EM@3AM: Periorbital Cellulitis
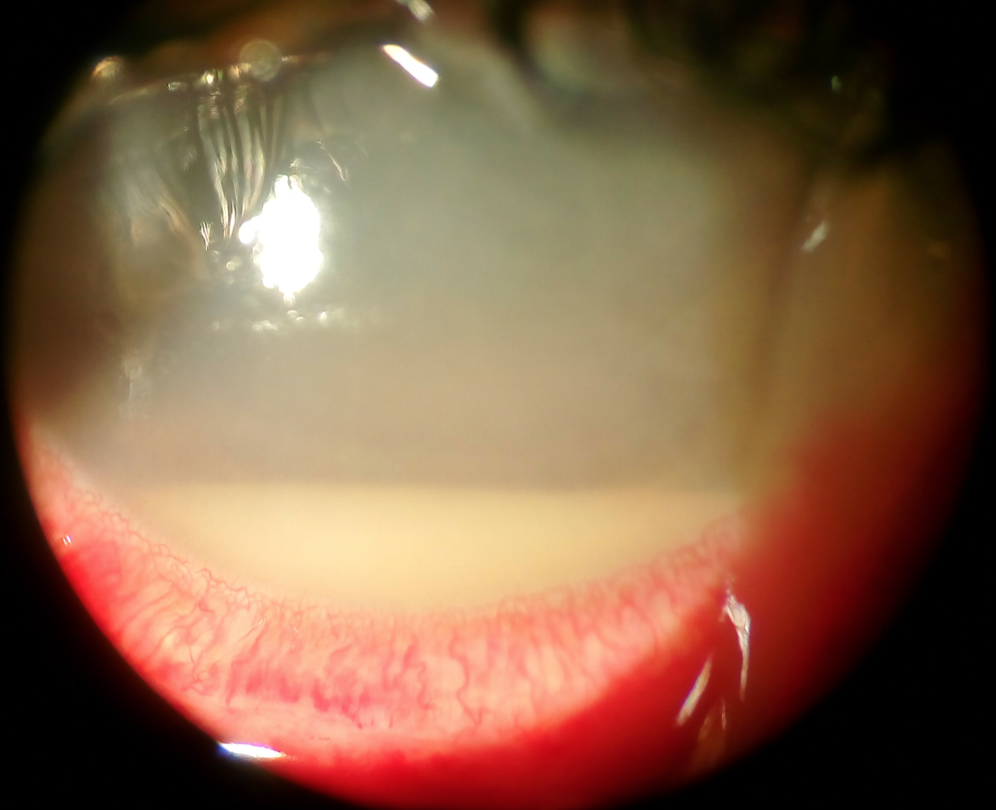
An 8-year-old boy presents with left eyelid swelling for 2 days. Parents report the swelling has progressively worsened and is greater in the upper eyelid. It is associated with erythema, warmth, and tenderness. They also note subjective fevers. For the past week, the patient had watery rhinorrhea, dry cough, and nasal congestion. Parents deny recent trauma or known insect bite. The patient’s vitals include T 100.2F, BP 113/67, HR 123, RR 26, SpO2 of 99% on room air. On physical exam, the patient is non-toxic appearing. His eye exam is significant for edema and erythema to the left periorbital region greater in the upper eyelid. There is mild warmth but no crusting or active drainage. His extraocular movements are intact and painless, and there is no conjunctivitis or chemosis. What is the diagnosis?
EM@3AM: Periorbital Cellulitis Read More »