Journal Feed Weekly Wrap-Up
- May 22nd, 2020
- Clay Smith
- categories:
We always work hard, but we may not have time to read through a bunch of journals. It’s time to learn smarter.
Originally published at JournalFeed, a site that provides daily or weekly literature updates.
Follow Dr. Clay Smith at @spoonfedEM, and sign up for email updates here.
#1: Move Over San Francisco – Canadian Syncope Score Validated
Spoon Feed
The Canadian Syncope Risk Score (CSRS) was successfully validated as a tool to risk stratify ED patients presenting with acute syncope. Patients at low risk for serious outcomes at 30 days can be safely discharged.
Why does this matter?
A patient presenting to the ED with syncope is often hospitalized unnecessarily when no obvious serious underlying condition is identified. This study is a prospective validation of the Canadian Syncope Risk Score which is a promising decision tool for emergency physicians confronted with determining patient risk for serious outcomes.
Disposition: Syncope
In this multicenter prospective cohort validation study performed in 9 Canadian EDs, patients age 16 and older presenting for syncope were enrolled and evaluated with CSRS. They excluded patients who had prolonged LOC (>5 minutes), witnessed seizure, mental status changes, head trauma causing LOC, major trauma, inability to provide a history, or another serious outcome identified prior to ED disposition. Through review of medical records, phone calls, and death records, patients were followed for 30 days for serious outcomes (i.e. death due to any cause, arrhythmic outcomes, and non-arrhythmic outcomes). Of the 3,819 patients, 139 (3.6%) had a serious outcome within 30 days. Only 3 (0.3%) out of 1,631 patients at very low risk and 9 (0.7%) of 1,254 patients at low risk experienced serious 30-day outcomes. None of those patients died or had ventricular arrhythmia. Comparatively, 19.2% of the high risk and 51.3% of the very high risk groups experienced serious 30-day outcomes. This risk stratification tool appears clinically useful in supporting ED disposition and may additionally be helpful in discussing risk estimates with patients during shared decision making in the ED.
Source
Multicenter Emergency Department Validation of the Canadian Syncope Risk Score. JAMA Intern Med. 2020 Mar 23. doi: 10.1001/jamainternmed.2020.0288. [Epub ahead of print]
Open in Read by QxMD
#2: Anorexia Nervosa – More Dangerous Than You Think
Spoon Feed
Anorexia nervosa (AN) is a common condition, with a high mortality rate. This will help you spot signs of severe illness, when to get labs and ECG, and when to admit.
Why does this matter?
A hallmark of this illness is the person is nonchalant about it. If you don’t know the danger signs, you may miss the severity on presentation, which could be a fatal error.
More dangerous than you think
AN is a common, severe psychiatric illness. It is often present with comorbid psychiatric illnesses. There is a high mortality rate, 5.6% per decade. It is notoriously difficult to treat with psychotherapy and pharmacotherapy. Most important for us in the ED is to recognize the danger signs and indications for immediate hospitalization.
History
-
Ask about weight trends, eating habits, food restriction, purging, fear of weight gain, excessive exercise, menstrual history (often amenorrhea), and syncope.
-
Ask others to corroborate focus on appearance, eating habits, fear of gaining weight, dissatisfaction with body shape, preoccupation with weight, and food intake.
-
Ask about suicidal ideation or depression.
Exam
-
Vitals: Take note of a BMI <16.5. Note the trajectory of weight loss as well. A rapid downward trend in weight is worrisome. A BMI ≤15 is often an indication for immediate admission. Look for orthostatic hypotension, bradycardia, and hypothermia. Note, patients will usually not become tachycardic, even if profoundly dehydrated.
-
Look for signs of dehydration, hair loss, presence of lanugo, erosion of dental enamel or salivary gland hypertrophy to indicate purging, or evidence of self harm.
Workup
-
If any concerns about severity, obtain labs and ECG.
-
Look for hyponatremia, hypokalemia, hypochloremia, hypomagnesemia, hypophosphatemia, and hypoalbuminemia.
-
On ECG, look for bradycardia, ectopy or other arrhythmias, and long QT interval.
Treatment
-
Be careful. Severity of illness is easy to overlook in these patients. They downplay most symptoms and are often not forthcoming with the severity of their own calorie restriction.
-
Some may need immediate hospitalization and refeeding. Indications may include: BMI ≤15, syncope, bradycardia, electrolyte abnormalities, concerning ECG findings, self harm, or suicidal ideation.
Source
Anorexia Nervosa. N Engl J Med. 2020 Apr 2;382(14):1343-1351. doi: 10.1056/NEJMcp1803175.
Open in Read by QxMD
#3: Differentiating STEMI from Pericarditis
Spoon Feed
While some overlap exists, ST elevation in lead III>II and ST segment depressions in various leads suggests STEMI, while PR depression and Spodick’s signs (downsloping T-P segment) are most suggestive of pericarditis.
Why does this matter?
In patients with chest pain and ST elevation, it is critical to differentiate between STEMI and pericarditis quickly in order to facilitate appropriate activation of the cath lab.
Cath lab or no cath lab?
This case-control study evaluated specific EKG findings in 207 patients with ST elevation and chest pain to determine changes associated with either STEMI or pericarditis (STEMI: n = 165, pericarditis: n = 42). The addressed EKG changes and results are in the table below.
