Originally published at EM Cases. Reposted with permission. Listen to accompany podcast HERE
Follow Dr. Anton Helman on twitter at @EMCases
There is a long list of rare neuromuscular diseases. Nonetheless, there are a few that you are likely to see in the ED, that are relevant to Emergency Medicine because they require timely diagnosis and treatment. In this Part 2 of our 2-part series on acute motor weakness with Roy Baskind and George Porfiris, we keep it short and simple by limiting our discussion to the key clinical clues and management strategies of two of the more common acute life-threatening neuromuscular diseases, myasthenia gravis and Guillain Barré syndrome, and how to distinguish them from their mimics…
Podcast production, sound design & editing by Anton Helman; voice editing by Raymond Cho.
Written Summary and blog post by Saswata Deb & Priyank Bhatnagar, edited by Anton Helman June, 2021
Cite this podcast as: Helman, A. Baskin, R. Porfiris, G. Neuromuscular Disease for Emergency Medicine. Emergency Medicine Cases. June, 2021. https://emergencymedicinecases.com/neuromuscular-disease. Accessed Tue, 22 Apr 2025 03:20:31 +0000
Guillain-Barré syndrome and myasthenia gravis are two neuromuscular disorders that can present with rapid respiratory compromise and subsequent mortality. Fortunately, they both present with hallmarks of clinical diagnosis that the emergency physician can use for early recognition.
Guillain-Barre syndrome (GBS): The areflexic ascending symmetric neuromuscular disease
Guillain-Barre syndrome is an autoimmune disorder of the myelin sheath characterized by an acute/subacute onset of progressive peripheral polyneuropathy, symmetrical distribution, ascending pattern of loss of power and areflexia. GBS has a 5% mortality risk, with one-third of patients requiring endotracheal intubation and ICU admission. Even non-ventilated patient can have prolonged admissions of up to 5 weeks. Recovery is also slow, with 50-95% of patients taking a year to return to baseline functional status.
Areflexia and ascending symmetrical weakness are the hallmarks of GBS
The loss of deep tendon reflexes in the patient with acute loss of symmetric ascending motor power should be considered GBS until proven otherwise. It is incumbent upon the EM provider to assess for deep tendon reflexes carefully, employing passive control of the patient’s limb and distraction techniques (such as asking the patient to count backwards from 100 in serial 7s) while eliciting reflexes. With a delay in diagnosis autonomic dysfunction ensues, resulting in swings of tachy/bradycardia and hypo/hypertension as well as diaphragmatic and respiratory muscle weakness and respiratory failure.
Despite complaints of numbness and tingling, sensation testing is usually intact in GBS. The presence of a sharp sensory level points to alternative diagnoses such as transverse myelitis.
Preceding viral infections are common in GBS but not necessary for the diagnosis. Up to two-thirds of patient with GBS report preceding viral symptoms. One of the more common viral infections seen in this context is Campylobacter jejuni gastroenteritis.
Early diagnosis and initiation of treatment of GBS is essential to prevent autonomic dysfunction and respiratory compromise
Early treatment of GBS is thought to prevent the progression to autonomic dysfunction and respiratory arrest as well as the need for ICU care/endotracheal intubation. The most effective treatment of GBS is plasma exchange, however it is not readily available at many centers. Hence, IVIG therapy is usually the first line treatment, and if it fails, then plasma exchange is usually initiated.
The two important alternate diagnoses to consider in GBS are tick paralysis and transverse myelitis
Tick Paralysis can be distinguished from GBS by prodromal ataxia, restlessness and irritability, a history of tick bite in an endemic area during spring or summer, and a more rapid progression of disease.
