EM@3AM: Testicular/Scrotal Abscesses
- Nov 4th, 2023
- Jacob Kirkland
- categories:
Authors: Jacob Kirkland, MD (EM Resident Physician, UTSW – Dallas, TX); Steve Field, DO (Assistant Professor of EM/Attending Physician, UTSW – Dallas, TX) // Reviewed by: Sophia Görgens, MD (EM Fellow Physician, Zucker-Northwell NS/LIJ, NY); Cassandra Mackey, MD (Assistant Professor of Emergency Medicine, UMass Chan Medical School); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 54-year-old male with a history of diabetes presents with “pain in my groin” for the past two weeks. He reports approximately one month of dysuria, and around two weeks ago noticed a dull aching sensation in his testicles that has progressively gotten worse. He came to the ED because he now has a fever, chills, and nausea along with his testicular pain. An ultrasound of the testes reveals the following:

What is the diagnosis?
Answer: Testicular abscess
Epidemiology
- Abscesses limited to scrotal wall are similar to other abscesses on areas of the body
- Local trauma can increase risk of infection, normally start as progressive swelling of a small pustule2
- Staph aureus is the most common cause in spontaneous skin abscesses3,4
- Intrascrotal abscesses can occur as a result of persistent processus vaginalis5
- More likely seen in children after appendicitis6
- Abscesses of the testicle are usually secondary to severe, untreated epididymo-orchitis7
- Younger, sexually active adults are typically affected8,9
- Older population is also at risk
- 14-35 years old: sexually transmitted Neisseria gonorrhoeae or Chlamydia trachomatis10
- 35+ Escherichia coli, Klebsiella, Pseudomonas, Staphylococcus, and Streptococcus are more common and arise from urinary tract infections7
- Other risk factors include bladder outlet obstruction, urogenital malformation9
- In children, epididymo-orchitis more attributed to viruses such as enteroviruses and adenoviruses 10
- Mycoplasma pneumoniae is a potential bacterial cause in children10
- Mycobacterium tuberculosis in adults or children is a common cause of chronic epididymo-orchitis
- Younger, sexually active adults are typically affected8,9
Anatomy

- Simple scrotal abscesses are limited to the scrotal skin
- Processus vaginalis is a blind pouch that develops during early fetal growth and usually obliterates in early life
- During development connects peritoneal cavity and tunica vaginalis
- Persistence can lead to extension of intra-abdominal infections into the scrotum5
- Epididymo-orchitis result from retrograde spread of bacteria from urethra through vas deferens and into epididymis/testes
Clinical Presentation
Scrotal abscess
- General history of small pustule that increased in size over time2
- Pain, swelling, induration, fluctuance to the superficial layers of scrotum
- Simple isolated scrotal abscesses should not have systemic symptoms
Testicular abscess
- Severe pain and swelling of intrascrotal structures
- Slower onset of pain compared to testicular torsion12
- May present several days or weeks after urethral instrumentation introduced
- May have tachycardia, fever, chills, lower UTI symptoms or in tandem with prostatitis9
- Prostatitis may have similar symptoms of UTIs with dysuria, and frequent urination, however may additionally have lower back pain, pain with ejaculation
- Scrotal wall erythema may be present
- Cremasteric reflex is intact
Evaluation
- Differential diagnosis of an edematous, painful scrotum/testicles should include
- Scrotal/testicular abscess
- Cellulitis
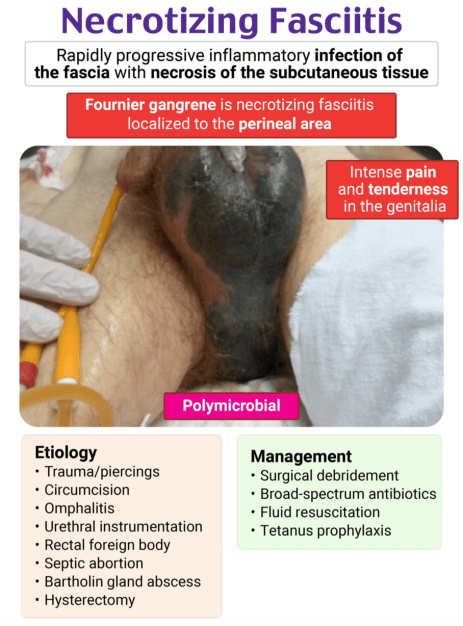
- Fournier gangrene
- Testicular torsion
- Epididymitis, orchitis
- Indirect inguinal
- Hernia
- Pyocele
- Scrotal abscess
- Ultrasound of suspected area
- Evaluate for septae, involvement of deeper structures, possible pyocele
Testicular abscess
- Urinalysis, urine culture, Nucleic Acid Amplification Test for Neisseria gonorrhoeae and Chlamydia Trachomatis9,12
