg Med. 2005;12(9):808.
- Holmes, et al. Pediatric Emergency Care Applied Research Network (PECARN). Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med. 2013;62(2):107.
- Adelgais KM, Kuppermann N, Kooistra J. et al. Intra-Abdominal Injury Study Group of the Pediatric Emergency Care Applied Research Network (PECARN) Accuracy of the Abdominal Examination for Identifying Children with Blunt Intra-Abdominal Injuries . J Pediatr. 2014 Dec;165(6):1230-1235.e5
- Estroff JM, Foglia RP, Fuchs JR. A Comparison of Accidental and Nonaccidental Trauma: It Is Worse Than You Think. J Emerg Med. Epub ahead of print. 2014 Sep 29.
- Narang S, Clark J. Abusive head trauma: past, present and future. J Child Neurol.2014 Dec;29 (12):1747-56. Epub 2014 Oct 14.
- Holmes JF, Gladman A, Chang CH. Performance of abdominal ultrasonography in pediatric blunt trauma patients: a meta-analysis. J Pediatr Surg. 2007;42(9):1588.
- Sinha TP et al. Diagnostic accuracy of bedside emergencyultrasoundscreening for fractures in pediatric trauma patients. J Emerg Trauma Shock. 2011 Oct;4(4):443-5.
- Rabiner JE1,Friedman LM,Khine H, Avner JR, Tsung JW. Accuracy of point-of-care ultrasound for diagnosis of skull fractures in children. Pediatrics. 2013 Jun;131(6):e1757-64
- Vanderhave KL,Brighton B,Casey V, Montijo H, Scannell B. Applications of Musculoskeletal Ultrasonography in Pediatric Patients. J Am Acad Orthop Surg. 2014 Nov;22(11):691-698.
- Foaud HM, Labib JR, Metwally HG, El-Twab KM. Plasma D-dimer as a Prognostic Marker in ICU Admitted Egyptian Children with Traumatic Brain Injury. J Clin Diagn Res. 2014 Sep;8(9) Epub 2014 Sep 20.
- Shakur H, Roberts I, Bautista R, et al; CRASH-2 Trial Collaborators. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376:23-32.
- Eckert MJ,Wertin TM,Tyner SD, Nelson DW, Izenberg S, Martin MJ. Tranexamic acid administration to pediatric trauma patients in a combat setting: The pediatric trauma and tranexamic acid study (PED-TRAX). J Trauma Acute Care Surg. 2014 Dec;77(6):852-8.
Further Reading:
National Trauma Data Bank. Chicago, IL: American College of Surgeons. Available: http://www.facs.org/trauma/ntdb.html.
http://www.ncbi.nlm.nih.gov/pubmed/25441044
http://www.ncbi.nlm.nih.gov/pubmed/25186511










8 thoughts on “Pediatric Trauma: Pearls and Pitfalls”
Pingback: LITFL Review 169 - LITFL
Pingback: Is Coronary CT Worth It? The FOAMed Report - news from Allwebsolutions.net
Pingback: Paediatric trauma: pearls and pitfalls | FOAM links
Pingback: Episode 95 Pediatric Trauma | EM Cases
Pingback: emDOCs.net – Emergency Medicine EducationThe EM Educator Series: Trauma Chameleons and Missed Injuries - emDOCs.net - Emergency Medicine Education
Pingback: LITFL Review 169 • LITFL Medical Blog • FOAMed Review
Pingback: eFAST – Översikt – Mind palace of an ER doc
Pingback: Conference Recap 10/4/2023 – BMC EM Blog