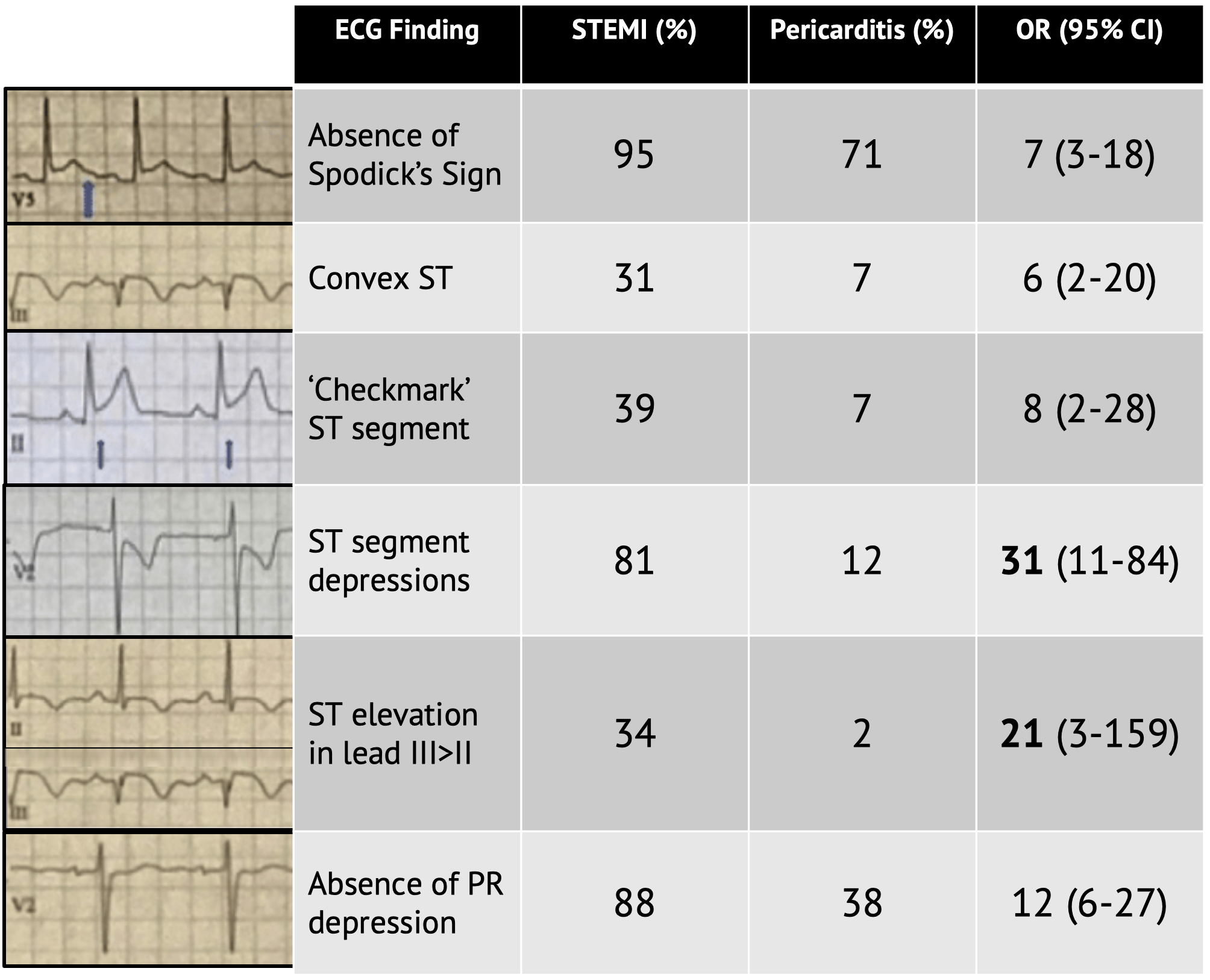
OR favors STEMI over pericarditis. ECGs from cited article. Table adapted from cited article.
In this study, the presence of ST segment depressions (in various leads, excluding aVR and V1) and ST elevation in lead III > II were the best discriminators pointing toward a diagnosis of STEMI. Presence of PR depression was the best discriminator pointing toward a diagnosis of pericarditis. However, PR depression was present in 12% of STEMIs, and Spodick’s sign was present in 5% of STEMI patients. In fact, every ECG finding had overlap between the two diagnoses.
This was a small, single-center study, but is an excellent review of some of the unique ECG findings associated with both STEMI and pericarditis. The big takeaway here is that there is no pathognomonic finding for either STEMI or pericarditis, and one should use caution before using a single finding to anchor on a diagnosis.
In his weekly ECG teaching series, senior author – Amal Mattu, recommends searching for signs to rule in STEMI on ECGs with ST elevation in the following steps before looking for any ECG changes associated with pericarditis:
-
Search for ST depression (aside from leads aVR and V1)
-
Look for ST elevation in lead III > II
-
Search for horizontal or convex upward ST elevation
Then, and only then, should you explore the other options for diagnosing pericarditis.
For more on pericarditis, see this EM@3AM and ECG Pointers.
Source
Evaluation of Spodick’s Sign and Other Electrocardiographic Findings as Indicators of STEMI and Pericarditis. J Emerg Med. 2020 Mar 25. pii: S0736-4679(20)30020-2. doi: 10.1016/j.jemermed.2020.01.017. [Epub ahead of print]
Open in Read by QxMD