- Ultrasound to evaluate for involved structures, presence of pyocele
- Abscesses will be ill-defined lesions, low echogenicity1,13
- Pyocele will show hypoechoic fluid in scrotum, possible septae or debris14
- Color Doppler will show hypervascularity in orchitis13
- CT imaging will show contrast enhancement/enlargement of affected testes1
Treatment

Scrotal abscesses
- Treatment is similar to other areas of cutaneous abscesses2
- Local anesthesia + incision/drainage
- Routine antibiotics are controversial
- Some studies show benefit with clindamycin and Trimethoprim/Sulfamethoxazole 15,16
- Sitz baths and frequent dressing changes17
- Consult urology for more complex abscesses, concern for Fournier gangrene
- Assess for erythema/edema extending to the perineum, necrotic tissue, crepitus, subcutaneous gas on CT imaging
Testicular abscesses
- Early consultation with urology as signs of acute scrotum may be a surgical emergency
- Surgical vs more conservative management with antibiotics1
- Surgical treatment may range from drainage to orchiectomy
- Antibiotic choice based on most likely organism
- Neisseria gonorrhoeae and Chlamydia trachomatis–Ceftriaxone + doxycycline9,18
- Enteric organisms–levofloxicin9,18
- Scrotal elevation, analgesia, and cooling may provide symptomatic relief 9,18
- Surgical vs more conservative management with antibiotics1
Disposition
Scrotal abscesses
- If simple abscess present, send home
- If immunocompromised or systemic symptoms present, admit for antibiotics/observation
- If more complex, or concern for Fournier gangrene, place early consultation with general surgery or urology
Testicular abscesses
- Admission for surgical intervention vs IV antibiotics and observation management
Pearls
- Testicular abscesses are usually secondary to severe/untreated epididymo-orchitis
- Ultrasound will show hypoechoic structures with possible debris and lack of color flow
- Early consultation with urology is needed for appropriate treatment
- Crepitus and involvement of perineum should be alarming for Fournier’s gangrene
- Use relief with scrotal elevation, cremasteric reflex, and flow on color doppler to differentiate between testicular torsion

A 55-year-old man presents with perineal pain. He has a long-standing history of hypertension and uncontrolled diabetes. He states 2 days ago, he noticed a “zit” and redness on his inguinal area and scrotum. He was seen by a different clinician yesterday, who started him on an antibiotic for cellulitis. Today the patient states the pain is worse, and he is now having fevers and chills. Vital signs are remarkable for a temperature of 39°C, HR 120 bpm, RR 23/min, BP 96/57 mm Hg, and SpO2 of 94%. Physical exam is remarkable for ecchymosis that extends from the medial right thigh and perineum to the right buttock. There is notable erythema with an indurated mass, patchy ecchymosis, and crepitus on palpation. Based on the presentation above, what is the best next step in management?
A) Administration of a 30 mL/kg bolus of normal saline
B) Admission for intravenous vancomycin
C) CT scan of the pelvis
D) Emergency surgical consultation and broad-spectrum antibiotics
Answer: D
Fournier gangrene is necrotizing fasciitis of the perineal, genital, or perianal anatomy. Often the process begins as a benign infection or simple abscess but quickly becomes virulent and results in microthrombosis of small subcutaneous vessels, leading to the development of gangrene of the overlying skin. Risk factors include diabetes and alcohol use disorder, as these result in an immunocompromised host, with male patients being most commonly affected. Early in the disease course, patients may complain of genital pain or perineal pain, often with associated pruritus. As the disease progresses, the pain may improve or completely resolve due to nerve damage or death. Crepitus and ecchymosis can occur, or the area may appear benign.
