emDOCs Podcast – Episode 80: Traumatic Arthrotomy
- Jun 21st, 2023
- Brit Long
- categories:
Today on the emDOCs cast with Brit Long, MD (@long_brit), we discuss traumatic arthrotomy, also known as an open joint.
Episode 80: Traumatic Arthrotomy
What is traumatic arthrotomy (TA)?
- TA occurs when a wound disrupts a joint capsule and exposes the intra-articular surface of a joint to contamination and potentially infection.
- May lead to significant morbidity

Typical presentation:
- Males in their 20s and 30s are most commonly affected
- Mechanisms include any potential injury, but GSW and MVCs are most common
- Knee is most commonly involved (53-91% of TA cases)
Complications
- Septic arthritis
- ~15% mortality risk
- Irreversible decrease in joint function in ~50% of patients
- Before the medical era with antibiotics, septic arthritis occurred in up to 100% of TAs, but now that rate is < 5%.
- Functional outcomes
- Severe soft tissue injuries and damage to the bony structures => poor functional outcomes.
- If we miss the diagnosis and there’s a delay in washout and debridement, patients can have chronic pain, a limp, decreased ROM, etc.
When to consider traumatic arthrotomy
- Classification system (Collins and Temple): Grade 1-4
- Grade 1: single capsular perforation/laceration without extensive soft-tissue injury; easily missed
- Grade 4: open dislocation or neurovascular injury requiring repair
- Consider open joint in any patient with wound near a joint, severe soft tissue injury, and fluid leaking from a wound.
History
- Identification of a mechanism that could result in a penetrating injury or an examination that identifies even a small periarticular laceration is the first step in raising the suspicion for TA
- No specific component of the history can rule in or out
- One study found clinical judgment alone had a sensitivity ~57% and specificity ~61% for TA diagnosis.
- Consider mechanism, risk for contamination, and risk of foreign body
Exam – suggestive findings
- Laceration over the joint
- Capsule disruption
- Synovial fluid (straw colored, viscous, oily)
- Presence of bubbles or fat droplets coming from the wound
How do you use labs and imaging in these patients?
- Labs do not play a significant role
- Imaging
- X-ray: Start with plain films to look for fracture near laceration, intra-articular free air, radiopaque foreign body.
- While suggestive of TA, not sensitive or specific.
- A 2013 study found a sensitivity of ~47% for TA of the knee using plain radiographs. Based on the data, a normal x-ray couldn’t rule it out.
- If thinking TA, share your concern with radiology, which improves sensitivity.
- US: under studied but not routinely recommended
- A 2019 study evaluating use of US in cadavers found a sensitivity of 65% and specificity of 75%.
- CT scan: more sensitive and specific in the knee, but not in smaller joints.
- Newer evidence supports the use of CT for TA of the knee. One study of cadavers found a sensitivity and specificity near 100% for detecting 0.1 mL of air in the knee. Another study found again a sensitivity approaching 100% for the knee, and CT changed management in over 40% of patients.
- There are many issues with the literature. CT has not been directly compared with saline load test (SLT), there’s significant bias, and many studies look at free air only or are performed with cadavers.
- Nowhere near as good for other joints. If you look at the elbow, some studies suggest a sensitivity of 0% for CT.
- X-ray: Start with plain films to look for fracture near laceration, intra-articular free air, radiopaque foreign body.
Gold Standard= Saline load test (SLT)
- Check integrity of the joint capsule by injecting sterile saline solution (STS) into the joint (away from location of the injury) and looking for fluid coming from the wound.
- Consult orthopedics first
- How to perform
- Place the joint in a comfortable position that allows access to the joint, allows you to see the injury and gives you the track you need to inject saline.
- Sterilize the skin with betadine or chlorhexidine.
- Inject 2-4 mL lidocaine 1-2% (+/- epi) opposite from the injury, tracking along the planned aspiration pathway.
- Prep a 60 mL syringe with STS and a 20 or 18g needle.
- Enter along anesthetized track and aspirate as you move. When in the joint, you’ll obtain synovial fluid.
- Inject lidocaine first, then slowly start injecting STS looking at the wound for saline coming out. You can range the joint which may help you see fluid extruding.
- Common operator errors
- Failing to enter joint capsule before injecting STS.
- Not injecting enough STS into the joint.
- Failing to see extravasation from the wound when it’s present (methylene blue has not been shown to improve sensitivity).
- Aborting the procedure if patients don’t tolerate it (consider procedural sedation).
- Joint specific recommendations for the SLT
- Knee
- Volume of injection plays a significant role in SLT sensitivity.
- Studies have shown that low volumes (50-60mL) injected have reported sensitivities of ~ 46% while higher volumes (190mL) found sensitivities of ~ 95%.
- Dynamic ROM during the SLT and has been found to increase sensitivity from 36% to 43% at volumes of 60mL.
- Elbow
- Higher volumes of injected saline can improve sensitivity
- In one study, a volume of 40mL achieved a sensitivity of 95% while 20mL only achieved a sensitivity of 72%. There was an improvement with dynamic ROM to 86%.