Like GBS, tick paralysis causes an ascending loss of motor power that may lead to respiratory compromise and arrest. It is caused by the salivary neurotoxin of several species of tick. The characteristic prodrome of tick bite paralysis is ataxia associated with restlessness and irritability that begins 4 to 7 days after the tick attaches to the patient’s skin. After these initial symptoms, an ascending, symmetrical flaccid paralysis occurs. This may progress to bulbar involvement and respiratory paralysis. Tick paralysis is more common in children than in adults. Treatment is early removal of the tick and supportive care. It is imperative to consider tick paralysis in the child who presents with ataxia.
Clinical Pearl: In pediatric patients with ataxia and/or acute loss of power and ascending weakness, it is important to thoroughly examine for ticks, including the entire scalp, as this is an often-missed location on assessment. Remove the offending tick using fine forceps applied close to the skin with gentle, steady, upward traction, taking care to avoid leaving tick parts embedded in the wound.
The reason that it is so important to make this diagnosis early and locate the offending tick on the patient, is that simply removing the tick is curative and prevents the progression to respiratory compromise and death.
Distinguishing transverse myelitis from GBS
Transverse myelitis is a rare inflammatory condition of the spinal cord. Like GBS, transverse myelitis is an acquired neuro-immune disorder, often postinfectious, that presents with the acute onset of bilateral lower extremity motor weakness, and may progress to include autonomic dysfunction. However, as opposed to GBS, paresthesias with a distinct sensory level deficit usually accompany the motor weakness, back pain is a typical feature, paresthesias may be asymmetric, reflexes are usually present, and most importantly, as it is a spinal cord condition, transverse myelitis typically presents with accompanying bowel or bladder dysfunction. The usual clinical scenario in the ED that transverse myelitis is considered in is in patients suspected of cauda equina syndrome, and the diagnosis is usually made after MRI, which typically shows 3-5 spinal cord segments of T2 increased signal occupying greater than two-thirds of the cross-sectional area of the cord with a variable pattern of enhancement.
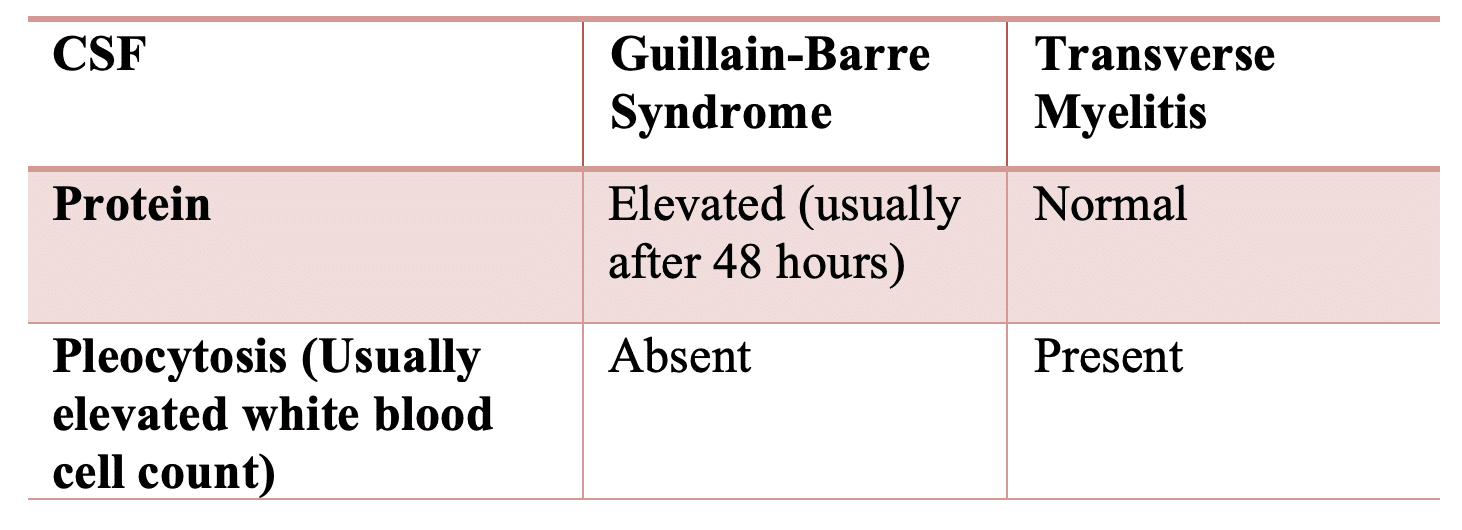
Lumbar puncture may help differentiate GBS from transverse myelitis. Typically, elevated cerebrospinal fluid proteins are seen in GBS, but if done early in the disease course protein levels may be normal requiring a repeat LP later in the hospital stay if GBS remains on the differential. Pleocytosis is typical of transverse myelitis whereas it is absent in GBS.
