Ready for the New Sepsis 3.0?
- Mar 17th, 2016
- Brit Long
- categories:
Author: Brit Long, MD (@long_brit, EM Chief Resident at SAUSHEC, USAF) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Sepsis is an all too common condition managed in EDs and ICUs around the world. A wide range of estimates for prevalence exists, with 300 to 1000 cases per 100,000 persons per year. Unfortunately, there is no validated gold standard criterion or standard diagnostic test for this syndrome, which results from the host response to infection, often with organ dysfunction. The syndrome consists of a constellation of clinical signs and symptoms with suspected infection.
The Old Definition
To meet SIRS criteria, two of the following must be present: HR > 90 bpm, RR > 20 or PaCO2 < 32, temperature < 36oC or > 38oC, and a WBC count < 4 x 109 cells/L or > 12 x 109 cells/L or > 10% bands. Two or more of these equals SIRS, and two or more with a source of infection equals sepsis.1,2 Unfortunately these criteria are non-specific, and the criteria alone do not provide a diagnosis or predict outcome. The definitions are shown below in Figure 1, along with severe sepsis and septic shock:
Figure 1 – SEPSIS Criteria, from Canetnacci MH, King K. Severe Sepsis and Septic Shock: Improving Outcome in the Emergency Department. Emerg Med Clin N Am 2008;26:603–623.
Many have questioned the use of SIRS and the old definition of sepsis. Patients with sepsis and this old definition include a heterogeneous group, and it may go unrecognized. According to the SIRS naysayers, one of the major issues with SIRS is that it misses 1 out of 8 patients with diagnosed severe sepsis (notice this is not sepsis, but severe sepsis), reported in a recent study from the NEJM.3 However, another way of thinking about this is it catches 7 out of 8 patients with severe sepsis, for a sensitivity of 88%. There are multiple positives and negatives of this study, which was conducted in ICU patients, where SIRS was retrospectively applied. Mortality was 24.5% in SIRS positive patients, compared to 16.1% in SIRS negative patients. The SIRS negative patients also had shorter ICU and hospital stays, as well as higher rates of discharge to their own home. All patients were diagnosed and treated, and most importantly, it demonstrates a decrease in mortality of both SIRS negative and positive patients. Please see this blog post by Justin Morgenstern, creator of First10EM, @ http://first10em.com/2016/03/04/sirs-vs-sofa/ for further information on SIRS and the study.
Now onto “Sepsis 3.0” with qSOFA and SOFA…
A task force consisting of the European Society of Intensive Care Medicine and the Society of Critical Care Medicine recently proposed a new definition for sepsis and septic shock. These definitions are based on the use of two scores, qSOFA and SOFA, which are validated in the ICU, not ED. Please see http://www.jamasepsis.com for the full overview of the new definitions.4-6
The resulting publication has stirred a large amount of controversy, with some advocating strongly for the new changes, and others decrying the change. The FOAM world has blown up with important aspects of the new changes.
Please see the following resources, each with thorough, complete descriptions of the new proposed definitions, as well as the potential issues with using these definitions: http://rebelem.com/sepsis-3-0/, http://icmwk.com/2016/02/25/sepsis-3/, http://foamcast.org/2016/02/21/sepsis-redefined/, http://stemlynsblog.org/sepsis-16/, and http://emcrit.org/pulmcrit/problems-sepsis-3-definition/.
This post will provide an overview of Sepsis 3.0. We will not delve into the controversies surrounding the updated definitions. For further reading, see the above excellent blog posts.
1. Sepsis is defined as life-threatening organ dysfunction due to dysregulated host response in the setting of infection.
2. Organ dysfunction can be identified based on total SOFA score > 2 points. A score > 2 points is associated with a mortality of 10%.
The SOFA score is based on blood pressure, vasopressor use, platelet count, bilirubin, GCS, creatinine, PaO2/FiO2 ratio, and presence of mechanical ventilation. Here is an easy plug in tool while on shift, from MDCalc: http://www.mdcalc.com/sequential-organ-failure-assessment-sofa-score/
Figure 2 – SOFA score from http://www.jamasepsis.com
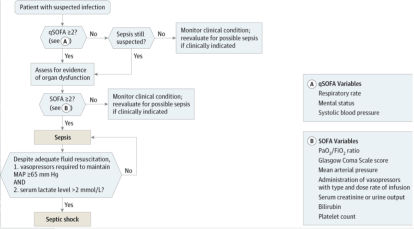
3. The qSOFA score does not require laboratory tests and can be used quickly at the bedside. This consists of hypotension (SBP < 100 mm Hg), altered mental status (or a GCS of 13 or less), and tachypnea with RR > 22/min. Greater than or equal to 2 suggests poor outcome.
4. Septic shock is defined by persisting hypotension that requires vasopressor use to keep MAP > 65 mmHg with a lactate > 2mmol/L, despite adequate volume resuscitation. Mortality for this group exceeds 40%.
A flow chart for the new definition is shown below in Figure 3.
Figure 3 – Updated Sepsis Diagram, from http://www.jamasepsis.com
For emergency providers, Justin Mandeville’s “rule of 2’s” is a helpful resource, from http://icmwk.com/2016/02/25/sepsis-3/
Caveats
– Notice that a patient with qSOFA > 2 on the chart still requires assessment for evidence of organ dysfunction, thus necessitating use of the SOFA score. However, on his excellent interview with Merv Singer, one of the lead authors of the new definition, Scott Weingart of EMCrit fame questioned this concern (http://emcrit.org/podcasts/sepsis-3/). Dr. Singer advocates for the use of clinical gestalt. Neither the qSOFA nor SOFA scores are management triggers. They instead function as markers for mortality, risk stratification, and as prompts to consider sepsis. If the clinician is worried for infection, begin treatment and resuscitation, even with negative qSOFA and SOFA scores.
– There is no longer “severe sepsis,” which was present in the older definition.
– These scores (qSOFA and SOFA) are not screening tools. They have only been validated as markers for mortality.
– Pediatric sepsis is not included in this update.
– Lactate is in the criteria for septic shock, but it is not present in the bedside criteria for sepsis identification. This test can be used as a marker for hemodynamic stress and mortality, as well as resuscitation (10% clearance), and likely should still be used.
– These definitions are not endorsed by American College of Emergency Physicians (ACEP), American College of Chest Physicians (ACCP), or the Latin American Sepsis Institute.
– These scores are validated for ICU patients, not the ED.
References/Further Reading:
- Elixhauser A, Friedman B, Stranges E. Septicemia in U.S. Hospitals, 2009. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb122.pdf.
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013;41:580–637.
- Kaukonen KM, Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic inflammatory response syndrome criteria in defining severe sepsis. The New England journal of medicine. 372(17):1629-38.
- Singer M, Deutschman CS, Seymour CW, et al: The Sepsis Definitions Task Force The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). AMA. 2016;315(8):801-810.
- Seymour CW, Liu V, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):762-774.
- Shankar-Hari M, Phillips G, Levy ML, et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). (JAMA, Feb 22, 2016).




3 thoughts on “Ready for the New Sepsis 3.0?”