Diagnosis is often clinical as no lab study is sufficient to make the diagnosis. A high index of suspicion is required to prevent a delay in diagnosis. Treatment consists of emergency surgical consultation for debridement and broad–spectrum antibiotics, such as piperacillin-tazobactam, imipenem, or meropenem with vancomycin. Clindamycin is another agent that should be given as it helps reduce toxin formation.
Even though establishing IV access and administering a 30 mL/kg bolus (A) will likely be a part of the patient’s management, these are not the best next steps in management. Emergent surgical consultation is warranted to ultimately treat the disease process.
Admission for intravenous vancomycin (B) would be appropriate management for failed outpatient treatment of cellulitis. However, this patient has findings concerning for necrotizing fasciitis requiring surgical debridement and broad-spectrum antibiotics.
Imaging should not delay emergent surgical consultation. A CT scan of the pelvis (C) will often identify the disease, but MRI has the highest sensitivity. This is not required, however, and the best next step in management should be emergency surgical consultation and empiric antibiotics.
References
- Avery LL, Scheinfeld MH. Imaging of penile and scrotal emergencies. Radiographics. 2013;33(3):721-740. doi:10.1148/rg.333125158
- Moore, S and Ryan Pedigo. Scrotal Abscess. In: Knoop KJ, Stack LB, Storrow AB, Thurman R. eds. The Atlas of Emergency Medicine, 5e. McGraw Hill; 2021. Accessed April 26, 2023. https://accessmedicine-mhmedicalcom.foyer.swmed.edu/content.aspx?bookid =2969§ionid=250456991
- Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666-674. doi:10.1056/NEJMoa055356
- Breyre A, Frazee BW. Skin and Soft Tissue Infections in the Emergency Department. Emerg Med Clin North Am. 2018;36(4):723-750. doi:10.1016/j.emc.2018.06.005
- Kamei J, Kuriyama A. Scrotal Abscess. JMA J. 2021;4(4):426-427.
- Saleem MM. Scrotal abscess as a complication of perforated appendicitis: A case report and review of the literature. Cases J. 2008;1(1):165. Published 2008 Sep 19. doi:10.1186/1757-1626-1-165
- Hackett B, Sletten Z, Bridwell R E (July 03, 2020) Testicular Abscess and Ischemia Secondary to Epididymo-orchitis. Cureus 12(7): e8991. doi:10.7759/cureus.8991
- Schlossberg D. Clinical Infectious Disease. Cambridge Univ Pr. (2008) ISBN:0521871123.
- Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009;79(7):583-587.
- Tracy CR, Steers WD, Costabile R. Diagnosis and management of epididymitis. Urol Clin North Am. 2008;35(1):101-vii. doi:10.1016/j.ucl.2007.09.013
- Adhikari, L. Testicular. Radiology Key. December 27, 2016. Accessed May 2, 2023. https://radiologykey.com/testicular
- Wampler SM, Llanes M. Common scrotal and testicular problems. Prim Care. 2010;37(3):613-x. doi:10.1016/j.pop.2010.04.009
- Tonolini M, Ippolito S. Cross-sectional imaging of complicated urinary infections affecting the lower tract and male genital organs. Insights Imaging. 2016;7(5):689-711. doi:10.1007/s13244-016-0503-8
- Bruner DI, Ventura EL, Devlin JJ. Scrotal pyocele: Uncommon urologic emergency. J Emerg Trauma Shock. 2012;5(2):206. doi:10.4103/0974-2700.96504
- Talan DA, Mower WR, Krishnadasan A, et al. Trimethoprim-Sulfamethoxazole versus Placebo for Uncomplicated Skin Abscess. N Engl J Med. 2016;374(9):823-832. doi:10.1056/NEJMoa1507476
- Daum RS, Miller LG, Immergluck L, et al. A Placebo-Controlled Trial of Antibiotics for Smaller Skin Abscesses. N Engl J Med. 2017;376(26):2545-2555. doi:10.1056/NEJMoa1607033
- Schmitz GR, Gottlieb M. Managing a Cutaneous Abscess in the Emergency Department. Ann Emerg Med. 2021;78(1):44-48. doi:10.1016/j.annemergmed.2020.12.003
- Manavi K, Turner K, Scott GR, Stewart LH. Audit on the management of epididymo-orchitis by the Department of Urology in Edinburgh. Int J STD AIDS. 2005;16(5):386-387. doi:10.1258/0956462053888853