Recognition and management of respiratory failure associated with neuromuscular disease
Tachypnea and neck flexion weakness are signs of impending respiratory compromise in the patient with neuromuscular disease
Patients with neuromuscular disease are at particularly high risk of respiratory failure, given the propensity for altered mental status and diaphragmatic and/or accessory respiratory muscle weakness. Tachypnea often presents sooner than, and may herald other signs of, impending respiratory failure.
It is prudent for the ED physician to look for the following when assessing the airway status of patient with motor power loss:
- Abnormal or poor mentation
- Difficulty with speech or weak voice
- Drooling or other indication of difficulty handling secretions
- Inability or difficulty lifting their head off the stretcher
- Weak, rapid, or shallow breaths or use of accessory muscles
Pitfall: A common pitfall is to assume that the cause of tachypnea in a patient with suspected neuromuscular disorder with a normal oxygen saturation is due to acidemia only. Tachypnea is often a sign of impending respiratory compromise in these patients due to neuromuscular compromise that may require a definitive airway.
When to intubate the patient with suspected neuromuscular disease: Neck flexor weakness and the “20/30/40 rule”
In addition to tachypnea, impending respiratory compromise can be heralded by decreased neck flexion strength, as it has shared innervation with the diaphragm. This can be tested by resisting neck flexion with your hand against the patient’s forehead and asking them to lift their head off the bed. Normally, the neck flexors are able to overcome the examiner’s hand.
The “20/30/40 rule” to aid in the decision to secure a definitive airway in patients with neuromuscular disease
Objective measures that help guide the decision for intubation include:
- Vital capacity (VC) < 20cc/kg,
- Maximal inspiratory pressure (MIP) < 30 cmH2O, and
- Maximal expiratory pressure (MEP) < 40 cmH2O.
The decision to secure the airway should not be made solely on the 20/30/40 rule.
BiPAP or High Flow Nasal Cannulae (HFNC) can be considered as a bridge to a definitive airway or to prevent the need for intubation in those patients with mild symptoms and who pass the 20/30/40 rule.
Myasthenia gravis: the fatigable, fluctuating, descending neuromuscular disease
Myasthenia gravis is an autoimmune disorder that typically presents as fluctuating descending motor weakness, without loss of sensation or reflexes. Anti-acetylcholine antibodies block postsynaptic acetylcholine receptors at the neuromuscular junction. Typically, bulbar symptoms appear early in the progression of the disease with ptosis and diplopia being the most common presenting symptoms. As the disease progresses caudally, generalized loss of motor power and respiratory muscles involvement ensues, leading to respiratory arrest if left untreated. Similar to Guillain-Barre syndrome, a delay in diagnosis may result in autonomic dysfunction, resulting in swings of tachy/bradycardia and hypo/hypertension. There is a bimodal peak age of presentation of myasthenia gravis; females in their 20-30s and male in their 70-80s. This older age group is often underappreciated.
The two Fs of myasthenia gravis: fatigability and fluctuation
The two Fs that characterize myasthenia gravis are fatigability of various muscle groups with repeated use including extraocular muscles, muscles of mastication, phonation and proximal limb muscles and fluctuation of symptoms. This sometimes makes clinical assessment difficult as patients may present on a day when their symptoms have resolved, or in the morning when fatigability has not taken effect, and their neurologic exam is grossly normal. With this course of illness, repeated visits to the ED are often required to make the diagnosis, and careful provocative testing is essential to make the provisional diagnosis.