- Wrist
- Injection volumes 2.3-7mL achieve a sensitivity > 95%. One study found an increase in sensitivity with increasing volume. No reports on modification with dynamic ROM.
- Ankle
- Much greater variability amongst the reported results compared to other joints, with volumes required to achieve a sensitivity of at least 95% being between 10-55mL. There was a trend towards increased sensitivity with increasing volume. No study reported using dynamic ROM
- Shoulder
- One study found an injection volume of 81mL was necessary to achieve a sensitivity of 95%; there was an increase in sensitivity with increasing volume.
- Hip –There are no studies available that discuss the use of SLT at the hip.
- In pediatrics- consult orthopedics.
- Knee
Management in the ED
- Consult orthopedic specialist, provide analgesia, reduce fracture, irrigate if contaminated, splint the joint, and administer antibiotics and tetanus prophylaxis as needed
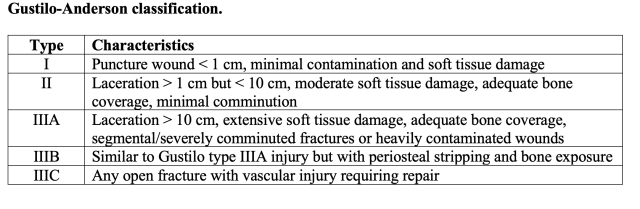
- Antibiotic options (based on Gustilo-Anderson classification):
- Small lacerations: first-generation cephalosporin (cefazolin)
- Extensive soft tissue damage: add gram-negative coverage with an extended spectrum penicillin (eg. piperacillin/tazobactam) or gentamicin.
- Risk factors for MRSA: add linezolid or vancomycin.
- Seawater involvement: use a 3rd-generation cephalosporin plus doxycycline to cover Vibrio vulnificus.
Summary:
- Traumatic arthrotomy (TA) can lead to significant morbidity and mortality when missed. Discuss the case with ortho in patients with high risk wounds.
- Plain x-rays can suggest TA when free air is seen in the joint space. Communicate the concern for TA to the radiologist prior to obtaining the radiograph.
- The saline load test (SLT) can be a sensitive test for identifying TA. However, it requires a significant volume of injected saline and is painful. Methylene blue is not necessary.
- CT shows promise in diagnosing TA of the knee but not other joints.
- Antibiotics should be administered to all suspected cases of TA.
References:
- Colmer HG 4th, et al. High risk and low prevalence diseases: Traumatic arthrotomy. Am J Emerg Med. 2022 Jan 21;54:41-45. PMID: 35121477.
- Voit GA, et al. Saline load test for penetration of periarticular lacerations. J Bone Joint Surg Br. 1996 Sep;78(5):732-3. PMID: 8836059.
- B. Sleasman, et al. Utility of conventional radiographs in the detection of traumatic knee arthrotomies: a retrospective cohort review. Curr Orthop Pract, 31 (5) (2020 Sept), pp. 479-482. Link.
- Konda SR, et al. The role of computed tomography in the assessment of open periarticular fractures associated with deep knee wounds. J Orthop Trauma. 2013 Sep;27(9):509-14. PMID: 23412508.
- Kongkatong M, et al. Can Ultrasound Identify Traumatic Knee Arthrotomy in a Cadaveric Model? J Emerg Med. 2019 Sep;57(3):362-366. PMID: 31375371.
- Kupchick TD, et al. Detection of traumatic elbow arthrotomies: computed tomography scan vs. saline load test. J Shoulder Elbow Surg. 2020 Sep;29(9):1869-1875. PMID: 32444316.
- Keese GR, et al. The accuracy of the saline load test in the diagnosis of traumatic knee arthrotomies. J Orthop Trauma. 2007 Aug;21(7):442-3. PMID: 17762473.
- Tornetta P 3rd, et al. How effective is a saline arthrogram for wounds around the knee? Clin Orthop Relat Res. 2008 Feb;466(2):432-5. PMID: 18196428.
- Feathers T, et al. Effectiveness of the saline load test in diagnosis of traumatic elbow arthrotomies. J Trauma. 2011 Nov;71(5):E110-3. PMID: 21768902.
- Gittings DJ, et alL. The Saline Load Test is Effective at Diagnosing Traumatic Arthrotomies of the Wrist. Tech Hand Up Extrem Surg. 2019 Jun;23(2):59-61.PMID: 30676429.
- Bohl DD, et al. Sensitivity of the Saline Load Test for Traumatic Arthrotomy of the Ankle With Ankle Arthroscopy Simulation. Foot Ankle Int. 2018 Jun;39(6):736-740. PMID: 29457483.
- Bohl DD, et al. Sensitivity of the Saline Load Test for Traumatic Arthrotomy of the Ankle With Ankle Arthroscopy Simulation. Foot Ankle Int. 2018 Jun;39(6):736-740. PMID: 29457483.