Fatigue: The most common symptom of myasthenia is fatigue of various muscle groups after prolonged exertion, worsening as the day progresses, and improving with rest. Commonly affected muscle groups include ocular (diplopia or ptosis after prolonged screen time), mastication muscles (difficulty in chewing by the end of eating dinner) and phonation (weakening voice with prolonged conversation). Muscle weakness may progress down to the hip flexors.
Bulbar muscle weakness may manifest as nasal speech, coughing, dysphagia, or dysarthria and calls for careful cranial nerve testing.
Physical Exam: provocative testing is key to the provisional diagnosis of myasthenia – prolonged upgaze and the ice pack test
There are two physical exam maneuvers specific to myasthenia gravis that can aid in the provisional ED diagnosis:
Prolonged upgaze: Ask the patient to g at the ceiling for 30 seconds. A positive sign includes ptosis (or worsening of ptosis) and the development of diplopia.
Ice pack test: Place an ice pack on patient’s orbit. The cold temperature inhibits the enzyme that breaks down acetylcholine, and therefore should result in resolution of ptosis and diplopia. The sensitivity is 90%; specificity is 80% for the diagnosis of myasthenia gravis.
Diagnosis is confirmed with the tensilon test which involves giving the fast-acting acetylcholinesterase inhibitor IV edrophonium and observing for improved ptosis and ophthalmoparesis. This test is specific but not sensitive for the diagnosis of myasthenia gravis. EMG testing may support the diagnosis as well.
Clinical pearl: Sensation, reflexes and pupillary reflexes are all spared in patients with myasthenia gravis
Key differential of myasthenia gravis: Lambert-Eaton syndrome and botulism
Lambert-Eaton Syndrome (LES)
While MG involves pathology with postsynaptic acetylcholine receptors, LES involves antibodies that target the presynaptic calcium channels which results in decreased calcium influx and consequently acetylcholine release.
Patients with LES are typically older and may have an underlying malignancy – usually small cell lung cancer. While motor weakness is typically fluctuating like in myasthenia gravis, the key distinguishing feature is the muscle groups involves tend to be proximal limb muscles which tend to improve with repeated use. This paradoxical improvement is likely due to more action potentials with repeated use that results in increase calcium influx in the neuronal cells.
A classic exam finding in LES is the Lambert’s sign, where handgrip in an affected individual strengthens with repeated evaluation.
Clinical pearl: The key distinguishing feature between myasthenia gravis and Lambert-Eaton syndrome is that muscle power fatigues with repeated use in the former and improves with repeated use in the latter.
Botulism
The Botulism toxin interferes with acetylcholine vesicle fusion at the presynaptic nerve terminal. Patients may present with muscle weakness, diplopia or blurry vision similar to myasthenia gravis. A distinguishing feature from MG is that in about 50% of patients with botulism, the pupillary reflexes are impaired.
In myasthenia gravis, it is recommended to use a lower dose of rocuronium since the pathophysiology of the illness includes destruction of the acetylcholine receptors at the neuromuscular junction.
Treatment of myasthenia gravis includes physostigmine (acetylcholinesterase inhibitor), immunosuppressants (azathioprine, cyclosporine, steroids, tacrolimus), IVIG and plasmapheresis.
Learn more about myasthenia gravis at EM Quick Hits 6 (skip to 26:37).
Take home points for neuromuscular disease for emergency medicine
- Guillain-Barre syndrome is an acute, ascending, symmetric and progressive peripheral neuropathy
- The hallmarks of Guillain-Barre syndrome are areflexia and an ascending symmetric pattern of weakness
- Many patients with Guillain-Barre syndrome report a preceding viral-like illnesses, but this is not necessary for the diagnosis
- Tick paralysis differs from Guillain-Barre syndrome in that there is a prodrome of ataxia and irritability prior to the loss of power, and that it occurs in the spring and summer months in tick-endemic areas
- Transverse myelitis differs from Guillain Barre syndrome in that urinary dysfunction is typical of the former
- Myasthenia gravis is a postsynaptic autoimmune disorder of young woman and older men characterized by a descending loss in motor power, typically presenting with bulbar symptoms that are fatigable and fluctuate, hence patients may present when symptoms and signs are absent
- The provisional diagnosis of myasthenia gravis can be in the ED with the simple ice pack test and upgaze test
- Lambert-Eaton syndrome is a presynaptic autoimmune disorder that is commonly seen in older patients and may be distinguished from myasthenia gravis by paradoxical improvement in symptoms with repeated muscle use
Learn more about acute motor weakness presentations to the ED in Ep 156
References for Neuromuscular Disease for Emergency Medicine
- Khamees D, Meurer W. Approach to acute weakness. Emerg Med Clin North Am. 2021;39(1):173-180.
- Asimos A, Birnbaumer D, Karas S, Shah S. Weakness: a systematic approach to acute, non-traumatic, neurologic and neuromuscular causes. Emergency Medicine Practice + Em Practice Guidelines Update. 2002;4(12):1-26.
- Ganti L, Rastogi V. Acute generalized weakness. Emerg Med Clin North Am. 2016;34(4):795-809.
- Asimos AW. Evaluation of the adult with acute weakness in the emergency department. UpToDate, Hockberger, RS (Ed), UpToDate, Grayzel, J. 2013.
- Grattan-Smith PJ, Morris JG, Johnston HM, et al. Clinical and neurophysiological features of tick paralysis. Brain. 1997;120 ( Pt 11):1975-1987.
- Edlow JA, McGillicuddy DC. Tick paralysis. Infect Dis Clin North Am. 2008;22(3):397-413, vii.
- Juel VC, Bleck TP. Neuromuscular disorders in critical care. In: Textbook of Critical Care, Grenvik A, Ayres SM, Holbrook PR, Shoemaker WC (Eds), WB Saunders, Philadelphia 2000. p.1886.
- Rabinstein AA, Wijdicks EFM. Warning signs of imminent respiratory failure in neurological patients. Semin Neurol. 2003;23(1):97-104.
- McGillicuddy DC, Walker O, Shapiro NI, Edlow JA. Guillain-Barré syndrome in the emergency department. Ann Emerg Med. 2006;47(4):390-393.
- Hughes RAC, Cornblath DR. Guillain-Barre Syndrome. Lancet 2005; 366: 1653-66.
- Raphaël JC, Chevret S, Hughes RA, Annane D. Plasma exchange for Guillain-Barré syndrome. Cochrane Database Syst Rev. 2002;(2):CD001798.
- Hughes RAC, Swan AV, van Doorn PA. Intravenous immunoglobulin for Guillain-Barré syndrome. Cochrane Database Syst Rev. 2014;(9):CD002063.
- Roper, J., Fleming, M. E., Long, B., & Koyfman, A. (2017). Myasthenia gravis and crisis: Evaluation and management in the emergency department. The Journal of Emergency Medicine, 53(6), 843-853.
- Jayarangaiah A, Theetha Kariyanna P. Lambert Eaton Myasthenic Syndrome. [Updated 2020 Jul 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- Guidon, A. C. (2019). Lambert-Eaton myasthenic syndrome, botulism, and immune checkpoint inhibitor–related myasthenia gravis. CONTINUUM: Lifelong Learning in Neurology, 25(6), 1785-1806.
Other FOAMed Resources on Neuromuscular Disease
First10EM on myasthenia gravis
First10EM on myasthenia crisis
EMCrit project on myasthenia gravis
Drs. Helman, Baskind and Porfiris have no conflicts of interest to declare








